first aid safety briefing
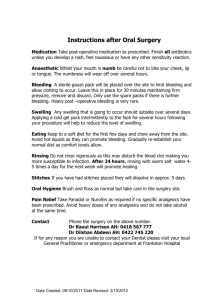
advertisement

• • • • • Equipment Medical Release Forms First aid supplies Baseball injuries 911 User Manual • • Catchers Gear BPF 1.15 • On ALL Website under General Info tab on the left • Consider adding insurance company name and medical record number • Dentist 24/7 emergency contact information? Located at Fields Icepacks Save-A- Tooth 4x4s Ace bandage Band-Aids Tape Non-latex powder free examination gloves • Ziploc bags for ice from coolers • Antiseptic Wipes • • • • • • • • Infectious Germs Carried in the Blood i.e. Hepatitis B&C and HIV • Can be Transmitted Through Contact Via Cuts, Abrasions and Mucous Membranes • What is MRSA (Methicillin-resistant Staphylococcus Aureus or a “Staph” bacteria resistant to antibiotics • Follow Standard Precautions & Hand washing – Treat all blood, body fluids, secretions, excretions (except sweat), regardless of whether or not they contain visible blood, nonintact skin and mucous membranes as if contaminated with a blood borne pathogen – Wash your hands often! Wash after removing gloves, before & after contact with body fluids • Wipe Up Blood Spills – Use Exam Gloves – Clean up with a 10% bleach solution or disinfectant • • • • • • • • Head and neck Knee / ankle Hand / fingers Eye Teeth Abrasions/ bruises/lacerations Muscle Heat Related CPR IN THREE SIMPLE STEPS 1. CALL Check the victim for unresponsiveness. If there is no response, Call 911 and return to the victim. In most locations the emergency dispatcher can assist you with CPR instructions. 2. BLOW Tilt the head back and listen for breathing. If not breathing normally, pinch nose and cover the mouth with yours and blow until you see the chest rise. Give 2 breaths. Each breath should take 1 second. 3. PUMP If the victim is still not breathing normally, coughing or moving, begin chest compressions. Push down on the chest 2 inches 30 times right between the nipples. Pump at the rate of 100/minute, faster than once per second. CONTINUE WITH 2 BREATHS AND 30 PUMPS UNTIL HELP ARRIVES HANDS-ONLY CPR This method of CPR was recommended by the AHA in 2010. It is intended for bystanders untrained in CPR. It is also recommended for situations when the rescuer is unable or unwilling to provide mouth-tomouth ventilations.. • Make sure Athletes are well hydrated with water or sports drinks • Managers are responsible for making sure water is provided • IF YOU SUSPECT A NECK OR BACK INJURY YOU MUST KEEP THE NECK AND/OR BACK PERFECTLY STILL UNTIL AN EMERGENCY CREW ARRIVES. DO NOT MOVE SOMEONE WITH A SUSPECTED NECK OR SPINE INJURY UNLESS THE PERSON MUST BE MOVED BECAUSE HIS OR HER SAFETY IS IN DANGER. ANY MOVEMENT OF THE HEAD, NECK OR BACK COULD RESULT IN PARALYSIS OR DEATH. IMMOBILIZE THE NECK BY HOLDING THE HEAD, NECK AND SHOULDERS PERFECTLY STILL. USE BOTH HANDS, ONE ON EACH SIDE OF THE HEAD. Fractures & Dislocations Must treat for bleeding first Do not push bones back into place Don’t straighten break Dislocations The most common dislocations occur in the shoulder, elbow, finger, or thumb. LOOK FOR THESE SIGNS: 1. swelling 2. deformed look 3. pain and tenderness 4. possible discoloration of the affected area IF A DISLOCATION IS SUSPECTED... 1. Immobilize the joint to keep it from moving. 2. Try to keep joint elevated to slow blood flow to the area 3. A doctor should be contacted to have the bone set back into its socket. SIGNS OF FRACTURES It is often difficult to tell whether a child's bone is broken. If you suspect a broken bone, treat it accordingly even if it looks normal. Signs to look for: • A piece of bone protruding from a wound • The child is unable to move the injured part. • Swelling or deformity of the injured limb or body part • Pain • Possible signs of shock • History – Did they feel a ‘pop’ or ‘snap’? – Can they walk? – Has there been a prior injury to the knee? • What to look for? – Swelling – Deformity • Immediate swelling, severe pain • Inability to bear weight • Hearing a “pop” • Treat the mind • • Use calming techniques. Acknowledging that child is in pain diminishes anxiety. Tell child you will do something about pain once you make sure nothing else more serious is going on. Ice • • • • • Critical to the care of somatic pain Constricts blood supply, decreasing swelling Decreases production of inflammatory chemicals Stimulates opioid receptors causing local numbing Do not put directly on skin to avoid tissue damage • Immobilization the effected area • • • Reduces pain by limited movement Should immobilize joints above and below injury Analgesics administered by parents or with permission from parents (No ASPIRIN) • • • Opioids Ibuprofen Acetaminophen • • • • Stop bleeding Ice Splint in position of comfort Seek medical treatment (X-ray) There are three classifications of bleeding. 