Role of Metabolism in Nutrition
advertisement

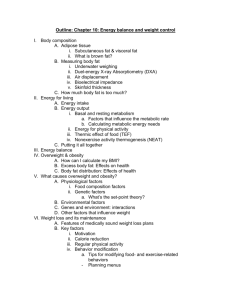
Lesson 2 : Role of Metabolism in Nutrition Metabolism • Metabolism – process by which living systems acquire and use free energy to carry out vital processes • Catabolism (degradation) – Nutrients and cell constituents are broken down for salvage and/or generation of energy – Exergonic oxidation • Anabolism (biosynthesis) – Endergonic synthesis of biological molecules from simpler precursors – Coupled to exergonic processes through “high-energy” compounds Role of Metabolism in Nutrition Definition: the sum of all biochemical changes that take place in a living organism. Group these reactions into two types: anabolic catabolic Reactions: require energy release energy Produce: more simple compounds more complex compounds Modus Operandi: Occurs in small steps, each of which is controlled by specific enzymes. Relationship Between Catabolic and Anabolic Pathways • Catabolic pathways – Complex metabolites are transformed into simpler products – Energy released is conserved by the synthesis of ATP or NADPH • Anabolic pathways – Complex metabolites are made from simple precursors – Energy-rich molecules are used to promote these reactions Examples of each type of metabolism: Anabolic Pathways Protein Biosynthesis Glycogenesis Gluconeogenesis Fatty Acid Synthesis Catabolic Pathways ATP Generated FOR Provides Energy Glycolysis TCA (Krebs cycle) ß-oxidation Respiratory Chain Other useful generalizations: Some of the steps in the anabolic path (going “uphill”) may not be identical to the catabolic path--but some are shared. Metabolism: Who Needs It? Average American consumes ~ 1450 lbs ( 600kg) of food each year. Assuming that 98.2% of this energy is metabolizable, 1424 lbs ( 590kg) is used to supply our needs. Supplies roughly 1 x 106 kcals/ year Energy needs Measurement of Energy Intake Diet Surveys • Dietary and nutritional survey of British Adults (Gregory 1990) • Average UK dietary energy intake • Men 10.2 MJ (2400 kcal/d) • Women 7.02MJ (1650 kcal/d) How do we employ energy? • MECHANICAL- muscle contraction • ELECTRICAL- maintaining ionic gradients (e.g., Na-K ATPase; 70% of ATP used by kidney & brain used to maintain gradient) • CHEMICAL- biotransformation of molecules (e.g., synthesis degradation, metabolism) International Unit of Energy: Joule : energy used when 1 Kg is moved 1 meter by a force of 1 Newton : kJ = 103 J; MJ = 106 J : 1 kcal = 4.184 kJ : Protein: CHO: Fat: 17 kJ or 4 kcal/g 17 kJ or 4 kcal/g 37 kJ or 9 kcal/g Energy needs Measurement of Energy Intake Metabolic Energy Yields Fuel KJ/g Kcal/g Fat 38 9 Alcohol 29 7 Carbohydrates 17 4 Protein 4 16 Average Energy Needs: European text: American Biochem text: 100 kJ/ day x BW in kg or 24 kcal/day x BW in kg 129-184 kJ/ kg or 31-44 kcal/kg Conversion Efficiency: Food to Usable Energy 40% used to make high energy phosphate bonds 60% “lost” (?) as heat How to measure energy in food • Direct Calorimetry – Direct measurement of heat produced – Bomb calorimeter • Calculate – Calories/g: 4 (cho), 9 (fat) ,4 (prt) and 7 (alcohol) – based: lab analysis of food composition • Calorie chart or nutrient database Energy needs Measurement of Energy Intake Bomb Calorimeter • Food is ignited electrically in the presence of oxygen • Heat of combustion is measured from a rise in water temperature Bomb Calorimeter measures heat produced when food is burned Text view of bomb calorimeter Energy needs Measurement of Energy Intake Bomb Calorimeter • Heat of combustion represents the gross energy of the food • Energy lost during digestion and absorption • Affected by illness Energy needs Measurement of Energy Intake % Energy from carbohydrates, protein and fat Food Total energy % Energy content of from serving (kJ) carbohydrate % Energy from protein % Energy from fat Chocolate 1195 43 6 51 Peas 230 47 35 18 Chicken Breast 1138 0 75 24 Potato boiled 535 89 10 