Mutation of Normal Genes
advertisement

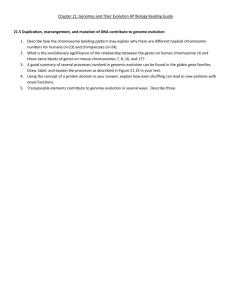
BIOLOGY OF CANCER AND TUMOR SPREAD Chapter 9 First Medial Description :Egyptian Text@ 2500BC-Imhotep Mastectomy: Johannes Scultetus (1595-1645)-fire, acid, leather binding Tumor – 1922 “it is tissue overgrowth that is independent of the laws governing the remainder of the body” “neoplastic overgrowth serves no useful purpose to the organism” Cancer Modern: “uncontrolled clonal proliferation of cells that can arise from virtually any cell type in the body” Derived from the Greek word for crab karkinoma – Hippocrates (460 – 370 BC) Malignant tumors Tumor Also referred to as a neoplasm – new growth Clonal Proliferation of a Single Cell “Storm Troopers: Star Wars” Benign vs. Malignant Tumors Benign Grow slowly Malignant Grow rapidly Well-defined capsule Not encapsulated Not invasive Well differentiated Invasive Poorly differentiated Low mitotic index High mitotic index Do not metastasize Can spread distantly (metastasis) Classification & Nomenclature Benign Named according to the tissue from which they arise, and includes the suffix - “oma” Lipoma Glioma Leiomyoma Chondroma Classification & Nomenclature • Malignant tumors – – – – – – Named according to the cell type from which they arise Epithelial tissue – carcinoma Ductal or glandular epithelium – adenocarcinoma Example: mammary adenocarcinoma Connective tissue – sarcoma Example: rhabdomyosarcoma Lymphatics – lymphomas Blood forming cells – leukemia Classification & Nomenclature Carcinoma in situ (CIS) Preinvasive epithelial malignant tumors of glandular or squamous cell origin that have not broken through the basement membrane or invaded the surround stroma Cervix, skin, oral cavity, esophagus and bronchus (epithelium) Stomach, endometrium, breast, large bowel (glandular) Stages of Cancer Spread “important component to diagnosis and treatment” Physical findings Laboratory tests – histological/biochemical/genetic Imaging studies Breast Cancer Cancer Cells Transformation Autonomy Cancer cells: independent from normal cellular controls Anaplasia Loss of differentiation (specialization and organization) “without form” - pleomorphic Cancer and Stem Cells Stem cells self-renew Cell divisions create new stem cells Stem cells are pluripotent Ability to differentiate into multiple different cell types Stem Cell Cancer…a genetic disease DNA the cell) “normal DNA** 1. RNA Proteins(workhorse of regulated growth” RNA** Proteins** Plasma membrane ** 2. Intracellular enzyme system** 3. Hormones/Growth factors** “unregulated growth…colonal proliferation ** multiple mutations- how many? Cancer…a genetic disease DNA** Example: RNA** EarlyCDT-Lung Proteins**(antigen) (Oncoimmune)-blood test 6 cancer associated antigens (p53, +5) Autoantibodies…against abnormal proteins** Medscape Medical News Sept 20,2010 Tumor Markers (DNA…RNA…Proteins) Tumor cell markers (biologic markers) are substances produced by cancer cells or that are found on tumor plasma cell membranes, in the blood, CSF, or urine Hormones Enzymes Genes Antigens Antibodies Tumor Markers Table 9-2 Used Screen and identify individuals at high risk for cancer(CA-125, PSA, CEA, Bense Jones protein) Diagnose specific types of tumors Observe clinical course of cancer Types of Genetic Lesions in Cancer Point mutation Subtle alterations (insertions, deletions, translocation) Chromosome changes (aneuploidy and loss of heterozygosity) Amplification Gene silencing Exogenous sequences (tumor viruses) Genetic Basis of Cancer Cancer-causing mutations Disease of aging (more mutation over time) Clonal proliferation or expansion Mutation leads to a Darwinian Survival advantage (↑ growth or ↓ apoptosis) Multiple mutations are required before cancer can develop (how many?) Oncogenes and Tumor-Suppressor Genes Proto-oncogene/Oncogenes Mutant genes that in their non-mutant state direct protein synthesis and cellular growth (accelerationpedal to the metal) Tumor-suppressor genes Encoded proteins that in their normal state negatively regulate proliferation Also referred to as antioncogenes (put the brakes on) Types of Mutated Gene:” 7 mechanisms” Secretion of growth factors (autocrine stimulation) Increased growth factor receptors (HER2/neu) Signal from cell-surface receptors is