Tuberculosis
advertisement

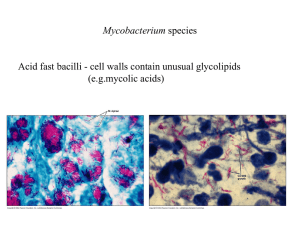
Tuberculosis:-Types, conventional and newer diagnostic techniques, treatment, prevention and control. Authors name:Divya Goel Mohammad Irshad Reza Mohammad Zakaria Modibo Blogs:-WWW.IRSHADD.WORDPRESS.COM B Pharm(SMAS) 3 rd year(1st sem) Galgotias University Introduction- Tuberculosis commonly known as TB, it is a chronic granulomatous disease which is major problem in developing countries. About one third of the world is getting infected by this disease in which India was the highest contributor with 2.2 million. It is an infectious disease caused by various strains of mycobacterium, usually by Mycobacterium tuberculosis. Tuberculosis typically attacks the lungs but can also affect other parts of the body, like stomach, urinary bladder, sex organs, etc. It spreads through the lymph and blood stream to any organ in the body. Generally two types of tuberculosis is known which is latent TB and Active TB. Latent TB do not have symptom, that means A person has been infected by TB bacteria but are not ill with disease and cannot transmit the disease. Active TB have symptoms like chronic cough with blood tinged sputum, fever ,etc,. Active TB develops by eventually progress in latent TB infections. About one in ten latent infection progress to active TB. If active TB left untreated, can kill more than 50% of patient. In past it is also called as phthisis, phthisis pulmonalis or consumption. Mode of transmission- Only the people having active TB can spread the disease. TB spreads in similar way to cold or flue but is not contagious. Tuberculosis spreads from infected person to healthy person through the air. When the people with TB bacteria present in their lungs or throat, cough, sneeze, sing or even talk, the germs may spread into the air. If a healthy person breathes in that germ containing environment, there is chance that they will become infected with tuberculosis. Usually repeated contact required for infection to occur. TB infection usually spread between family members who live in the same house. Symptoms-the symptoms of TB range from no symptoms(latent TB) to symptoms of active disease. Infect, you may not even be aware that you have latent TB infection until its revealed through a skin test, perhaps during a routine check up, if you have active TB disease, you may have these symptoms overall sensation of feeling unwell cough, possibly with bloody mucus fatigue in all body muscle and faint shortness of breath weight loss slight fever night sweats chest pain Sign and symptoms of TB are similar to those caused by other diseases, like Pneumonia, Malaria, lung cancer, anorexia nervosa, diabetes mellitus, allergic alveolitis, etc,. the classical symptoms of active TB infection are a chronic cough with blood tinged sputum, fever. Life cycle of the parasite(pathogen)- Mycobacterium tuberculosis is an acid fast obligate bacillus non motile anaerobic bacterium. The genus mycobacterium is defined by the mycolic acids and waxes, which makes the bacterium resistant to many bactericidal agent. Due to this killing of bacteria is difficult and can be easily spread. The generation time of M. tuberculosis is 15-20 hours. It is an obligate parasite and transferred through the air, therefore it appears in the upper lungs first. Mycobacterium tuberculosis when enters into the human body, they starts invading macrophases. It completes their life cycle in 5 stagesStage 1: onset(1-7 days):- Bacteria inhaled through the air and reaches to alveoli of lungs. In alveoli macrophases engulfed the bacteria. If the bacteria not killed by the macrophases, the bacteria reproduce the initiate the infection. Stage 2: symbiosis(7-21 days):- if the bacteria does not get killed, then the bacteria replicate until the macrophases burts. The bacteria now engulfed by alveolar macrophases and non activated macrophases. The blood arrived macrophases engulf the exposed bacteria in a symbiotic manner. Stage 3: initial caseous necrosis(14-21 days):- when the bacterial reproduction slowdown the tuberculosis starts developing. The bacterial reproduction slows because as the bacteria reproduce more, they kill all the surrounding non activated macrophases and run out of the cells to devide within. In addition the increased number of bacteria produces anoxic conditions and reduces the local pH. In this condition bacteria cannot reproduce anymore but can live for a long time. The bacteria forms tubercle. At this stage the host will test positive for Tuberculin. Stage 4: interplay of tissue damaging and macrophase activating immune response(after 21 days):-macrophases(some are inactive) surround the tubercle. Tubercle uses the inactive macrophases to reproduce and growth. The tubercle may break off and spread into the bronchus causes pulmonary TB. Sometimes tubercle spreads to the other parts of the body through blood stream and