1 Energy Balance: Input vs Output Energy Balance • Energy In = Energy Out – Weight Maintenance • Energy In > Energy Out – Weight Gain • Energy In < Energy Out – Weight Loss Energy Balance • Sources of fuel for energy – Input from diet: carbs, fat, prot, alcohol – Stored energy: glycogen, fat, muscle • Energy outgo from: – Basal metabolism – Physical activity – “Dietary thermogenesis” Energy In • Food and Beverages – Food composition tables – Bomb Calorimetry • Complex social, environmental, physiological control Energy Out • Energy of food = Body Energy = ATP – Overall efficiency 25%, 75% released heat • Energy out: • 3 main components: – Basal Metabolic Rate – Thermic Effect Food – Physical activity BMR > Activity > Dietary Thermogenesis Energy needs Measurement of Energy Output Energy Output Energy of food • 50% efficiency ATP + Heat Loss ATP • 50% efficiency “Work “+ Heat Loss “Work “ Heat Energy needs Measurement of Energy Output Energy Output Measurement of heat • Two methods • direct calorimetry • indirect calorimetry Measurement of energy used Energy needs Measurement of Energy Output direct calorimetry • Measurement of heat loss Energy needs Measurement of Energy Output Indirect calorimetry • Utilisation of oxygen • Oxygen consumption is proportional to ATP synthesis • Use oxygen consumption to determine heat production Energy needs Measurement of Energy Output Indirect calorimetry • Glucose oxidation C6H12O6 + 6O2 6H2O + 6CO 2 + 15.5 kJ/g of energy • Starch oxidation (C6H12O5)n + 6nO2 5nH2O + 6nCO 2 + 17 kJ/g of energy Energy needs Measurement of Energy Output Indirect calorimetry • Fat oxidation (e.g. glyceryl butro-oleostearate (main fat in butter) C3H5O3.C4H7O.C18H33O. C18H35O 43CO2 + 40H2O + + 60O2 39 kJ/g of energy Energy needs Measurement of Energy Output Indirect calorimetry • Respiratory quotient (RQ) • CO 2 Produced / O 2 Consumed • RQ for Carbohydrates = 1.0 C6H12O6 + 6O2 6H2O + 6CO 2 • RQ for fats = 0.71 (average) Energy needs Measurement of Energy Output Indirect calorimetry • RQ value can be used to find the amount energy produced per litre of oxygen consumed • Metabolic mix Energy needs Measurement of Energy Output Indirect calorimetry • Respiratory Gas Analysis • Respirmeters • Direct of measurement of O2 and CO2 • Heart Rate Monitoring • Heart rate calibrated against oxygen utilisation • Isotope Method • Labelled water (2H and 18O) • Difference of rates of loss of isotopes loss of CO2 What are the components of energy expenditure? 1: Basal metabolic rate Definition: Determinants: Calculation: Energy Out: Basal Metabolism • Largest daily energy output • Definition: “the sum total of minimal activity of all tissue cells of the body under steady sate conditions” • Men estimate: lbs body weight X 11 • Women estimate: lbs body weight X 10 • affected by – Muscle > Fat Male > Female – Young > Old – Temperature: body and environment Basal Metabolic Rate • BMR = number of calories would need daily simply to stay alive if were totally inactive, in bed, awake for 16 hours & slept for 8 hours • Harris-Benedict Equation: • Women: 661+(4.38 x weight in pounds)+(4.38 x height in inches)-(4.7 x age)=BMR • Men: 67+(6.24 x weight in pounds)+(12.7 x height in inches)- (6.9 x age)=BMR James & Schofield 1) Basal Metabolic Rate • 50-70% Energy Expenditure • Maintain basic metabolic processes Cells Growth • • • • • • • Muscles Temperature regulation Osmotic pumps Protein synthesis Heart Respiratory system Digestive tract Individual variation Within individual variation 10% Factors affecting BMR • 1) Body Size & Composition – Lean tissue BMR – Body weight wt lean tissue (but also fat) • 2) Age: – age Lean tissue • 3) Sex: Men lean • 4) Activity: Exercise lean tissue Factors affecting BMR • 5) Growth BMR – Children, pregnancy • 6) Fasting/starvation: BMR • 7) Fever/stress BMR • 8) Smoking/caffeine: BMR 2: Energy Expenditure Component : THERMIC EFFECT OF FOOD Definition: Determinants: Contribution to Total Energy Expenditure: 2) Energy Out: Dietary Thermogenesis • Dietary thermogenesis – Energy to digest, absorb, metabolize food – About 10% of calories eaten 2) Thermic Effect of Food • 3-6 hours following ingestion • ~10% energy intake – 2000 kcal diet = 200 kcal TEF • Affected by: – Meal size/frequency – Composition: Protein > Carbs/fat – Genetics 3: Components of Energy Expenditure Physical Activity Contribution to Total Expenditure: 4: What about accounting for changes in energy expenditure due to injury or trauma? 