Digestive - Florida International University
advertisement

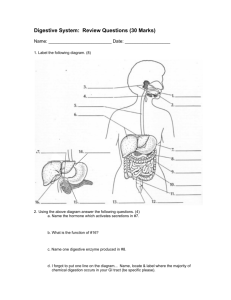
Functional Human Physiology for the Exercise and Sport Sciences The Gastrointestinal System Jennifer L. Doherty, MS, ATC Department of Health, Physical Education, and Recreation Florida International University Overview of Gastrointestinal System Function Digestion Absorption Secretion Motility Organs of the Gastrointestinal System The alimentary canal Continuous hollow tube extending from the mouth to the anus Called the gastrointestinal (GI) tract as is passes inferior to diaphragm Functions: Digestion Absorption of digested fragments into blood Organs of the Gastrointestinal System Accessory organs Assist in the chemical process of digestion by secreting saliva, enzymes, and bile Salivary glands Pancreas Liver Gallbladder Assist in the mechanical process of digestion Teeth Tongue Digestion The process mechanically breaking down food into particles small enough to be absorbed through cell membranes Two methods of food breakdown Chemical Mechanical Digestion: 5 Integrated Steps (1) Ingestion (2) Propulsion Foodstuff enters the GI tract via the mouth The process that moves foodstuff through the GI tract via coordinated reflexive contraction activity (3) Digestion The process of breaking down large food particles into smaller particles via chemical and mechanical action Digestion: 5 Integrated Steps (4) Absorption The movement of digested end products through the intestinal wall and into the blood or lymph End products include small organic molecules, electrolytes, & H2O (5) Defecation The process of discharging undigested and unabsorbed foodstuff The GI Tract The Gastrointestinal Wall 4 layers (1) Muscosa Lamina propria Muscularis mucosa (2) Submucosa (3) Muscularis Externa (4) Serosa Mucosa Inner most mucous membrane Lines lumen Composed of simple columnar epithelium Contains many mucus secreting goblet cells Mucosa Lamina propria Underlying loose CT Contains blood vessels, sensory nerve endings, lymph vessels, and scattered lymph tissue Muscularis mucosa Layer of smooth muscle Produces local movements that change the shape of the lumen Mucosa Functions: Protect underlying tissue Absorb digested material Secrete mucous or digestive juices Increase surface area Folds in the mucosa Villi present in the small intestine Submucosa Composed of loose CT Contains blood vessels and lymphatics Function to circulate absorbed nutrients Contains nerves from the ANS Form the submucosal plexus A component of the intrinsic nervous system of GI tract Muscularis Externa Composed of two layers of smooth muscle Inner layer - circular fiber arrangement Outer layer - longitudinal fiber arrangement Muscularis Externa Inner layer - circular fiber arrangement When fibers contract = ↓ lumen size Forms sphincter muscles Prevent backflow of materials Outer layer - longitudinal fiber arrangement When fibers contract = mix and propel food along the alimentary canal Muscularis Externa Myenteric plexus Extensive nerve network between the smooth muscle layers Regulate motility Movement/contraction of the GI tract walls Regulate glandular secretions Secretions into the lumen of the GI tract Serosa Outermost layer of the GI wall Inner layer Outer layer - Mesothelium Consists of fibrous CT Provides structural support Consists of epitelium Secretes a water lubricating fluid allowing organs to slide past one another Peritoneal Cavity The space between the visceral peritoneum and parietal peritoneum Both visceral and parietal peritoneum secrete serous fluid into the peritoneal cavity Lubricates and protects abdominal tissues as they slide past one another GI Motility Patterns Contractions of the muscularis externa Two methods Peristalsis Segmentation GI Motility Patterns Peristalsis Propelling motion produced by alternate waves of contraction and relaxation of muscularis externa layer Occurs due to contraction of one part of wall with simultaneous relaxation of the wall ahead Propels food along tube GI Motility Patterns Segmentation Occurs due to rhythmic, local contractions of the smooth muscle in the muscularis externa layer Mechanically grinds foodstuff in the