The Clinical Interdisciplinary Team for the State of Hawaii
The Clinical Interdisciplinary
Team for the State of Hawaii
Developmental Disabilities
Division
David Fray DDS, MBA
Chief, State of Hawaii Developmental Disabilities Division (DDD)
Jeffrey Okamoto M.D.
Medical Director, State of Hawaii Developmental Disabilities Division (DDD)
We [and/or an immediate family member including our spouses/partners] DO NOT have a financial interest, arrangement or affiliation with a commercial organization (currently or within the past 12 months) that may have a direct or indirect interest in the subject matter of my presentation.
Our presentation or participation will not involve comments or discussion concerning unapproved or off-label uses of a medical device or pharmaceuticals.
Objectives
Orient on the MR/DD Medicaid Home and Community based waiver program and what diagnoses and services this encompasses
Explain why Pediatric support is helpful in these activities
Explore possible service and training endeavors with a State Agency
Highlight transition issues around people with developmental disabilities
Prototypical
Developmental
Disabilities
Mental Retardation
Autism
Cerebral Palsy
Seizure Disorder
Most CNS disorders with comorbid cognitive impairment
Federal definition of
Developmental Disability
Results in functional limitations in three or more of the following areas of life activity:
– self care
– learning
– mobility
– self-direction
– receptive or expressive language
– capacity for independent living
– economic self sufficiency
Prevalence of Intellectual
Disability
Estimate of persons with Intellectual
Disability in a population is 0.70 % to
1.25 % source: State of the States Report, 2008
David Braddock PhD
University of Colorado
History of DD Division
Services in Hawaii
Waimano Training School and
Hospital: 1924-1998
Community Based Waiver
Services began in 1982
1990s: limited admissions and lengthy waitlists
Legal catalysts: Olmstead/ Makin
2000s: Family Support Model
Nationally, since the 1960s, there has been increasing awareness that individuals with DD/MR can be, and should be, served in the community.
These individuals are citizens who are members of their communities as any other person – able to participate in activities, earn incomes, and live in residences of their choice.
Christmas in
Purgatory
Look Magazine, 1967
In years past, individuals with DD/ID were served primarily by
Hawaii’s institution for the mentally retarded.
Waimano Training
School and Hospital
DEINSTITUTIONALIZATION
In 1999,
Hawaii closed Waimano
Training School & Hospital
– one of the first ten states in the nation to eliminate all large state institutions.
What is the DD
Waiver?
Origin: The Katie Beckett “waiver” in 1982 by President Reagan
Community Support Services
Not Medicaid State Plan Services i.e. medical services, medicines
Not an entitlement program; but an option to State Medicaid agencies
Services vary by State
What is the DD
Waiver?
Personal assistance, habilitation, behavioral assessment & planning, case management, emergency plan, environmental modifications, respite, pre-vocational services, specialized equipment
Individualized Support Plan (ISP)
Person Centered Principles
“NOTHING ABOUT ME
WITHOUT ME!”
Client Demographic Growth for Hawaii Developmental
Disabilities Division
1994
1998
2001
2004
2005
2008
1,564
2,438
2,776
3,084
3,259
3,586
CATCH THE WAVE!
Skyrocketing DEMAND for Services
Litigation Impact: Persons with ID/DD live supported in their community.
Traumatic Brain Injury requests are rising
Diagnosis of Autism in Hawaii is growing
Autism rates increased 269% in 10 years in California’s Dept. of Dev. Disability
BUT STATISTICS ARE DECEIVING !
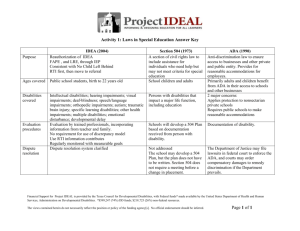
Disability
Mental Retardation
Hearing Impairments
Speech or Language Impairments
Visual Impairments
Emotional Disturbance
Orthopedic Impairments
Other Health Impairments
Specific Learning Disabilities
Deaf / Blindness
Multiple Disabilities
Autism
Traumatic Brain Injury
Developmental Delay
Total
Special Education Child Count
Dec. 2001 Dec. 2000
2412
460
1943
2723
423
2519
85
3229
123
1591
10698
3
88
3442
166
1426
10752
3
354
494
68
2066
23526
337
364
65
1643
23951
Data source: State Hawaii Dept of Education
Autism Epidemic?
1985: 1 in 2,500 children for ASD
2007: 1 in 150 children with ASD
Transition to Adulthood
Adult physician providers are good at adult disease management
Adult physician providers comfortable with certain disabilities commonly seen through adulthood
Cerebral Palsy
Gastrostomy
Seizure disorders
Difficulty of communication with affected individual problematic
Change from child mental health providers to adult mental health providers
Transition from
Pediatrics to Internal
Medicine
Adult physician providers not comfortable with traditionally Pediatric entities
Spina bifida
Autism
Many genetic disorders
Prader-Willi Syndrome
Williams Syndrome
Neuronal migration Disorders
Mitochondrial disorders
Metabolic Disorders
Fragile X
Transition from
School to Work
Individualized Education Plans
(IEPs) now with transition planning from age 14 or younger for adult life
College?