3) Energy Out: Physical Activity • Physical Activity affected by: – Intensity -- how vigorous – Time spent – Body weight 3) Physical Activity • Variable: 20-40% • Working muscles require energy – Heart/lung extra energy • Amt energy used depends on: – Muscle mass – Body weight – Activity nature & duration Activity Level and Metabolism • Activity can account for 20-30% of metabolism 1. Sedentary = Multiplier 1.15 x BMR 2. Light activity (Normal Every day activities) = Multiplier 1.3 x BMR 3. Moderately Active(exercise 3-4 x’s week) = Multiplier 1.4 x BMR 4. Very Active (exercise more than 4 x’s week) = Multiplier 1.5 x BMR 5. Extremely Active (exercise 6-7 x’s week) = Multiplier 1.6 x BMR Activity Level and Metabolism • If you change Light activity (Normal Every day activities) to Moderately Active(exercise 34 x’s week) daily caloric burning goes up 7.7% • If you change Light activity (Normal Every day activities) to Very Active (exercise more than 4 x’s week) daily caloric burning goes up 23% • If you change Light activity (Normal Every day activities) to Extremely Active (exercise 67 x’s week) daily caloric burning goes up 38.5% Full thickness Burns GI Cardiac trauma sepsis Renal Cancer Injury, Trauma, Surgery Neurohormonal Activation of the Stress Response Glucocorticoid & Catecholamine Activation, Hi Glucagon:Insulin Ratio, Growth Hormone Release Tachycardia, Tachypnea, Hyperglycemia, Mobilization of Body Fat, Massive Catabolism of Skeletal Muscle In Critical Illness, Timing of Assessment is Extremely Important! Why????? Metabolism in critical injuries goes through at least three distinct phases: Ebb (1st 24 hrs post-injury) Flow (Days 2-5) Anabolic (7-10 days) Immediate Needs to Sustain Life: • • • Restore blood flow; Maintain oxygen transport; Prevent/treat infections. If malnourished, introduce nourishment cautiously, if not-Refeeding syndrome: malabsorption, cardiac insufficiency, respiratory distress, CHF, etc. Maintaining Body Composition: Fuel Utilization in Maintenance and Injury Average Adult Composition Water % (w/w) 55 Protein 19 Adipose Tissue 19 CHO <1 Inorganic matter 7 Recommended Fuel Sources (% of kcal) Source Fat % of kcals DRVs Atwater* 30 33 Protein 10 15 CHO 60 52 *W.O. Atwater (1894), USDA Scientist credited with deriving physiologic energy values of pro, CHO, fat. PROGRESS!!! Fuel Sources During Exercise Normal ADL LIGHT MODERATE HEAVY Energy Requirements • Difficult to estimate • Direct measurement – Research • Estimates from averages – Based on age/sex – Assume light/moderate activity – Estimate TEF Energy • We Need Energy for 3 Reasons: – 1) Basal metabolism – 2) Physical activity – 3) Dietary thermogenesis • How many calories do you need? – Simple calculation 1) Basal Metabolism • Definition: Energy required to maintain normal body functions while at rest • To estimate the calories you need for basal metabolism – For men: Multiply body weight (lbs) by 11 – For women: Multiply body weight (lbs) by 10 2) Energy for Physical Activity ACTIVITY LEVEL PERCENTAGE OF BASAL METABOLISM CALORIES Inactive: sitting most of the day; <2 hours moving about slowly or standing 30% Moderate: sitting most of the day; walking or standing 2-4 hours, no strenuous activity 50% Active: physically active for >4 hours a day; little sitting or standing; some strenuous activity 75% 3) Dietary Thermogenesis • Definition: the energy