stomach and intestines mixing it with digestive juices Gastrointestinal Regulation Intrinsic Control Submucosal Plexus Myenteric Plexus Extrinsic Control Parasympathetic nerve fibers Sympathetic nerve fibers Gastrointestinal Regulation: Intrinsic Control Provided through the Submucosal Plexus Myenteric Plexus Local stimulus = distension of submucosa or muscularis externa walls Local response = activation of stretch receptors ↑ glandular secretions ↑ smooth muscle contractions in the immediate area Gastrointestinal Regulation: Extrinsic Control Includes Parasympathetic and Sympathetic input from the ANS Fibers within the muscularis externa layer specifically assist in controlling the rate and strength of contractions Gastrointestinal Regulation: Extrinsic Control Parasympathetic activity Impulses carried by the vagus nerve ↑ motility ↑ glandular secretions Gastrointestinal Regulation: Extrinsic Control Sympathetic activity Opposes parasympathetic activity ↓ motility ↓ glandular secretions Causes sphincters to contract thus slowing the movement of foodstuff through the GI tract Digestion: 5 Integrated Steps (1) Ingestion (2) Propulsion (3) Digestion (4) Absorption (5) Defecation Digestive Function: Ingestion The digestive process begins in the mouth Includes… Mechanical fragmentation of foodstuff Foodstuff mixes with saliva Digestive Function: Ingestion Organs and associated structures Tongue Mixes foodstuff with saliva during chewing Initiates swallowing Contains taste buds Sensitive to chemical differences among food molecules Differentiate sweet, sour, salty, or bitter tastes Digestive Function: Ingestion Organs and associated structures Teeth Tear and grind food Mastication Mechanical breakdown of foodstuff into smaller fragments Digestive Function: Ingestion Organs and associated structures Lips and Cheeks Keep food in mouth Involved in speech Digestive Function: Ingestion Organs and associated structures Palate Forms roof of mouth 2 distinct parts Hard Palate Soft Palate Digestive Function: Ingestion Organs and associated structures Hard palate Anterior region composed of bone Forms a hard surface against which foodstuff is pushed during chewing Soft palate Posterior region composed of skeletal muscle Rises reflexively to close off nasopharynx during swallowing Digestive Function: Ingestion Organs and associated structures Salivary glands - 3 pairs 1). Parotid glands 2). Submandibular glands Largest salivary glands Anterior to the ears Inferior to the jaw 3). Sublingual glands Inferior to the tongue Digestive Function: Ingestion Organs and associated structures Saliva Produce 1 - 1.5 L/day Basic composition Water (98 - 99%) Salivary Amylase: a digestive enzyme Mucins: mucous that lubricates the mouth and food Ions, buffers, metabolites, antibodies, etc Dissolves foodstuff Digestion: 5 Integrated Steps (1) Ingestion (2) Propulsion (3) Digestion (4) Absorption (5) Defecation Digestive Function: Propulsion Swallowing Reflex response which moves foodstuff through the pharynx and down the esophagus The swallowing reflex is triggered when material moves into the pharynx Digestive Function: Propulsion Components of the swallowing reflex: The soft palate rises The epiglottis covers the opening of the larynx Prevents foodstuff from entering the air passageways Peristaltic contractions along the pharyngeal and esophageal walls propel foodstuff through the GI tract Relaxation of lower esophageal sphincters allows foodstuff to enter the stomach Digestive Function: Propulsion Esophagus A muscular tube which collapses when it is not in use Contains 2 sphincters Upper esophageal sphincter Lower esophageal sphincter The sphincters contract to prevent the backflow of stomach acids into the esophagus Digestive Function: Propulsion Both the pharynx and the esophagus are only passageways for foodstuff Peristalsis The pharynx and the esophagus are not directly involved in digestive activities Digestion: 5 Integrated Steps (1) Ingestion (2) Propulsion (3) Digestion (4) Absorption (5) Defecation Digestive Function: Digestion Saliva Dissolves foodstuff via chemical processes Contains salivary amylase Chemical breakdown of starches Allows food