1. Capillary- Capillary bleeding is slow, the blood "oozes" from the (wound) cut. 2. Venous- Venous bleeding is dark red or maroon, the blood flows in a steady stream. 3. Arterial- Arterial bleeding is bright red, the blood "spurts" from the wound. Arterial bleeding is life threatening and difficult to control. There are three methods to control bleeding: 1. direct pressure 2. elevation 3. indirect pressure. 1. Direct Pressure: – Place a sterile dressing or clean cloth on the wound, tie a knot or adhere tape directly over the wound, only tight enough to control bleeding. If bleeding is not controlled, apply another dressing over the first or apply direct pressure with your hand or fingers over the wound... 2. Elevation: – Raising (elevation) of an injured arm or leg (extremity) above the level of the heart will help control bleeding. Elevation should be used together with direct pressure. • Penetrating Objects – DO NOT remove the object. Stabilize the object by using bulky dressing around the object and secure it in place. Children with Asthma need to have inhalers on-hand • Scrape the stinger out from the stung area -- never squeeze or pull out the stinger. • Persons with severe allergic reactions to insect stings should consider wearing a medical ID bracelet and carrying an insect allergy kit where appropriate. • Apply ice to reduce the swelling • Do not scratchy the sting site. • Allergic reactions to bee stings can be deadly. People with known allergies to insect stings should always carry an insect sting allergy kit and wear a medical ID bracelet • There are several signs of an allergic reaction to bee stings. Look for swelling that moves to other parts of the body, especially the face or neck. Check for difficulty in breathing, wheezing, or dizziness Get the person immediate medical care if any of these signs are present. How to Use an EpiPens EpiPens Remove the device from the plastic protective container. Remove the grey cap from the fatter end of the device. NB: This "arms the unit" ready for use Hold the EpiPen in your fist with clenched fingers wrapped around it (NB: there is nothing to "push" at the white end) Press the black tip gently against the skin of the mid thigh, then start to push harder until a loud "click" is heard. This means that the device has been activated. Hold in place for 10-15 seconds. • Basketball and baseball cause the most eye injuries, followed by water sports and racquet sports. • First-aid for physical trauma to the eye: • • • • Gently apply small cold compresses without pressure immediately to reduce pain and swelling. Do not attempt to treat severe blunt trauma or penetrating injuries to the eye. Tape a paper or Styrofoam cup over the injured eye (cover both eyes) to protect it until proper care can be obtained. In the case of a blow to the eye, do not assume the injury is minor. The eye should be examined thoroughly by an ophthalmologist because visionthreatening damage could be hidden. First aid is only the first step for emergency treatment. If you experience pain, impaired vision, or any possibility of eye damage, call your ophthalmologist or go the emergency room immediately. DENTAL TRAUMA • 5 million teeth are knocked out each year? The roots of a knocked out tooth will start to die within fifteen minutes, making it impossible to save the tooth? When you or your child knock out a tooth, What will you do? • Save-A-Tooth® allows you to be ready for a knocked-out tooth emergency. It gives you 24 hours to get treatment vs. 15 minutes and can save on costly dental work. • It has a 2-year shelf life and is relatively inexpensive. Hold the tooth by the crown and rinse