expended during digestion of food • It accounts for approximately 10% of the body's total energy need (basal needs and energy needs) Doing the Calculation • Jane weighs 140 and is moderately active student (she goes to classes and goes to the gym 1hr/day) • Basal needs: 140 * 10 = 1400 • Physical activity needs: 1400 * .50= 700 • So far she needs 2100 calories, but wait, she has to digest! • 2100 * .10 = 210 calories • Now, we add it up for her: 1400 + 700 + 210= 2310 calories • How many calories do you need??? Energy Balance • Balanced energy intake: not losing or gaining weight • Negative energy balance (weight loss): energy intake < energy expended • Positive energy balance (weight gain): energy intake > energy expended Hunger vs. Appetite • Hunger: physical need for energy, accompanied with unpleasant symptoms such as weakness, stomach pains, irritability • Appetite: desire to eat is driven by mental stimuli Obesity • How do we define obesity? –By culture –By science Is Obesity an Epidemic? • Prevalence in US: 33% of adults and 25% of children are obese (But according to whom????) • Risks associated with obesity: diabetes, hypertension, stroke, heart disease, elevated total cholesterol, low HDL-cholesterol, certain types of cancer, gallbladder disease What Causes Obesity • 3 major factors contribute to the development of obesity – 1) Genetic background • Heredity may account for approx. 25-40% of obesity but this is very poorly understood • Effects on metabolism (rare); traits that predispose (common) – 2) Dietary intake – 3) Physical activity Measuring Body Fatness • • Weight-for-Height tables: – Dietary Guidelines for Americans – Metropolitan Life Insurance Company (allows for increased weight with age) – Limitations: not based on percentage body fat Body Mass Index (BMI)- widely used – Calculated by dividing body weight (in kg) by height (in meters) squared • 19-25 is considered acceptable • overweight is btw. 25-30 • > 30 obesity Some Methods for Assessing Body Fat: • Scale weighing doesn't distinguish between lean body mass and body fat – – – – – – – – Skinfold thickness measurements Bioelectrical impedance Underwater weighing Magnetic resonance imaging (MRI) CAT scans Ultrasound Total body electrical conductivity Magnetic resonance spectroscopy We Do Need Body Fat • For survival we need: – 3-5% for men – 10-12% for women • Low body fat associated with – – – – Delayed physical maturation during adolescence Infertility Accelerated bone loss Symptoms of starvation Role of Body Fat: – Makes hormones – Component of every type of body cell – Cushions internal organs – This fat is not available for energy Location of Body Fat is Important to Health • Central obesity is associated with more health risks than lower obesity • Assessing Body Fat Distribution: – Waist to hip ratio • More than .80 in women and .95 in men indicate central body fat distribution – Waist circumference • Over 40" (102 cm) in men (increased risk for health problems) • Over 35" (88 cm) in women Realities of Obesity • Myth: any individual can get to any body weight if they diet and exercise enough • People do come in different shapes and sizes and people should come in different shapes and sizes • From a health perspective, the goal of obesity prevention and treatment should be for people to eat a health promoting diet, get regular exercise, and pay attention to hunger and satiety cues – What are the barriers with this goal????? Body Composition Body Weight • Fat Mass + Fat Free Mass • FFM: muscle, lean tissue, bone, water • Diseases associated with: – Excessive fat mass – Depleted fat mass – Depleted FFM Body Weight • Body weight = Fat + FFM – Not % fat % FFM Healthy Body Weight • Weight associated lowest mortality • Techniques for Assessing body weight – Life Insurance Tables – Relative weight – Body Mass Index • Life Insurance Tables – Rarely used research/clinical practice • Relative weight – Actual