causes extrapulmonary TB(active TB). Stage 5: liquification and cavity formation:-sometimes the centres of the tubercles may liquefy which provides a very conductive environment for the bacteria to spread of disease rapidly. Not everyone will get to this stage. Only a very small percent of infected individual will progress to this stage. Types of tuberculosis[A]-On the basis of mode of action active TB miliary TB latent TB Active TB-It is an illness in which mycobacterium tuberculi readily multiply and invades different organs of the body excluding only hair and nails. It generally attack the person who have poor health or poor immune system. The bacteria is continuously reproducing and spreading in infected person body causing damage to the tissues. Person having active TB feels sick typical symptoms include cough lasting for 3 weeks, weight loss, night sweat and fever. Miliary TB-It is also known as disseminated TB, tuberculosis cutic acuta generalisata and tuberculosis disseminata. Military TB is the widespread dissemination of mycobacterium TB via hematogenous spread. Classically military TB is defined as millet like seeding of TB bacilli in the lung as evidenced on chest radiography. Miliary TB is present upto 20% of all extra pulmonary TB cases. latent TB- In this infection the person is infected with M. TB but do not show symptom and are not contagious. About 1/3rd of world of population is believed to have latent TB. It is based on the immunity of the patient. It changes into active TB much faster in those who have weak or poor immune system. It usually occurs in lungs. Person don’t look or feel sick. Infected person chest x rays are usually normal. It can be diagnosed by Tuberculin skin test and by IGRAs test. [B]- on the basis of site of action Pulmonary TB Extra pulmonary TB Pulmonary TB- Pulmonary TB is a contagious bacterial infection that involves the lungs, and it may spread to the other organs. Person can get pulmonary TB by breathing air contaminated by droplets from cough or sneeze of an infected person. Different types of pulmonary TB are Primary TB pneumonia- it is an uncommon type of TB present as pneumonia, patient feel high fever and cough. It generally occurs in extremely young children and elderly persons. Tuberculosis pleurisy- it develops soon after the initial Infection. Granuloma located at the edge of the lung ruptures into the pleural space(space between the chest wall). Once the bacteria invade the pleural space the amount of fluid increases dramatically and compresses the lungs causing shortness of breath and sharp chest pain. Cavitary Tuberculosis- This type of TB occurs in reactivation disease. It invades upper lobes of the lungs. It can rarely occur soon after primary infection. Laryngeal Tuberculosis- it is extremely infectious. Larynx or vocal cord area is infected Miliary Tberculosis- A disseminated TB which describe small nodules throughout the lung that look like millet seed appear on chest x-ray. Extra pulmonary TB- TB can affect any part of the body like inner organs, bones, brain spine, etc., while the majority of TB infections affects the lungs. If the TB infection is not primarily located in the lung, it is known as extrapulmonary TB. World wide it is estimated that between 10 to 25% of TB infections occurs extrapulmonary. It is difficult to diagnose extrapulmonary TB because less common doctors often think of other causes for the symptoms, for e.g., pain in the right ankle is more likely to be of sprained ankle than of joint TB. The most common forms of extrapulmonary TB are Lymph node Tuberculosis- TB bacilli often infect the lymph nodes in the neck and above the clavicles(the thin bone underneath the shoulders), which then swell up and skin around them becomes inflamed. Tuberculosis pericarditis- the membrane surrounding the heart( the pericardium) is affected in this condition. This causes the space between the pericardium and heart to fill with fluid, impending the heart’s ability to fill with blood and beat efficiently. Osteal Tuberculosis-it is an infection of bone caused by the TB bacteria. This extrapulmonary form can lead to bone tissue weakening and even bone fractures depending on where the disease has spread in body and which bone has affected, it usually attack the spine which can lead to compression fracture and back deformity. Renal Tuberculosis- Mycobacterium TB invades the kidney, normally because of some heamatogenous seeding, although it is secondary to a tuberculosis infection of the Gastrointestinal tract or bone. Adrenal Tuberculosis-TB of adrenal gland can lead to adrenal insufficiency. Adrenal insufficiency is the inability to increase steroid production by the adrenal gland during stress, causing weakness and collapse. Tuberculosis meningitis- it is infection of tissue covering brain and spinal cord( meninges) caused by Mycobacterium TB. This infection can leads to fever, mental