to be tasted Moistens foodstuff and converts it into bolus Mass of moistened food that can be easily swallowed Digestive Function: Digestion Control of Salivation Regulated by both the PNS and SNS Receptors in mouth send signals to brain Controlled primarily by the PNS Causes ↑ salivation Rate of secretion and composition of saliva changes in response to… sight, sounds, smells, pressure of food in mouth Digestive Function: Digestion Stomach Stores foodstuff Gradual delivery to the small intestine Mixes foodstuff with gastric juices Initiated the digestion of proteins Digestive Function: Digestion Stomach Protein digestion occurs via pepsin Enzyme that breaks down proteins into smaller polypeptide and amino acid fragments Protein digestion is the only type of chemical digestion occurring in stomach Digestive Function: Digestion Stomach Foodstuff mixed with gastric juices forming a creamy paste called Chyme Chyme is passed out of the stomach into the small intestine Limited absorption occurs in the stomach Absorb small amounts of H2O, glucose, salts, alcohol, and lipid-soluble drugs The Stomach Distends to accommodate foodstuff Empty stomach Full stomach Walls collapse forming folds (rugae) in the inner lining Rugae smooth out Able to hold 1 - 1.5 L of foodstuff The Stomach Regions of the stomach Body - large, main portion of stomach Cardiac region - surrounds opening where esophagus enters the stomach Fundus - domed-shaped region that projects above the cardiac region Serves as a storage area The Stomach Regions of the stomach Pylorus - exit Antrum (pyloric antrum) - funnel-shaped region near the pylorus Pyloric canal - narrow region terminating at the pylorus Pyloric sphincter - controls stomach emptying The Stomach Modifications of the Stomach Wall The muscularis layer is modified according to the functions of the stomach Greater churning/mixing ability Mechanical breakdown of foodstuff into smaller pieces Composed of 3 layers Circular Longitudinal Oblique layer - additional innermost layer The Stomach Modifications of the Stomach Wall The mucosa layer contains gastric pits Gastric pits lead into gastric glands Millions of pockets in the epithelium Gastric glands are located deep in the lamina propria Gastric glands produce gastric juices Stomach secretions Gastric Glands 4 types of gland cells: 1) Chief cells Zymogenic cells 2) Parietal cells Oxyntic cells 3) Mucous neck cells 4) Enteroendocrine cell Gland Cells: Chief cells (Zymogenic cells) Secrete pepsinogen Inactive form of pepsin Protein-digesting enzyme Activated by stomach acids Also secrete gastric lipase Fat-digesting enzyme Not very active in stomach due to low pH Main action is on butter fat Gland Cells: Parietal cells (Oxyntic cells) Secretes HCl HCl is a strong acid that ↑ the acidity of the stomach (pH = 1.5 - 3.5) Activates pepsin Also secretes Intrinsic factor Required for vitamin B12 absorption in the small intestine Only stomach function essential for life Gland Cells: Mucous Neck Cells Secretes alkaline mucous Protects stomach lining from… Damaging acidity in the stomach Damaging action of protein-digesting enzymes Gland Cells: Enteroendocrine Cells Secrete a variety of compounds directly into the lamina propria These compounds then diffuse into blood capillaries Function as local hormones to regulate the functions of various digestive organs i.e.) Gastrin – regulates the stomach Gland Cells Gastric juices do not digest the walls of the stomach due to… The mucous barrier is alkaline Mucous barrier Epithelial cells Neutralizes acid on the stomach lining Tight junctions between epithelial cells prevent acid from leaking to underlying tissue Rapid turnover of epithelial cells Replaced every 3 days Regulation of Gastric Secretion Neural control Parasympathetic input Conducted via the vagus nerve Increases secretion from all gastric gland cells ↑ Pepsin concentration in stomach ↑ HCl concentration in stomach ↑ Gastrin concentration in stomach Regulation of Gastric Secretion Neural control Sympathetic input Overrides Parasympathetic input Inhibits gastric gland secretion ↓ Pepsin concentration in stomach ↓ HCl concentration in stomach ↓ Gastrin concentration