mutated to the “on” position Mutation in the ras intracellular signaling protein – (cell growth without growth factors) : “kinase” “all lead to increase growth” Types of Mutated Genes Types of Mutated Genes:”7 mechanisms” Inactivation of Rb tumor suppressor(tumor suppression) inherited Activation of protein kinase* that drive the cell cycle (oncogene) Mutation in the p53 gene (# apoptosis)-tumor suppression gene 17p13.1 *-PO4: activates and amplifies enzymatic processes over and over… Types of Mutated Genes:Bowel Cancer Question: How many mutations does it take to cause cancer? “Cancer Genome Atlas”-breast cancer 127 mutations Driver mutations: 11-15 (average=13)-directly cause growth and survival of the cancer; hit oncogenes/tumor suppression genes; limited number exist Bystander/passenger mutations: accidental copying of DNA; no impact on the biology of cancer Driver Mutations “Core metabolic pathway leads to dysregulation of any tumor” One or more proto-oncogene/tumor suppression gene may skip mutation, but others mutations activate the core pathway CANCER Angiogenesis (core pathway) Growth of new blood vessels Advanced cancers can secrete angiogenic factors (VEGF) Telomeres and Immortality: core Body cells are not immortal and can only divide a limited number of times (double about 50 times Hayflick Limit: 1961) Telomeres are protective cap on each chromosome and are held in place by telomerase (germ cells & stem cells) enzyme Telomeres become smaller and smaller with each cell division- “somatic cells” – quit dividing/die Telomerase enzyme: rebuilds telomeres Nobel Prize 2009:Blackburn, Greider, Szostak Telomeres and Immortality Mutations of Normal Genes → Cancer Genes Point mutation (most common) Change of one or a few nucleotide base pairs ras gene (pancreatic, colon) Chromosome translocation A piece on one chromosome is transferred to another t(8;14) Burkitt Lymphoma t(9;22) chronic myeloid leukemia (Philadelphia chromosome – 1960) Mutations of Normal Genes → Cancer Genes Chromosome amplification Duplication of a small piece of chromosome (DNA) over and over Result in ↑ expression of an oncogene N-myc oncogene @ 25% amplification Mutation of Normal Genes Oncogenes and Tumor-Suppressor Genes Oncogenes Mutant genes that in their non-mutant state direct protein synthesis and cellular growth (jammed acceleration) Tumor-suppressor genes Encoded proteins that in their normal state negatively regulate proliferation Also referred to as antioncogenes (put the brakes on) Mutations of Normal Genes →Cancer Genes Tumor-suppression genes(“inherited”) Unregulated cellular growth (put on the brakes) Rb gene (inactivated) → retinoblastoma, lung, breast, bone Two hits or mutations to inactivate the genes(Rb) Childhood retinoblastomas: 2 forms-inherited(2-6 mo.)/sporadic(2-4 yrs) De Gouvea(1872)-Brazilian Ophthmol. :young boy & his 2 daughters= cancer can be inherited Mutations of Normal Genes → Cancer Genes Loss of heterozygosity Loss of a chromosome region in one chromosome Unmasks mutation in the other locus of a tumor suppression gene Mutation of Normal Genes: Tumor Suppression Genes Mutations of Normal Genes → Cancer Genes Gene silencing No mutation or change in DNA sequence Whole regions of chromosomes are shut off while the same regions in other cells remain active Shuts off critical tumor suppression genes Mutations of Normal Genes → Cancer Genes Caretaker genes(“inherited”) Encode for proteins that are involved in repairing damaged DNA (UV or ionizing radiation, chemicals and drugs) Loss lead to increase mutation rates Chromosome instability Increase in malignant cells Results in chromosome loss, loss of heterozygosity and chromosome amplification Loss of tumor suppression genes with overexpression of oncogenes Genetics and Cancer-Prone Families Somatic cells – most cancers Exposure to mutagen Defect in DNA repair Not inherited Germ line cells (sperms and eggs) Vertical transmission of cancer causing genes Tumor suppression and caretaker genes One mutant allele (mom or dad), loss of heterozygosity in some cells → tumors Viruses and Cancer Implicated Hepatitis B & C viruses* Epstein-Barr Virus (EBV) Kaposi’s Sarcoma Herpes Virus (KSHV) Human Papillomavirus (HPV)* Human T cell Leukemia – Lymphoma Virus (HTLV) *80% virus-linked