Apoptosis
advertisement

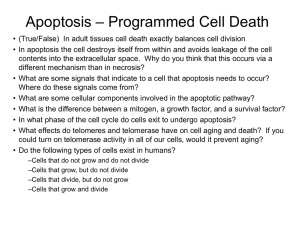
Adaptation, Injury and Death (Part 2) Tom Davis 8-14-14 Lecture 3 Learning Objectives • 1. List characteristics of apoptosis and necrosis • 2. Diagram the intrinsic and extrinsic pathways of apoptosis • 3. Diagram the mechanism of some antineoplastic drugs that exert their effect via apoptosis • 4. List 4 types of intracellular accumulations and describe the associated pathology Mechanisms of Cell Death • Necrosis- groups of cells are killed by injurious agents • Apoptosis- individual cells are induced to commit suicide Apoptosis • • • • ATP-dependent Cell membrane intact Organelles intact No inflammation (macrophages ingest apoptotic bodies) Necrosis • • • • ATP not required Cell membrane rupture Organelles rupture Inflammation (neutrophils) NECROSIS NECROSIS APOPTOSIS APOPTOSIS Apoptosis Morphology • Cell shrinkage • Chromatic condensation • Plasma membrane wrinkles/blebs • Fragmentation into apoptotic bodies • Phagocytosis of apoptotic cells/bodies Apoptotic Cells in H & E Sections • Oval mass of intensely eosinophilic cytoplasm with dense chromatin fragments; occurs rapidly; no inflammation CIVATTE BODIES Civatte Bodies PHYSIOLOGIC APOPTOSIS • Embryology- fingers and toes/maleness • Hormone-dependent- endometrial cells shed on estrogen withdrawel; breast duct regression after weaning • Neutrophils (PMNs) disappear in acute inflammation • Cytotoxic T cells eliminate virusinfected cells Apoptosis of Neutrophils PATHOLOGIC APOPTOSIS • Radiation and anticancer drugs damage DNA and apoptosis follows ( p53 expression) • Hypoxia- apoptosis (if mild) or necrosis if the hypoxia is severe or prolonged • Decreased cell death in lymphomas (Bcl-2 overexpression) • Misfolded proteins Apoptosis after Radiation Pathologic Apoptosis in Viral Infections • HPV- E6 protein inactivates p53 • EBV- Bcl-2-like substance produced • HIV- infected cells make high levels of FasL which will induce apoptosis in HIVuninfected Tcells Biochemical Events in Apoptosis • Caspases (cysteine proteases) cleave the cytoskeleton and activate DNAses and other enzymes • DNA breaks into 50- to 300-kilobase pieces; further broken into multiples of 200 base pairs by endonucleases (Ca++ and Mg++)- demonstrated as a “ladder pattern” on agarose gel; also proteases. • Phosphatidylserine is exposed and attracts macrophages with little “collateral damage” The intrinsic Pathway • Major mechanism • Increased mitochondrial permeability and release of pro-apoptotic molecules (cytochrome c) • Pro: 1. membrane- Bim, Bid, Bad and Bax, Bak 2. cytoplasm- Smac/DIABLO • Anti: Bcl-2, Bcl-x Extrinsic Pathway • Activation of plasma membrane death receptors • TNFR1 and Fas Control and Integration Stage Specific proteins connect the “death signals” to proteolytic enzymes in the capase family responsible for “the execution phase”. The Execution Stage Caspases cleave cytoskeletal and nuclear matrix proteins and result in DNA cleavage into fragments giving “DNA Ladder pattern” by agarose gel electrophoresis. A. B. C. Normal cells Apoptosis Necrosis Removal of Apoptotic Bodies Apoptotic cells are coated by Phosphatidyl serine (which “flips out”) or C1q leading to early recognition and removal by macrophages. Thrombospondin is an adhesive glycoprotein. DNA-damage and Apoptosis • • • • Radiation or chemotherapy damages DNA p53 accumulates Cell cycle arrested at G1 (allows repair) If repair fails, p53 triggers apoptosis Tumor Necrosis Factor and Cytotoxic Lymphocytes in Apoptosis • Fas (CD95) –FasL induces apoptosis in lymphocytes that recognize “self”; Fas/FasL mutations may cause autoimmune disease • TNF/TNFR1-TRADD-FADD causes caspase activation and APOPTOSIS; TNF also activates NF-kB which aids cell SURVIVAL and is antiapoptotic • Foreign Ag-CTLs- lymphocytes produce PERFORMIN which allows entry of GRANZYME which activates caspases; CTLs kill target cells Dysregulated Apoptosis “Too little” activity diminished in certain cancers (p53 mutations in solid tumors) “Too much” neurodegenerative diseases, ischemic injury, virus-induced lymphocyte depletion Defective Apoptosis • 50% of human cancers have p53 mutations • Hormone-dependent tumors (breast, prostate) • Follicular lymphomas and colon cancers