weight/desirable weight – 110-120%: overweight – 120-130% obese • Disadvantages relative weight – Desirable difficult to define – Not sex specific – Not adjusted for age Body Mass Index (BMI) Weight (kg) BMI = Height (m2) Classification Weight (lb) Height (in2) BMI (kg/m2) X 705 Risk co-morbidity Normal values 18.524.9 Average Overweight Pre-obesity Obesity class I Obesity class II Obesity class III 25 2529.9 30.034.9 35.039.9 40.0 Increased Moderate High Very High World Health Organization, 1998 Limitations of BMI Both men have a BMI of 31 Find % body fat by: Underwater Weighing Skinfold • Measures subcutaneous fat • Accuracy depends on caliper skill Other High Tech Methods • Bioelectrical Impedance BMI • Magnetic Resonance Imaging MRI • “Bod-Pod” measures air displacement Bioelectrical Impedance • • • • • • • • Estimation of body composition Most used in clinical practice Based on electrical conduction through organism At higher frequencies (eg 50 kHz) resistance of cell membranes reduced so that current penetrates both extra- and intracellular fluids Bio impedance is a reliable prediction of the body’s main conduction material : water 73.2% FFM consists of water and total FM + FFM = total body weight Electrodes placed on dominant side of body; legs apart and not in contact More accurate in obese women than DEXA Fat intake but Overweight Total calories Physical activity 1 lb (0.4kg) body fat =~ 3500 kcal Energy Balance • Positive - Gain 1 lb - eat 3,500 kcal more than need • Negative -Lose 1 lb - eat 3,500 kcal less than need • If energy bal = - 500 kcal / day 3500/500 = 7 days to lose 1 lb • Best to combine with physical activity, e.g., mile walk = - 100 kcal What happens in weight loss? Water Fat Muscle mass May Bone density Gradual weight loss minimizes loss of muscle & bone • Drastic methods: fasting, surgery, liposuction • Other methods: diets, pills • • • • • Body fat location is important • Apple = Abdomen • Pear = Hips & thighs • Apple -> risk of heart disease • waist/hip ratio: >0.8 F, > 0.95 M indicates apple shape Assessing obesity: bmi, waist circumference and disease risk Disease Risk Relative to Normal Weight and Waist Circumference Men <102 cm Women <88 cm Men >102 cm Women >88 cm Category BMI Underweight — — Normal* <18.5 18.5-24.9 — — Overweight 25.0-29.9 Increased High Obesity 30.0-34.9 35.0-39.9 High Very high Very high Very high >40 Extremely high Extremely high Extreme obesity *An increased waist circumference can denote increased disease risk even in persons of normal weight. Adapted from Clinical guidelines. National Heart, Lung, and Blood Institute Web site. Available at: http://www.nhlbi.nih.gov/nhlbi/cardio/obes/prof/guidelns/ob_gdlns.htm. Accessed July 31, 1998. • Correlates with body fat content • European Origin – – – – Asian: healthy weight <23.5 Polynesian: healthy weight 18.5-26 Elderly: healthy weight up to 27 Requires further research • Not suitable for athletes Body Fat Distribution • disease risk/mortality with excessive body fat • ‘Healthy’ % body fat – 12-20% Men 20-30% Women • Fat distribution associated disease risk – Abdominal fat risk – Lower body fat: no increase risk • Central Obesity: Abdominal fat – prevalence Men, postmenopausal women • Measures of Central Adiposity • 1) Waist Circumference – > 88 cm women, 102cm men • 2) Waist:Hip Ratio – >0.8 women, 0.95 men • 3) Fat fold measures – Training required Obesity • • • • Prevalence increasing Serious health concern body weight 10% significant health risk Prevalence obesity increases – Age – Lower socio-economic status – Women (USA) • 0.5kg fat stores ~ 4500 kcals • Recommended weight loss: 0.5kg/wk max – Not greater than 1kg/wk • • • • intake by ± 600 kcals Slow reduction: decreased loss lean tissue Rapid loss: Large loss fluids Long term: 75% fat loss, 25% lean loss Weight Control • Case Study Underweight • <5% US population • Causes: – Hunger, illness, appetite, psychological