cancers Bacterial Causes of Cancer Helicobacter pylori Chronic infections associated with: Peptic ulcer disease Stomach carcinoma Mucosa-associated lymphoid tissue lymphoma Immunity and Cancer Surveillance – “nonself” Viral-induced cancers Immune defect – HIV /immunosuppressants ↑ viral cancers Organ transplant – immunosuppression – little or no ↑ in prevalent cancers So → ? Immunity and Cancer Chronic inflammation – “complex” Cytokine release form inflammatory cells – may promote growth Free radicals Mutation promotion ↓ response to DNA damage Diseases colitis – 30x ↑ Liver – HBV/HBC - ↑ risk Lung cancer – chronic asthma ↑66% Ulcerative Cancer Progression and Metastasis Metastasis – “a defining characteristic of cancer” Localized Breast 5 year survival > 90% - local 5 year survival < 3% - metastatic Pattern of spread Vascular, may be cured(“in situ”) : lymphatic and natural tissue planes Selectivity Breast to bone, not kidney or spleen Lymphomas to spleen, not bone Distant Metastasis Cancer cells must detach(invade) and migrate from its primary location Survive passage through the body Attach, invade and multiply while stimulating angiogenesis Thus: #1. Vast majority of cancer cells do not have the ability to form metastasis “appropriate cancer “seed” and a permissive “soil” Therapy for Cancer Surgery (1800-1900s) Halsted Radical vs simple mastectomy vs local excision + radiation Chemotherapy 3 to 7 drugs (ALL) Bone marrow transplant-maximum chemotherapy Radiation to tumors(Hodgkin’s lymphoma) Targeted: mutated gene’s protein Breast cancer +Her-2 membrane receptor: antibody:Herceptin CML: kinase signal inhibitor: Gleevec Why do the cancer cells become resistant to chemo/targeted therapy? A few stem cells of the cancer mutate and produce a new protein product that specific chemo/targeted therapy can no longer inhibit and kill. A new generation of resistant cancer cells evolves Clinical Manifestations of Cancer • Pain – – – Little or no pain is associated with early stages of malignancy Influenced by fear, anxiety, sleep loss, fatigue and overall physical deterioration Mechanism • – Pressure, obstruction, invasion of sensitive structures, stretching of visceral surfaces, tissue destruction and inflammation Priorities of treatment 1. Control – rapid and complete (patient) 2. Prevention – of recurrence Clinical Manifestations of Cancer Fatigue Tiredness, weakness, lack of energy, exhaustion, lethargy, inability to concentrate, depression, sleepiness, boredom, lack of motivation and ↓ mental status Most frequently reported symptom – cancer/treatment Mechanism – poorly understood Clinical Manifestations of Cancer • Cachexia – – – Most severe form of malnutrition Present in 80% of cancer patients at death Includes • – Anorexia, early satiety, weight loss, anemia asthenia, taste alterations and altered protein, lipid and carbohydrate metabolism Mechanism – multifactoral • • • Hormones (leptin) Neuropeptides Pro-inflammatory cytokines Cachexia Clinical Manifestations of Cancer Anemia Decreased amount of hemoglobin in the blood Mechanisms Chronic bleeding resulting in Fe deficiency, severe malnutrition, medial therapies or malignancy in blood forming organs Suppression of erythropoietin on the bone marrow rHuEPO Clinical Manifestations of Cancer Leukopenia and thrombocytopenia Direct tumor invasion to the bone marrow Chemotherapy toxic to bone marrow Infection Risk increases when the absolute neutrophil and lymphocyte counts fall ANC = WBC x (% neurophils + % bands), if < 1000 protective → isolation) [Table 10-3 Review] Clinical Manifestations of Cancer Paraneoplastic syndromes Symptom complex unexplained by local or distant spread of the tumor or by the effects of hormones released by the tissues from which the tumor arose 10% of individuals Earliest symptoms of an unknown cause May represent serious and life threatening problems May mimic cancer progression and interfere with appropriate treatment. [Table 10-4] Review Side Effects of Cancer Treatment “targeting the most rapidly growing cells” Gastrointestinal tract Oral ulcers, malabsorption and diarrhea Nausea and vomiting → antiemetic therapy Supplemental nutrition (enteral or parenteral) Bone marrow – ↓RBC with fatigue Platelets – bleeding White blood cells – infection (ANC) Anemia