status changing, nausea, vomiting, stiff neck, sensitivity to light, etc,. [C]-On the basis of drug resistance Multi drug resistant TB(MDR-TB) Extensively drug resistant TB(XDR-TB) Totally drug resistant TB(TDR-TB) Multi drug resistant TB(MDR-TB)-MDR-TB is defined by the resistance to the two most commonly used drugs in the current four drug( or first-line drug) regimen namely Isoniazid and Rifampin. MDR-TB has emerged and spread due to inadequacy of treatment. The treatment for drug resistant TB can take upto two years and it is so complex, expensive, and toxic that third of all MDR-TB patient die. MDR-TB is treated with second-line drug which are more expensive than first-line drug and more adverse effects also. Directly observed therapy helps to improve outcomes in MDR-TB and should consider an integral part of treatment of MDR-TB. Treatment must be given for minimum 18 months and cannot be stopped until the patient has been culture negative for minimum 9 months. Symptoms are same as for ordinary TB. Drugs used are Capreomycin, kenomycin, and Amikacin in addition to Isoniazid and Rifampin. Extensively drug resistantTB(XDR-TB)- XDR-TB is relatively rare type of multi drug resistant TB. XDR-TB is resistant to ant fluoroquinolone and at least one of three injectable second-line drugs in addition to isoniazid and rifampin, this makes the XDR-TB treatment extremely complicated and impossible in resource-limited area. XDR-TB can be cure but with the current drug available , the likelihood of success is much smaller than in patient with ordinary TB or even MDR-TB. Treatment depends on extent of drug resistance, the severity of disease and whether the patient immune system is compromised. Totally or Extremely drug resistant TB(TDR or XXDR-TB)- TDR-TB is resistant to all first-line and second-line TB drugs. This makes it almost but not totally impossible to treat. TDR-TB has been identified in 3 countries; India, Iran and Italy. Epidemiology-Tuberculosis is the second major cause of death world wide. It is one of the most common infectious disease. About 32% of the worlds population is infected by TB bacterium. The World Health Organisation(WHO) estimates that one third of the worlds population has latent TB infection. Every year approximately 8 miliion of infected people develop active TB and 2 million die(in 2006), 1.5 million die(in 2013), 1.3 million die(in 2012). Recent Data- Tuberculosis has increased over the last 20 years. WHO estimates that about 30 million people will be infected by TB within the next 20 years. WHO ‘s “Global Tuberculosis Report 2014”shows that 9 million people develop TB in 2013 and 1.5 million died including 3.6 lacks people who were HIV positive. This data revealing that there are almost half a million more cases of the disese than previously estimated, however the mortality rate from TB is still falling and has dropped by 45%since 1990, while the number of people developing the disease is declining by an average 1.5% a year. The MDR TB(Multi drug resistant TB) crisis continues with an estimated 4.8 lacks cases in 2013. Futhermore XDR TB( extensively drug resistant TB) and TDR or XXDR(totally or extremely drug resisitant TB), is even more expensive and difficult to treat than MDR TB has now been reported in some countries. On 20 january 2015 in Geneva, the global TB programme welcomes the decision by United Nation secretory General Banki Moon to appoint Dr. Eric P Goosby as the new UN special envoy in TB. Special envoy Goosby brings a wealth of experience to the fight against this infectious disease. Global TB report 2014- TB remain one of the worlds deadiest communicable disease in 2013, an estimated 9 milion people developed TB, 1.5 million died from the disease, 360,000 of whom were HIV positive, and estimated that 37million lives were saved between 2000 and 2013 through effective diagnosis and treatment. Most deaths from TB are preventable, the death toll from the disease is still unacceptably high and efforts to combat it must be accelerated if 2015 global targets, set within the context of development goals(MDG’s). TB is present in all regions of the world and the global TB report 2014 includes data compiled from 202 countries. A special supplement to the 2014 report high lights the progress that has been made in survilliance of drug resistant TB over the last two decades and the response at global and national levels in recent years. Worldwide the progression of new cases with multi drug resistant TB was 3.5% in 2013 and has not changed compared with recent years. However much higher levels of resistance and poor treatment outcomes are of major concern in some part of the world. The supplement drug resistant TB. Survelliance and response defines priority actions needed from prevention to occur. Burden of disease and progress towards 2015 global targets- improved data given a clear global picture of TB burden1- the data available to estimate TB disease burden continue to improve. In 2013 direct measurement of TB were available from 126 countries and since 2009 there has been an increase in number of direct measurements of TB prevalence from nation to worldwide. 