traits, hereditary… • If malnourished weight gain nec – 1lb/month – 750-800kCals – Establish new eating habits Weight Gain Strategies • Energy dense foods – Whole milk not skim • • • • • Regular meals Large portions Extra snacks High energy beverages Exercise: add lean muscle Anorexia Nervosa: definition • • • • • • Starvation intentional Fear of fatness Significant weight loss altered body image Bizarre food behavior Amenorrhea, delayed menses Diagnosis • Refusal maintain body weight • Intense fear weight gain/fatness • Undue influence body weight/shape self esteem • Amenorrhea or delayed menses – 3 consecutive periods • 2 types • Restricting type – No regular binge eating/purging • Binge eating/purging – Regular binge eating/purging Demographics • • • • • • Inc dramatically 2-5% adolescent & young women 5% mortality rate Upper SES Family history Stress/perfectionist Physical consequences • PEM: similar to Marasmus – LBM BMR • • • • Decreased growth Irregular heart beat, blood pressure Electrolyte imbalance brain tissue, impaired immune system, anemia, digestive functioning • Development body hair Treatment • Multidisciplinary approach – Involve family • Restore nutritional status – Add 200kcal/week – Supplements initially • Psychological treatment – Reward eating not weight • Exercise education Bulimia Nervosa: diagnosis • Recurrent episodes binge eating – Large amount food short time – Sense of lack control • Inappropriate compensation • 2/week for 3 months • Self esteem unduly influenced body shape Demographics • More prevalent AN • More common in men than AN • Single white female – Well educated – Close to ideal body weight • Family history – Obesity, depression, abuse, conflicts, high expectations. Physical consequences immune system Fluid & mineral imbalance Abnormal heart rhythms, kidney damage UTI Damage pharynx, esophagus, salivary glands, teeth • Calloused hands • • • • • Treatment • • • • • • Avoid finger foods Prolong eating time, add bulk Satisfy hunger Plan meals, snacks Depression, additive behavior therapy Goal: Weight maintenance – Avoid cyclic weight, Binge Eating Disorder: BED • Binging without purging • Consume less during binge than BN, less restraint following • Associated with – Self loathing, depression, anxiety • Treatment: psychological counseling Female Athlete Triad Eating disorder •Restrictive dieting, •over exercising, •lack body fat Amenorrhea •hormones Osteoporosis •Bone mineralization OVERVIEW OF METABOLISM: Too Much, Too Little, Too Stressed Energy Economy in Feasting Metabolic Adaptation to Starvation • WHO Guidelines for Treatment of Severe Malnutrition Fuel Utilization in Hypermetabolic States Reclaiming Energy From Stored Fuel Sources: By Choice = Fasting By Necessity= Starving Exhaustion of “labile” CHO: Exhaustion of stored CHO: Problem: certain tissues require glucose for energy Tapping into stored protein: Short-term effect and contribution: If this contribution continues: Adaptation to Starvation/ Fasting Building glucose in the absence of labile or stored CHO: After deamination, the carbon skeletons of some amino acids can be used to make glucose or ketone bodies (ketoacids). Gluconeogenesis: the formation of glucose from lactate, some amino acids, and glycerol Long-term dependence on GNG to fuel brain is not feasible. Switch to ketone production within 10 d of fast -- provides majority of energy for brain. Protein sacrificed for glucose production for parts of brain requiring it. Benefits of Ketosis: • • provides needed source of energy; suppresses appetite. Concomitant Changes in Energy Expenditure Wasting results in decreased energy expenditure Heart mass Lung mass Skeletal muscle Hormonal response to fasting leads to energy conservation Metabolic Adaptations to Fasting/Starvation: ADVANTAGES & DISADVANTAGES Advantages Energy Expenditure Body Temperature Enhanced Survival Disadvantages Wasting of muscle mass Decreased immune competence