express high levels of Bcl-2 (translocation of bcl-2 gene) • HPV- protein E6 binds and inactivates p53 • EBV- proteins that mimic or increase production of Bbcl-2 • Autoimmune disorders Increased Apoptosis • • • • • • Neurodegenerative diseases Ischemic injury Death of virus-infected cells (hepatitis) AIDS (death of uninfected CD4 cells) FasL+ tumors are MORE aggressive Microorganisms induce apoptosis Example of Pneumocystis pneumonia • Pneumocystis causes pneumonia in AIDS • Human macrophages are killed before they can engulf the organisms • Apoptosis is triggered in macrophages by polyamines • Pneumocytis is not phagocytosed Apoptosis Summary • Normal part of the cellular machinery • Pathology results when it is increased or decreased • Future Study of Apoptosis: inflammation and repair (cell signaling); immune system; neoplasia; infectious diseases • Future targets for new chemotherapeutic and antimicrobial agents Clinical Applications • Velcade (bortezomid)- blocks proteasomes in multiple myeloma; proteins accumulate which are toxic to myeloma cells; also activates p53 and apoptosis of malignant plasma cells • Genasense (oblimersen)- blocks production of BCL-2 in lymphomas rendering them more susceptible to other anticancer drugs Subcellular response to Injury • Primary lysosome- hydrolytic enzymes • Lysosome/vacuole fusion- secondary lysosome or phagolysosome • Heterophagy • Autophagy • Others- lipids, proteins, filaments, Ca++ Cytoskeletal Abnormalities • • • • Microtubules- 25 nm Actin filaments (thin)- 8 nm Myosin filaments (thick)- 15 nm Intermediate- 10 nm Abnormal Microtubules • Sperm motility deficiency “YBCS syndrome” • Immotile cilia syndrome (Kartagener’s Syndrome) • Colchicine- disrupt microtubule formation and inhibit PMN migration; gout therapy • Vinca alkaloids- antitumor; disrupt the mitotic spindle Intermediate Filaments (IM) • Mallory bodies (alcoholic hyalin)- keratin IM • Neurofibrillary tangles- neurofilament IM seen in Alzheimer’s Disease Mallory Hyaline Neurofibrillary tangles Intracellular Accumulations • 1. Normal substance that cannot be metabolized- fatty liver (triglyceride) • 2. Genetic defect in metabolism of a substance (alpha-1-antitrypsin deficiency and “storage diseases” like Gaucher’s) • 3. No normal enzymes to degrade an abnormal substance (silica-silicosis) Fatty Change (Steatosis) • Triglycerides accumulates in parenchymal cells • Alcoholism, protein malnutrition, anoxia Oil Red O Stain Gaucher’s Disease in Spleen Cerebroside in Gaucher’s Disease Silica in silicosis (polarized view) Cholesterol Accumulation • Atherosclerosis- smooth muscle cells and macrophages (foam cells) Foam Cells in Atherosclerosis Protein Accumulation • Renal failure- reabsorption of filtered protein in the proximal tubule accelerates • Vesicles of protein fuse with lysosomes and appear as pink hyalin droplets in the tubules Protein in Renal tubules Protein Folding Errors (failure of chaperones) • • • • Alpha-1-antitrypsin deficiency Cystic fibrosis Familial hypercholesterolemia Unfolded Protein Response- caspase-12 is activated with apoptosis induction; Alzheimer’s, Huntington’s, Parkinson’s • Amyloidosis- amyloid not eliminated Hyaline change • Homogenous, glassy, pink appearance • Eg. Mallory alcoholic hyalin Hyaline Change in Hypertension Pigments • Carbon (exogenous) • Lipofuscin- lipid and phospholipid polymers complexed with protein; wear-and-tear pigmentliver and heart of aging patients • Melanin- dihydroxyphenylalanine (from Tyr) • Hemosiderin- iron-ferritin forms hemosiderin granules; hemosiderosis (in macrophages); hemochromatosis (in parenchymal cells) Lipofuscin Iron/hemosiderin Prussian blue Stain Pathologic Calcification • Dystrophic- necrotic tissue; serum Ca++ normal; atheromas, heart valves; psammoma body/asbestos body • Metastatic- hypercalcemia; parathyroid, skeletal metastases, vitamin D, renal failure; lungs, arteries Calcified heart valve Dystrophic Calcification Psammoma Body Asbestos Bodies Metastatic Calcification in lung Cellular Aging • DNA damage • Replicative senescence – progressive shortening of telomeres • Defective protein homeostasis – impaired chaperone and proteasome functions • Nutrient sensing system – caloric restriction increases longevity