2-of estimated 9 million people who developed TB in2013 more than half (56%) were in the Asia rates of case deaths relative to population. India and China alone accounted for 24% and 11% of total case respectively. 3- about 60% of TB case and death occur among men but the burden of disease among women is also high. In 2013 an estimated 510,000 women died as a result of TB, more than one third of whom were HIV positive. There were 80,000 deaths from TB among HIV negative children in some year. 4- the 2015 millenium development goal(MDG) of halting and reversing TB incidence has been achieved globally in all six WHO regions and is most of the 22 high TB burden countries worldwide, tuberculosis incidence fell at an average rate of about 1.5% per year between 2000 and 2013 5- the TB rate fell by an estimated 45% between 1990 and 2013 and the TB prevalence rate fell by 42% during the same period. Progress needs to accelerate to reach the sop TB partnership targets of a 50% reduction by 2015 6- two out of six WHO have achieved all three 2015 targets for reduction in TB disease burden (incidence, prevalence, mortality) the region of the America appears on track to meet all three targets, prevalence and mortality rates. Diagnosis methods- to confirm the infection whether a person has been infected with TB bacteria or not two kinds of tests, thar are used which is mantoux test or tuberculin skin test and TB blood test. These test only tells that a person has been infected or not. TB is often difficult to diagnose, even if person has symptoms. This difficulty may occur due to problem in TB test, like some test takes long time to obtain a result and some are not very accurate. Some test has low sensitivity(the ability to detect people with TB). It means that there will be significant number of false negative test. This test suggesting that, a person doesnot have TB, but actually they have. On contrary some tests have low specificity( ability to detect the people who haven’t got TB). It means that there will be significant number of false positive test. This test suggesting that a person has TB, but actually they donot have. Chest X-ray or Roentgenography-this test is mainly used forpulmonary TB and is advised by the doctor, if a patient had positive skin test. Lesions may appear in anywhere in the lungs mainly in upper lungs and is characterized by having cavities or spots and consodillation where immune system has walled off TB bacteria. In case of milliary TB, on chest x ray tiny spots appear similar to millat seeds. In immunodepressed person like in HIV positive patints the chest x ray may appear normal. If mediastinum or pleura is affected then it is termed as tuberculosis pleurisy. Abreugraphy or MMR(mass miniature radiography) is a type of x ray used for diagnosis of tuberculosis. MMR is much less expensive but its resolution is limited(it does not allow the diagnosis of cancer). CT(computed tomography) scans provide more detailed images than on x ray. Interferon Gamma Release Assay(IGRA)- IGRA is a newer type of blood test for TB mainly for latent TB. It is based on the ability of mycobacterium tuberculosis antigens ESAT-6(early secretory target-6) and CFP-10(culture filtrate protein-10) to stimulate the production of interferon gamma in host. This test measures the person’s immune response to the bacteria. This test is performed by taking a blood sample and mixing it with special substances to identify the gamma interferon or cytokine if present. Antibodies from lymphocyte secretion(ALS) assay- ALS assay is an immunological assay to detect mainly active TB. This assay can quantitatively measure the PBMC(peripheral blood mononuclear cell) produced antigen specific antibody, cultured in postvaccination blood sample. It is impossible to distinguish between the antibodies is recently produced by PBMC or the preexisting antibodies. To perform the ALS assay PBMC were isolated from blood sample via histopaque layering method. The isolated PBMC were treated with citrate anticoagulant and diluted with sterile phosphate buffered saline(PBS-Sigma). The diluted PBMC now differential centrifugated and suspended in 24- well tissue culture plates culture medium and were incubated at 37’c with 5% CO2. Cultured supernatants were collected after suitable time of incubation and tested against BCG or by ELISA. Test indicates the negative or positive result. Newer Diagnostic Techniques/methodsConventional diagnostic techniques for detection of TB have limitations of speed, sepecificity, and sensitivity. Because this a variety of new diagnostic techniques have been developed for the more rapid and sensitive detection