off the root of the tooth in water if it’s dirty. Do not scrub it or remove any attached tissue fragments. If possible, gently insert and hold the tooth in its socket. • • • Most minor wounds stop bleeding on their own. If bleeding continues, apply pressure to the wound with a clean bandage. Wash the skin around the wound with soap and water. Hold the wound under running water to remove dirt. Pat the wound dry with sterile gauze and apply antiseptic ointment. In the case of cuts, close the wound with sterile adhesive wound closure strips. If strips are not available, cover the wound with clean gauze and adhesive tape. Adhesive nonadherent bandages can be used for abrasions that continue to ooze blood. • When stitches are required • If a wound doesn't close easily, the wound is deep (more than 0.6cm), gaping or jagged-edged, you may need stitches to promote healing, prevent infection and minimize scarring. Stitches are often necessary in small children as they tend to remove dressings, or if the cut is on the face or hands or joints. Stitching should be done within eight hours. FIRST AID Merit Badge • Heat Illness can be defined as inability of normal regulatory mechanisms to cope with a heat stress • Very prevalent, so one must understand the normal temperature regulatory mechanism and abnormal variations from it • If unrecognized and untreated, has high morbidity – In athletes, heat stroke is second only to head and c-spine injuries as cause of death – Not all forms of heat-related illness require emergent treatment • Person’s level of acclimatization – Process of becoming physically adjusted to environment • Length and intensity of exposure • The young and old are at most risk – Unable to remove themselves from the hot environment • Environmental factors – Humidity, sun, wind • Heat cramps – Painful spasms of heavily used muscle groups caused by excessive sodium and water loss – Caused by strenuously activity in a hot environment with insufficient (water) rehydration – May feel dizzy or faint • Treatment • Remove person from heat – place in cool shaded area or AC • Treat with fluid and electrolyte replacement • Water depletion Thirst Weakness Dizziness Poor muscular coordination – Agitation – Palpitations – – – – • Salt depletion – – – – – – – Fatigue Weakness Headache Anorexia Vomiting Skeletal muscle cramps Absent thirst • Treatment: – Remove from heat • Cool, shaded area or air conditioning – Remove some clothing and fan patient • Avoid chilling patient to point of shivering – Rehydration with IV (oral if mild) normal saline • May require up to 4L or more • Without termination of heat stressor and immediate treatment, symptoms may progress to heat stroke • True medical emergency!! • Temperature regulatory mechanism in brain is lost leading to cell death and damage to brain, lever, kidneys • Core temperature at which heatstroke begins – Generally characterized by body temp of at least 105°F • Mortality of up to 70% Warning signs of heat stroke vary but may include the following: •An extremely high body temperature (above 103°F, orally) •Red, hot, and dry skin (no sweating) •Rapid, strong pulse •Throbbing headache •Dizziness •Nausea •Confusion •Unconsciousness If you see any of these signs, you may be dealing with a lifethreatening emergency. Have someone call for immediate medical assistance while you begin cooling the person. Do the following: • Get the person to a shady area. • Cool the person rapidly using whatever methods you can. For example, immerse the person in a tub of cool water; place the person in a cool shower; spray them with cool water from a garden hose; sponge the person with cool water; or if the humidity is low, wrap them in a cool, wet sheet and fan them vigorously. • Monitor body temperature, and continue cooling efforts until the body temperature drops to 101102°F. • If emergency medical personnel are delayed, call the hospital emergency room for further instructions. Definition A seizure may be mild and cause minimal symptoms or may be severe and cause loss of consciousness and a sudden, violent contraction and relaxation of the muscles caused by spontaneous electrical activity in the brain. Most seizures last from 30 seconds to 2 minutes. However, if a