in stomach Occurs during times of… Physical activity Emotional stress Regulation of Gastric Secretion Hormonal control Provided primarily by Gastrin Increases secretion from all gastric gland cells ↑ Pepsin concentration in stomach ↑ HCl concentration in stomach ↑ Gastrin concentration in stomach Three phases of gastric secretion Occur almost simultaneously Phases of Gastric Secretion 1). Cephalic phase (Reflex phase) Triggered by sight, smell, thought, or taste of food Sensory input is relayed to hypothalamus Vagus nerve sends impulses to gastric glands Sensory input is integrated in hypothalamus Vagus nerve is stimulated Increase secretions from all gastric gland cells Prepares the stomach in advance for the arrival of foodstuff Phases of Gastric Secretion 2). Gastric phase Begins when foodstuff reaches the stomach Stimulation of the vagus nerve occurs due to 2 stimuli a). Distension of stomach walls b). Chemical stimuli Stimulation of stretch receptors Provided by partially ingested foodstuff Increase secretions from all gastric gland cells Phases of Gastric Secretion 3). Intestinal Phase Purpose = control the rate of gastric emptying Provides the small intestine with enough time for digestion and absorption Phase begins when chyme enters the duodenum First portion of the small intestine Phases of Gastric Secretion 3). Intestinal Phase cont. Presence of foodstuff in the stomach stimulates the release of intestinal gastrin Hormone similar to gastrin Increase secretions from all gastric gland cells Helps speed digestion in the stomach before stomach-emptying is complete Released only when stomach begins to empty Inhibition of Gastric Secretions Can be accomplished via… Emotional upset Sympathetic innervation The rate of gastric secretion may also be inhibited by the… Stomach Small intestine Inhibition of Gastric Secretions Gastric secretion may be inhibited during the gastric phase Gastric secretion decreases when the mucosa becomes too acidic (pH < 2) Slows the rate of further gastric secretion Occurs as the stomach empties and buffering capacity of food material decreases Inhibition of Gastric Secretions Gastric secretion may be inhibited during the intestinal phase Most regulatory controls during the intestinal phase are inhibitory Duodenum responds to various stimuli through the enterogastric reflex Inhibition of Gastric Secretions Enterogastric reflex This is an inhibitory reflex in the small intestine that slows gastric secretions Stimuli Distension of the duodenum Presence of acidic (H+) and/or hypertonic chyme Presence of fats, partially digested proteins, and/or irritants Inhibition of Gastric Secretions Inhibitory effects: enterogastric reflex PNS input to the stomach mucosa SNS input to the pyloric sphincter Prevents additional foodstuff from entering the small intestine gastric motility hormone release from the small intestine, which inhibits gastric secretions Digestive Function: Digestion Mechanical Digestion and Propulsion Mechanical digestion is achieved through contractile activity of the stomach Propulsion is achieved through peristalsis and segmentation Mechanically mix and breakdown foodstuff Propel chyme from the stomach to small intestine These mechanisms are triggered via distension of the stomach ~ 1 L of food enters Digestive Function: Digestion Mechanical Digestion and Propulsion cont. Peristaltic waves sweep across the stomach toward the pylorus Foodstuff is pushed against the pyloric sphincter, which is normally closed Large food materials are churned and mixed in the stomach until the food particles are small enough to pass through the pyloric sphincter Regulation of Gastric Emptying The rate of gastric emptying depends on the type of food ingested Fluids Pass through quickly 90 minutes Solids Remain in the stomach until reduced to very small particles Remain in the stomach until dissolved in gastric juices 3 - 4 hours Regulation of Gastric Emptying Gastric emptying of nutrients Carbohydrates are emptied first Followed by proteins Fats take the longest to leave the stomach Regulation of Gastric Emptying Dependent upon the duodenum Gastric emptying is regulated along with gastric secretions Stimuli