of Mycobacterium tuberculosis. New diagnostic techniques broadly can be divided into two parts 1)Molecular methods 2)Non molecular methods Molecular methods- Variety of molecular assays have been designed to detect the presence of Mycobacterium tuberculosis and to detect the bacteria resistant to Isoniazid and rifampin i.e., to detect the multi drug resistant tuberculosis(MDR-TB) and extensively drug resistant tuberculosis(XDR-TB) (I)PCR (Polymerase Chain Reaction)/Line probe assay- This assay involves extraction of DNA from clinical specimens, PCR amplification of DNA sequence, hybridization of labeled PCR products with oligonucleatide probes immobilized on strip, and calorimetric development that allows for lines to be seen where the probes are located, hence this assay is termed as line probe assay. This is very sensitive diagnostic technique, it can even detect the single bacteria. The commercially PCR assay is based on amplification of 584 bp region of a gene encoding 16sRNA. This assay is also used for detection of MDR TB. First line probe assay- First line probe assay also known as INNO-LiPA Rif.TB (Innogenetics NV) assay is the type of line probe assay, it was evaluated for the detection of first line drug resistance mycobacterium tuberculosis i.e, identification of Mycobacterium tuberculosis complex strains and for the detection of Rifampin resistance mycobacteria. The results of clinical evaluations of the assay indicated that it accurately detects the resistance to Rifampin, but some evaluations showed that the assay was less sensitive for the detection of Mycobacterium tuberculosis complex strains. This assay has the potential to provide rapid information that is essential for the effective management of MDR-TB. Second line probe assay- second line probe assay is the genotype MTBDRs1 assay, evaluated for the detection of second line drug resistance Mycobacterium tuberculosis i.e, identification of Mycobacterium TB resistant to fluoroquinolones, kanamycin, amikacin, ethambutol, and capreomycin.The sensitivity for detection of fluoroquinolone resistance was 75.6% (31/41) (95% confidence interval [95% CI], 59.7% to 87.6%), and for kanamycin resistance, the sensitivity was 100% (5/5) (95% CI, 47.8% to 100%). The sensitivity of the test for detection of ethambutol resistance was low, consistent with previous reports, at 64.2% (34/53) (95% CI, 49.8% to 76.9%). The specificity of the test was 100% for all three drugs. This assay has the potential to provide rapid information that is essential for the effective management of extensively drug resistance tuberculosis (XDR-TB). (II)loop mediated isothermal amplification- The loop mediated isothermal amplification assay is based on a novel form of nucleic acid amplification with sufficient efficiency that enough DNA is generated to enable detection by visual inspection of fluorescence. In contrast to the polymerase chain reaction (PCR) technology in which the reaction is carried out with a series of alternating temperature steps or cycles, loop mediated isothermal amplification is carried out at a constant temperature, and does not require a thermal cycler. This method has been evaluated on limitation basis and has been shown to have high sensitivity for smear-positive specimens but low sensitivity for smear-negative specimens. (III) Oligonucleotide Microarray- oligonucleotide microarray measure the expression levels of large numbers of genes simultaneously or to genotype multiple regions of a genome, which can be used to detect either conserved sequences for detection of microorganisms and/or detection of mutations in sequences that confer drug resistance of an isolate. The TB-biochip (a oligonucleotide microarray), has been evaluated for the detection of Rifampin resistance in mycobacterium tuberculosis. In an evaluation the assay showed a sensitivity of 80% for detecting rifampin resistance. (IV)Xpert MTB/RIF Assay- Xpert MTB/RIF assay is a molecular assay which detects the DNA in TB bacteria. It uses a sputum sample and can give a result in less than 2 hours. it can also detect the genetic mutations associated with resistance to the drug Rifampicin. In a limited evaluation, the assay was shown to be 100% sensitive for detecting smear-positive isolates but only 71.7% sensitive for detecting smear-negative culture-positive isolates. In a larger field trial, the assay was shown to be 98.2% sensitive for the identification of culture-positive isolates but only 72.5% sensitive for the identification of smear-negative culture-positive isolates. In the same study, the assay was shown to be highly sensitive for detecting rifampin resistance, correctly identifying 97.6% of rifampin-resistant isolates and 98.1% of rifampin-susceptible isolates. One obvious disadvantage to this system is the inability to test for and detect isoniazid resistance. Non molecular methods- Non molecular methods are developed