seizure is prolonged, or if multiple seizures happen in succession with no recovery of consciousness in between, this is a medical emergency. • When a seizure occurs, the main strategy is to try to prevent injury. Try to protect the person from falls. Lay the person on the ground in a safe area. Clear the area around the person of furniture or other sharp objects. • If the person requires restraint, place him on his side. • If vomiting occurs, try to turn the head so that the vomitus is expelled and is not inhaled into the lungs or windpipe. • Known epileptics should always take any prescribed medication and wear a medical alert tag. • Some statistics – Nearly 8 million lightning flashes every day worldwide – Approximately 150-300 lightning-related fatalities per year in US • 3rd most common cause of death from isolated environmental phenomena – 100 out of every 500 electricity related fatalities are result of lightning strikes – Fatality rate 25-32% • 74% experience permanent injury • Clear the field, dugouts and stands immediately when you hear thunder or see lightning • Retreat to cars or suitable shelter • Wait at least 30 minutes before returning after the last rumble of thunder or lightning • Cars with players shouldn’t leave the park until the game has been officially called by the umpires • Have a plan! • Inspect the fields prior to each game • Discuss safety at he plate conference • Confirm location of first aid kit Alexandria Little League Baseball League ID- 76332 2014 Season Safety Plan Mission Statement: The Alexandria League Safety Program is designed to get everyone involved in safety; promote an aggressive program that will reduce the risk of safety related accidents and ensure a fun experience for everyone. Safety Code: Dedicated to Safe Play and Injury Prevention. Emergency/League Official Phone Numbers City Police-Emergency......................................................................911 Alexandria Police Non-Emergency……..………………703-838-4444 Alexandria Little League Main Number……..…………703-739-4444 League President - Stephen Frerichs……………………703-212-9416 League Safety Officer -Saul Grosser……………………240-398-6852 District Administrator - Ellen Witherow………………..571-259-3901 League Safety Officer Every league shall appoint or elect a league safety officer (LSO). It is encouraged that the LSO recruit assistance to help maintain a steady focus. The LSO shall maintain a complete set of emergency phone numbers that should be distributed to all concerned. The LSO will review the league constitution, by laws, rules and policies for: • Description of his/her duties • Safety rules already adopted • Safety history • League safety plan Alexandria Little League Safety Plan Emergency Contacts under n General Information Tab E A ALL Website So what happens when you call 911? • When you call from a cell phone you may be connected with a call center other than Alexandria VA! – Could be DC, FFX, or Arlington for example – Don’t worry they’ll transfer the call to the incident jurisdiction • You’ll be asked a series of questions by the call taker – Such as type of emergency (Fire/EMS) • Location / commonplace name / address – Simpson Field, field number, best access? • Describe injured / injury – Breathing / not breathing, head injury, adult / child / fracture / bleeding • Appropriate emergency equipment and personnel will be dispatched based on information obtained • Emergency responders may be from AFD, WMAA, ACFD, and / or FFX etc. – May also include one or more Ambulance, Medic Unit, EMS Supervisor, Engine, Paramedic Engine, Helicopter • Patient may be transported to Inova Alexandria, GWU, Children's Hospital National Medical Center, Inova Fairfax Hospital, Virginia Hospital Center • Transport hospital depends on type of injury and hospital status – Throughout the day hospital emergency departments go on bypass for two hours and do not accept patients • Have one or more people treat the patient • Have someone else call 911 • Have another person or persons direct the emergency responders • Contact the patient’s parent / guardian after you have something to tell them – Matt’s OK, he may have broken his arm, and was transported by Medic Unit to Inova Alexandria Hospital THE END