Vocational training
Independent and semiindependent living
Scenario #1
21 year old female with severe cerebral palsy and mental retardation does not want to leave her home for physical checkups.
Her fingernails and toenails are several inches long. She has recent weight loss.
What kind of physician should handle this situation?
Scenario #2
8 year old male with autism is hitting his mother at home. His father left the home two years ago.
His school does not feel that the aggressive behavior at home is their issue - his behavior is fairly well controlled in school with two aides (in addition to the special education teacher and school based behavioral health specialist).
Scenario #2
He has a 3 year old brother.
How would you support this mother with her 8 year old child with autism with aggressive behavior?
Scenario #3
A family has a child with Pervasive
Developmental Disorder. They are requesting gourmet burgers and other foods as a special diet be paid through the DD Waiver.
The financial office of the State DD agency is asking your advice on what to do about this and other diet requests
(most commonly casein and gluten free diets), that are not covered by most insurance plans
Scenario #4
A 7 year old child on Maui has moderate mental retardation and visual impairment. She has a difficult to treat seizure disorder, with many breakthrough seizures that are not clinically evident on video EEG.
She is being home schooled, although the
Department of Education has an ongoing hearing to have the child be placed in a schoolbased program. Teachers and therapists currently go to the home.
Scenario #4
An out of State Child Neurologist relates that the child needs 24 hour 7 day a week nursing care. The nurses rarely administers prn medication and does not provide much care except routine medication administration.
The State agency wants your opinion on the need for this level of nursing care, which is expensive.
Clinical
Interdisciplinary
Team
In Hawaii, several expert disciplines supported individuals in institutional care (Waimano
Training Hospital and School)
With de-institutionalization, these individuals needed to use community resources with case managers (mostly social workers) coordinating care
Improves behavior thru PBS
Need for Clinical
Interdisciplinary
Team
Eligibility (esp. for complex cases)
Technical aspects of eligibility
Psychometrics
Medical diagnoses
Supports for Case Management
Evidence based Practice standards
Coordination with Psychiatry/
Psychology for behavioral support
Access to Specialty Care
Current Hot Issues
Person-centered planning
The individual makes decisions
Living arrangements/ caregivers
Diet, Dental, Medical choices
Residence, medication, physical restraints for people with DD who are violent to themselves or others
Managed Care: Cost Containment
Quality Framework from CMS
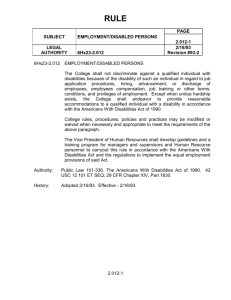
The ADA: the State’s Obligation
Americans with Disabilities Act, 1990
Title II : covers services & programs
A qualified individual cannot be excluded on the basis of disability
Most integrated setting Supreme Court decisions on the ADA -
Bragdon v. Abbott, 1998; HIV
L.C., E.W. v. Olmstead, 1999; cognitive
Reasonable accommodations required
Title II of the ADA
…no qualified individual with a disability shall, by reason of his disability, be excluded from participation in, or be denied benefits of the services, programs, or activities of a public entity, or be subjected to discrimination by any such entity…
Department of Justice
Regulation:
A public entity shall administer services, programs, and activities in the most integrated setting appropriate to the needs of qualified individuals with disabilities. [28 CFR
Section 35.130(d)]
Olmstead v. L.C.
Supreme Court decision in
Olmstead v. L.C. (119 S. Ct.
2176) —the Americans with
Disabilities Act (ADA).
ADA prohibits states from institutionalizing persons with disabilities and from failing to serve them in the most integrated setting.
What is Olmstead?
A June, 1999 Supreme Court decision that has created a mandate for choices for individuals with disabilities
It creates an “even hand” in state programs to allow a continuum of choices in where people live and receive services
Tommy Olmstead, Georgia
Department of Human Resources
Commissioner
L.C. and E.W. in Olmstead
Two women--Lois Curtis
(L.C.) and Elaine Wilson
(E.W.) —with mental illness and mental retardation were confined in a
Georgia state psychiatric hospital.
What Did the Court Say
About Integration?
(a) institutional placement of persons who can handle and benefit from community settings perpetuates “unwarranted assumptions” that persons so isolated are incapable or unworthy of participating in community life.
(b) Confinement in an institution severely diminishes the everyday life activities of individuals, including family relations, social contacts, work options, economic independence, educational advancement, and cultural enrichment.
Current Policy of the
United States
All People With Disabilities Are
Viewed as Capable Of Growth
And Development And Shall
Have The Full Opportunity For
Normal Everyday Experiences
With People Without Disabilities.
DD Act of 2000
DD Act of 2000: Bill of Rights
USC Title 42, Chapter 144, Subchapter 1 Part
A, Section 15009
Community Integration Mandate
Meet Minimum Standards for Appropriate and
Sufficient Medical and Dental Care
Prohibition of the use of physical restraint… unless absolutely necessary to ensure the immediate safety…
Effective: October 30, 2000
In addition to constitutional rights for all