for the detection of Mycobacterium tuberculosis complex and/or antimicrobial drug resistance. This method also used for the detection of drug resistance TB( multi drug resistance and extensively drug resistance). A few of these methods are designed to improve existing technology, such as specimen processing and smears, whereas others are based on newer technologies. This methods is based on smear microscopy. Introducing these methods would require fewer resources than would introducing new technologies and these methods are likely to be less expensive than new technologies. (I)Colorimetric Assays- Calorimetric assay is based on the observation that growing tubercle bacilli convert a yellow dye [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide or MTT] to a purple color that can be detected visually or by use of a spectrophotometer. Calorimetric assay is performed directly on sputum specimens and indirectly on Mycobacterium tuberculosis clinical isolates. However, due to their high cost and equipment requirement, these new methods are not feasible in the clinical laboratories of developing countries in the diagnosis. of tuberculosis (TB). Instead, these countries use the proportional method, which is very time-consuming . Although these methods are conceptually straightforward, they are likely to be useful primarily in larger laboratories with the capacity to perform more complex assays. (II) MDR-XDR TB Color Test- MDR-XDR TB Color assay is based on Thin-Layer Agar (TLA) technology. This Colour Test combines the thin-layer agar technique with a simple colour-coded quadrant format, selective medium to reduce contamination and colorimetric indication of bacterial growth to simplify interpretation. This assay is based on color changes in the 4 quadrants of the plate, with 1 quadrant for detection of growth and the other 3 quadrants for Antimicrobial susceptibility testing or AST (1 quadrant each for isoniazid, rifampin, and ciprofloxacin). This assay has high sensitivity and specificity for detecting drug resistance TB. (III) Microscopic Observation Drug Susceptibility (MODS) Assay-the microscopic observation drug susceptibility assay (MODS), is a novel assay developed in Perú. This assay is based on use of an inverted light microscope and culture in Middlebrook 7H9 broth to detect mycobacterial growth.MODS is a culture method shown to be more sensitive, faster and cheaper test than current culture-based tests for tuberculosis. This assay detects resistance to both isoniazid and rifampicin; the two most commonly used drugs for therapy i.e, it detects mono-resistant, and multi-drug resistant (MDR) TB usually within a 5 to 10 day incubation period. The conventional MODS method was approved by the WHO for use in direct specimen testing of sputum for TB. The WHO determined the conventional MODS method to be 98% sensitive and 99% specific for the detection of rifampin resistance; and 91% sensitive for isoniazid resistance. (IV)Fluorescent Light Emitting Diode (LED) Microscopy-LED microscopy uses LED technology as a light source for the diagnosis of tuberculosis. LED microscopy is more sensitive and equally specific, compared with either conventional light or fluorescent microscopy. Light-emitting diodes (LED) have been developed to offer the benefits of fluorescence microscopy without the associated costs. The World Health Organization (WHO) recommends that conventional fluorescence microscopy be replaced by LED microscopy, and that LED microscopy should be “phased in as an alternative for conventional light microscopy”. Other newer diagnostic technique for tuberculosisSepti-chek AFB-Septi-chek AFB (Roche Diagnostic Systems) is a test which allows simultaneous detection of Mycobacterium tuberculosis and non-tuberculosis mycobacteria. It is biphasic culture system made up of a modified Middlebrook 7H9 broth with a three-sided paddle containing chocolate, egg based, and modified 7H11 solid agar, the bottle is inverted regularly to inoculate the solid media. This method requires about 3 weeks of incubation, but the nonradiometric approach has the potential to expedite processing, obviate CO2 incubation requirements thus facilitating early detection of positive cultures. The growth is observed by observing the three-sided paddle. BACTEC 460 radiometric culture system- BACTEC 460 radiological culture system has been long considered the best method for rapid testing of susceptibility of M tuberculosis to major antituberculous drugs such as rifampicin, isoniazid, ethambutol, pyrazinamide and streptomycin, i.e, to detect the multi drug resistant TB(mdr-tb) and extensively drug resistant TB(xdr-tb). Culture media contains 14C-labeled palmitic acid. If present in the broth, mycobacteria metabolize the14C-labeled substrates and release radioactively labeled 14CO2 in the atmosphere, which collects above the broth in the bottle. The instrument withdraws this