Responses Distention of the wall in the small intestine Presence of acid (H+), fat, or hypertonic solution in the small intestine Trigger the enterogastric reflex ↓ gastric motility Slows rate of gastric emptying Purpose Provides time for the small intestine to digest and absorb foodstuff Small Intestine (SI) Chyme leaves the stomach ~3-4 hours after ingestion Carbohydrates and proteins are partially digested upon entering the SI Too large to be absorbed through SI wall Fats are undigested upon entering the SI Small Intestine (SI) In the duodenum, bile from liver is added to chyme Also in the duodenum, enzymes from pancreas are added to chyme Enteroendocrine Cells in the duodenum also secrete enzymes ***All nutrient absorption occurs in small intestine*** Small Intestine (SI) The SI extends from the pyloric sphincter of the stomach to the iliocecal valve in the large intestine Subdivisions Duodenum Jejunum Ileum Small Intestine (SI) The SI contains ducts that carry bile and pancreatic juices to the duodenum Hepatopancreatic Ampulla A single duct that empties into duodenum Sphincter of Oddi Also called hepatopancreatic sphincter Duct that controls entry of bile and pancreatic juices into duodenum Digestion: 5 Integrated Steps (1) Ingestion (2) Propulsion (3) Digestion (4) Absorption (5) Defecation Digestive Function: Absorption Anatomy of the SI Plicae Permanent transverse folds in mucosa & submucosa layers Villi Function to increase the surface area Increased surface area = Increased absorption Finger-like projections in mucosa layer Microvilli Finger-like projections on the lumenal surfaces of mucosa cells Digestive Function: Absorption SI Secretions: Intestinal juice A watery secretion with neutral pH (7.0) Serves as a medium for digestion and absorption of nutrients Glands normally secrete ~1-2 L/day Stimuli for secretion Distension of SI walls due to the presence of chyme Irritation of SI mucosa caused by hypertonic or acidic chyme Digestive Function: Absorption SI Secretions: Digestive enzymes Disaccharidases Carbohydrate digestion: breakdown disaccharides into monosaccharides Peptidases Secreted by epithelial cells in the SI Protein digestion: breakdown polypeptides into amino acids Lipases Fat digestion: breakdown fats into glycerol and fatty acids Digestive Function: Absorption Gastric Secreting Gland Cells Goblet cells Located in the mucosal epithelium of the SI Secrete alkaline mucous Enteroendocrine cells Secrete local hormones to regulate activity of the SI Intestinal Glands Location At base of villi in intestinal crypts Secrete intestinal juices A watery mixture with neutral pH (7.0) Glands normally secrete 1 - 2 L/day Function Serves as medium for digestion and absorption of nutrients Stimuli Distension of SI walls due to the presence of chyme Irritation of SI mucosa caused by hypertonic or acidic chyme Intestinal Glands Specialized structures located in submucosa Peyer's patches Collections of lymph tissue Preventing bacteria in undigested food from entering the systemic circulation Brunner's glands Only located in the initial part of duodenum Secrete alkaline mucous Protects duodenal walls by neutralizing the acidic chyme entering the SI from the stomach Regulation of Intestinal Secretions Stimuli to ↑ intestinal secretions Presence of chyme in duodenum Distension of SI walls Stimuli elicits a response from the Parasympathetic nervous system Impulses carried via vagus nerve Results in the secretion of… Alkaline mucous Digestive enzymes The Pancreas Both endocrine and exocrine function Endocrine Function Alpha cells release glucagon Beta cells release insulin Exocrine Function Acinar cells Secrete pancreatic juice into the pancreatic duct Watery alkaline fluid (pH = 8) Contains HCO3- and various digestive enzymes The Pancreas Pancreatic Enzymes All are proteolytic or protease enzymes Trypsin, Chymotrypsin, and Carboxypeptidase Protein-digesting Require alkaline environment Provided by HCO3- Pancreatic Enzymes Secreted in inactive form Activated in the duodenum Pancreatic amylase Breaks down almost all carbohydrates Pancreatic lipase Prevents self-digestion of pancreas Breaks down fats Pancreatic nuclease Breaks