CO 2containing atmosphere and measures the amount of radioactivity present. MB/Bact system-MB/BacT is a non-radiometric continuous monitoring system designed for the isolation of mycobacteria from clinical specimens. This system is based on the colorimetric detection of CO2. It had slightly longer time for detection of growth as compared to BACTEC 460 radiometric culture system. ESP blood culture system-The ESP blood culture system was designed to detect consumption and/or production of gas by microbes, rather than only the production of CO2, as is the case with BACTEC 460 radiometric culture system. Organism are cultured in a modified Middlebrooks 7H9 broth with enrichment and a cellulose sponge to increase the culture's surface area. The instrument detects growth by monitoring pressure changes that occurs as a result of consumption and/or production by the organism as they grow. preventionStrategies for TB prevention- TB prevention consists of two main parts. The first part of TB prevention is to stop the transmission of TB from one adult to another. This is done through firstly identified people with active TB and then curing them through the provision of drug treatment. With proper TB treatment someone with active TB disease will very quick not be infectious and so can no longer spread the disease to others. The second main part of TB prevention is to prevent people with latent TB from developing active and infectious. TB prevention-the BCG vaccine- The TB vaccine called Bacillus Calmette Gurene(BCG) was first developed in the 1920. It is one of the most widely used of all current vaccine, and it reaches more than 80% of all new born children and infants in countries where it is part of the national childhood immunization programme. The BCG vaccine has shown to provide children with excellent protection against the disseminated forms of TB. Protection against pulmonary TB in adults is variable most transmission originates from adult cases of pulmonary TB. The BCG vaccine is generally used protect children rather than to interrupt transmission amongst adults. For TB prevention the WHO recommend the drugs Isoniazid should be taken daily for atleast six month and preferably nine months. The main target groups for TB treatment and prevention1-infants and children age less than 4 year old 2-people infected within the previous 2 year 3-people infected with both TB and HIV 4-people who have certain clinical condition 5-people with diabetes and people with chronic renal failure. Ioniazid is a cheap drug, but in a similar way to the BCG vaccine. it is mainly used to protect individual rather than to interrupt transmission between adults, this is because children rarely have infection TB and it is hard to administer ioniazid on large scale to adults who do not have any symptoms. Taking isoniazid daily for six months is difficult in respect of adherence. Preventing TB transmission in households action to be takenIn households where someone has infectious TB, the following action taken 1-household should be adequately ventilated 2-anyone who cough should be educated on cough etiquette and respiratory 3-while smear positive TB patient should spend as much time as possible outdoors. If possible sleep alone in separate, adequately ventilated room. Spend as little time as possible on public transport. Physical measures for TB prevention- before drug treatment for TB become available, removing TB patient from their homes and putting them in isolation in sanatoria, was the main way of reducing the transmission of TB. TB prevention in health care facilities-heath care workers who provide care for patients with TB, must follow infection control procedures to ensure that TB infection is not passed from one person to another. Every country should have infection control guidance which clearly needs to take into account local facilities and resources as well as the numbers of people being provides with care. However infection control guidance must not only be written but also implemented. TB transmission occurs in hospitals in 2012, it was reported that patient in the UK had become infected with TB and had died, as a result of receiving kidney dialysis when sitting next to another patient with infectious TB. Treatmentmedications are the corner stone of TB treatment. But treating TB takes much longer than other bacterial infections. With TB you must taken antibiotics for at least six to nine months. The exact drugs and length of treatment depend on your age overall health, possible drug resistance, the form of TB( latent or active) and the infection location in the body. Recent research suggests that a shorter term of treatment four months instead of nine with combined medication may be effective in keeping latent TB from becoming TB. With the shorter course of treatment, people are more likely to all their medication and risk of side effects is lessened. Studies are ongoing. Most common TB drugs- if you have latent TB, you may need to take just one type of drugs. Active TB particularly if it is drug resistant strain will require several drugs at once. The most common medication used to treat TB include- Isoniazid, Rifampin(rifadin, rimactane), Ethambutol(myambutol), pyrazinamide If you have drug resistant TB, a combination of antibiotics called fluoroquinolones and injectable medications such as Amikacin, ksnsmycin or capreomycin, are generally used for 20 to 30 months. Some types of TB are developing resistance to these medications as well a number of new drugs are being looked at as add on therapy to the current drug resistant combination treatment, including- Bedaqufline, Delamanid, PA-824, Linezolid, Sutezolid. Medication side effects-serious side effects of TB drugs aren’t common but can be dangerous when do occur. All TB medications can be highly toxic to your liver. When taking these medication call your doctor immediately if you experience any of the following- nausea or vomiting, loss of appetite, yellow colour to skin, dark urine, fever more days and no obvious cause. Complete treatment is essential-after a few weeks you wont be contagious and you may start to feel better. It might be tempting that to stop taking your TB drugs. But it is crucial that you finish the full course of therapy and take the medication exactly as prescribed by your doctor stopping treatment too soon or skipping doses can allow the bacteria that are still to alive to become resistant to those drugs leading to TB that is much more dangerous and difficult to treat. To help people stick with their treatment a program called directly observed therapy(DOT) is recommended. In this approach, a health care worker administers your medication so that you do not have to remember to take in an your own. TB detection and treatment outcomes-the treatment success rate among new cases of TB continues to be high but major efforts are needed to ensure all cases are detected, notified and treated. 1-2013,6.1 million TB cases were reported to WHO of these 5.7 million were people newly diagnosed and another 0.4 million were already on treatment. 2-notification of TB case has stabilized in recent years. In 2013 about 64% of the estimated 9 million people who developed TB were notified about as newly diagnosed cases. This is estimated to have left about 3 million cases that were either not diagnosed, diagnosed but not reported to national TB program(NTPs) major efforts needed. 3-in 2013, the treatment success rate continued to be high at 86% among all new TB cases. 4-although treatment success rate in the European region have improved since 2011, they were still below average in 2012 at 75%. Increase use of new diagnostics is ensuring that significantly more TB patients are correctly diagnosed, but major treatment gaps remain and funding is insufficient. Multi drug resistant TB detection outcomes1-globally 3.5% of new and 20.5% of previously treated case were estimated to have had MDRTB in 2013. This translates into an estimated 480,000 people having developed MDR-TB in 2013. 2-on average, an estimated 9% of patients with MDR-TB had extensively drug resistant TB(XDRTB). 3- in late 2013, WHO expanded its recommendation on the use of x per MTB/RIF to include the diagnosis of TB in children. Refrences: World Health Organization (2011). Guidelines for intensified tuberculosis case-finding and isoniazid preventive therapy for people living with HIV in resource-constrained settings. Available online: http://www.who.int/hiv/pub/tb/9789241500708/en. World Health Organization (2011). Guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. European Respiratory Journal, 38(3): 516–528. Khan K, Wang J, Hu W, et al. Tuberculosis infection in the United States: national trends over three decades. Am J Respir Crit Care Med. 2008;177:455-460. Alami NN, Yuen CM, Miramontes R, et al. Trends in tuberculosis - United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63:229-233. Menzies, D; Al Jahdali, H, Al Otaibi, B (March 2011). "Recent developments in treatment of latent tuberculosis infection". The Indian journal of medical research 133(3): 257–66. Acton, Q. Ashton (2011). Mycobacterium Infections: New Insights for the Healthcare Professional. ScholarlyEditions. p. 1968. Centers for Disease Control and Prevention (2005). Guidelines for using the QuantiFERON®-TB test for diagnosing latent Mycobacterium tuberculosis infection. MMWR, 54(RR-15): 49–55. Griffith D, Kerr C (1996). "Tuberculosis: disease of the past, disease of the present".Journal of Perianesthesia Nursing 11 (4): 240–5. Bloom, editor, Barry R. (1994). Tuberculosis : pathogenesis, protection, and control. Washington, D.C.: ASM Press. Markowitz N, Hansen NI, Hopewell PC, et al. Incidence of tuberculosis in the United States among HIV-infected persons. Ann Intern Med. 1997;126:123-132. Thankyou