down nucleic acids Regulation of Pancreatic Secretion Begins during the cephalic and gastric phases of gastric secretion via PNS activation Major stimulus for secretion is… Presence of chyme in the duodenum Occurs during the intestinal phase Regulation of Pancreatic Secretion Chyme in duodenum stimulates the secretion of… Secretin Cholecystokinin (CCK) Targets duct cells to secrete watery alkaline fluid Targets acinar cells to secrete pancreatic juice containing digestive enzymes Pancreatic secretions trigger the enterogastric reflex The enterogastric reflex slows gastric emptying The Liver Liver is the largest visceral organ Blood circulation in the liver O2 blood delivered via hepatic artery Nutrient-rich blood delivered via hepatic portal vein from the intestines Blood from these 2 sources mixes as it flows through the liver sinusoids Blood leaves the liver via central veins --> hepatic veins --> heart The Liver Functions: Contributes to blood maintenance Phagocytosis Pathogens and old RBCs Synthesize plasma proteins Detoxify drugs and poisons Metabolic regulation Aids in digestion Synthesis and secretion of bile Bile Yellow-green alkaline solution Composition Water Bile salts Synthesized in the liver from cholesterol Function: Emulsification of fat globules Mechanical break down of fat globules into small droplets Small droplets have larger surface area thus allowing lipases to act more effectively Bile Pigments Biliverdin Metabolized by bacteria in SI Exit body in feces (gives brown color) Metabolized by bacteria in SI Exit body in feces (gives brown color) Aid in digestion Phospholipids Bilirubin Bile salts Aid in digestion Lecithin Cholesterol Neutral fats Electrolytes Bile Pathway Bile exits the liver via canaliculi Tiny bile canals Bile ducts from the liver join together to form the common hepatic duct Extends downward toward the duodenum Bile Pathway Cystic duct from the gall bladder joins common hepatic duct as well Common bile duct Forms the common bile duct Joins with the pancreatic duct via the hepatopancreatic ampulla Pancreatic Duct Empties bile and pancreatic juices into the initial portion of the duodenum Sphincter of Oddi guards this entry into duodenum Gallbladder Small green sac located on the inferior surface of the liver Concentrates and stores bile Does not synthesize bile Sphincter of Oddi When closed, bile cannot enter duodenum Bile is then stored in the gallbladder Regulation of Bile Release Bile release from the gall bladder into the duodenum… The presence of fat and protein in the duodenum stimulates the secretion of Cholecystokinin (CCK) Targets acinar cells to secrete pancreatic juice containing digestive enzymes CCK stimulates the gallbladder to contract and sphincter of Oddi to relax Results in bile release into the duodenum Digestive Function: Digestion and Absorption The SI is the major site of digestion and absorption Requires that chyme be mixed with… Bile, and Digestive enzymes Necessary to expose foodstuff to the SI mucosa for absorption Digestive Function: Digestion and Absorption Segmentation Begins as soon as chyme enters the SI Do not propel chyme onward Peristalsis Propels chyme onward Requires time to move chyme Allows more time for digestion and absorption Digestion and Absorption of Major Nutrients Carbohydrates (CHO) Amylase Salivary amylase Began CHO digestion in mouth Pancreatic amylase Continues digestion of CHO in the SI Digestion and Absorption of Major Nutrients Carbohydrates (CHO) Glucose is the major end-product of CHO digestion Cellulose and other indigestible CHO provides dietary fiber Cannot be digested by humans Passed to the large intestine Simple sugars are absorbed across intestinal mucosa of the SI Digestion and Absorption of Major Nutrients Proteins (PRO) In Stomach Dietary PRO is initially broken into smaller polypeptide fragments by pepsin In Small Intestine Trypsin and chymotrypsin are enzymes from pancreas that further break down polypeptides into smaller fragments Digestion and Absorption of Major Nutrients Proteins (PRO) Complete PRO digestion occurs in the SI via the following enzymes… Carboxypeptidase (from pancreas) Peptidases (from SI) Final breakdown products are amino acids Absorbed in the SI and travel to the liver via the hepatic portal vein Digestion and Absorption of Major Nutrients Fats (Lipids) The SI is basically the only site of fat digestion Triglycerides (TG) are the most abundant dietary fat As TGs enter the SI they are emulsified by bile salts Emulsification droplets Pancreatic lipase Enzyme that breaks down TGs into… 2 free fatty acids (FFA) 1 monoglyceride (glycerol) Digestion and Absorption of Major Nutrients Fats (Lipids) FFAs and Glycerides interact with bile salts to form micelles Fatty elements clustered around bile salts for the purpose of increasing solubility Micelles enhance fat absorption in the SI Once absorbed, 2 FFAs and 1 Glycerol form a TG Digestion and Absorption of Major Nutrients Fats (Lipids) TGs then combine with other lipid material to form chylomicrons Water-soluble lipoprotein droplets that are processed in the cell Chylomicrons are secreted into interstitial fluid Carried by lacteals through the lymphatic system Ultimately enter the systemic circulation Digestion and Absorption of Major Nutrients Fats (Lipids) Chylomicrons are present in the systemic circulation Systemic capillaries contain lipoprotein lipase Enzyme that breaks down TGs into… 2 FFA 1 Glycerol FFAs and Glycerol may then diffuse out of the blood and into cells Used for energy, or Stored as fat Digestion and Absorption of Major Nutrients Vitamins Fat-soluble vitamins (A, D, E, K) Bind to ingested lipids Absorbed with lipids via lacteals Water-soluble vitamins Mostly absorbed with water Exception - vitamin B12 Must bind with intrinsic factor, which is produced by parietal cells located in the stomach Absorbed via endocytosis Digestion and Absorption of Major Nutrients Electrolytes Na+ and Cl K+ Absorbed via active transport Absorbed via passive diffusion H 2O Absorbed via osmosis Moves freely across intestinal mucosa Digestion: 5 Integrated Steps (1) Ingestion (2) Propulsion (3) Digestion (4) Absorption (5) Defecation Digestive Function: Defecation The Large Intestine 2 major regions Colon Rectum Digestive Function: Defecation The Colon The largest portion of the large intestine Extends from the ileocecal valve to the rectum Subdivisions: Ascending colon, Transverse colon, Descending colon, and Sigmoid (S-shaped) colon Digestive Function: Defecation The Rectum Distal portion of GI tract Includes last 6" of large intestine Extends to anal canal Opens to the exterior of body at the anus Sphincters Internal sphincter External sphincter The Large Intestine (LI) Anatomical Modifications Mucosa contains many goblet cells No villi or microvilli Alkaline mucosa Holds feces together Protects the lining of the large intestine Longitudinal muscle layer arranged in 3 bands Produces out-pocketings of the LI wall Called haustra The Large Intestine (LI) Motility Patterns (1) Haustral churning Similar to segmentation in the SI Local contractile activity mixes chyme Places chyme close to the haustra Facilitates absorption of water (2) Peristalsis Very sluggish Contributes little to movement of chyme The Large Intestine (LI) Motility Patterns cont. (3) Mass movements Powerful peristaltic waves Pass over large areas (8" segments) of the colon ~ 3 times/day Responsible for… Moving foodstuff to the rectum Producing the urge to defecate The Large Intestine (LI) The LI has limited digestive and absorptive function… Digestion: the lumen contains millions of bacteria Metabolize remaining nutrients Produce gases Hydrogen, methane, CO2, hydrogen sulfide Absorption: limited Some vitamins, electrolytes, & H2O Digestive Function: Defecation Feces are forced into the rectum via mass movements This causes distension of the LI wall Triggers the defecation reflex Digestive Function: Defecation Regulation of the defecation reflex is provided by centers in the sacral cord Stimulates… Contractions in rectum and distal LI Relaxation of internal anal sphincter Input to the cerebral cortex allows decision regarding appropriate behavior Relaxation of both the external and internal sphincter if appropriate Digestion: 5 Integrated Steps (1) Ingestion (2) Propulsion (3) Digestion (4) Absorption (5) Defecation