resprog/internalmedicine/Manuals/Inpatient Third
advertisement

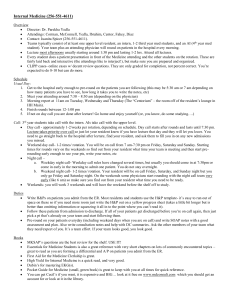
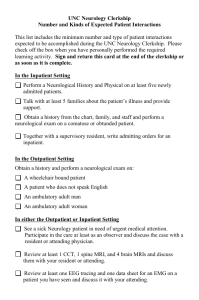
Inpatient Internal Medicine Clerkship Orientation-Good Sam Welcome! We are excited to have you here with us and expect your rotation to be filled with interesting patients, great expansion of your knowledge of Internal Medicine, meeting residents and forming friendships. If you have any questions, please feel free to contact Dolores Castro clerkship coordinator (602-8395961 Dolores.Castro@bannerhealth.com), or your outpatients clerkship director Keri Lyn Gwisdalla, M.D. (pager 602-201-5069) or your inpatient clerkship director Kendall Novoa-Takara, M.D. (pager 602201-0921, Kendall.novoatakara@bannerhealth.com). The chief residents are here to help you as well. They remember what it was like to be a medical student and they will try to answer any questions you may have. Our website, www.goodsamim.com, has information pertaining to our program, along with the medical student curriculum guide and forms which you will need during your clerkship with us. Handy References: Some of these can fit in your coat pocket and will be helpful to you while working up patients, waiting for rounds, etc. Pocket Medicine: The Massachusetts General Hospital Handbook of Internal Medicine (Sabatine) Pocket Pharmacopoeia or Epocrates for your Palm Pilot (practically a must-have!) UpToDate: available on every computer here, just go to www.utdol.com www.goodsamim.com: Schedules and forms are housed on our website under “For our medical students”. The username/password is gsphoenixim. This is also where you will find the reading for academic half day. Click on ‘Learning’ on the left hand side of the screen and the month under Academic Half Day to find the assigned articles. Internal Medicine Essentials: 39.95 for ACP student members (student membership in ACP is free) or 49.95 for non-members. There is one copy in the library in the workroom (not to be checked out and you have to ask for it). Student Responsibilities Participate fully and actively in all of the activities of the team-know (peripherally) and examine ALL patients on the team’s service Work up and follow patients as assigned by the resident (MS III usually 1 per admitting day/ 3-5 per week, MSIV 1 new patient per admitting day and 3-5 patients daily) Pre-round on all patients before management rounds Know your patients inside and out Present patients on rounds Perform and document H&P including the assessment and plan on all new admissions and to present these to the faculty attending within 48 hours of admission (MSIV should be prepared to present the same day) Write daily SOAP progress notes on all patients assigned (must be reviewed by intern/resident) Order writing may be practiced on paper and reviewed with an intern or resident Personally follow up on every study that is ordered on your patient See your patients again in the afternoon Evening reading about your patients Logistics (AKA about Good Sam) There are maps of the hospital available down in the department of Medicine. All numbers to our hospital begin with the prefix 839-####. While in house, you can call any extension from any phone by dialing 1-####. For example, 1B is 839-2124, so in house you can dial 1-2124. Sometimes when you get paged, you will see a four digit number after the extension. This is usually the last four digits of the pager number of the person who paged you. You will receive a password to Cerner in order to access information on your patients’ labs, discharge summaries, reports, etc. scrub cards-see Medical Education Parking-see Medical Education You may wish to familiarize yourself with the hospital policies. These can be found by clicking on the internet icon on any computer here (the “home” page) then choosing “resources” on the left side tool bar. These policies can aid you in patient care (infection control, restraint use, ethics, etc.) You do NOT need to read every one; this is just a resource if you need it. Your first day Report to Dolores in medical education at 8 am. Orientation will be with Dr. Kendall Novoa-Takara at noon. Check with Dolores for time. During the morning ID badges, scrub cards and pagers will be issued. Computer training is done before you start your rotation but we will have you test the computer codes on the first day. If your computer code does not work, DO NOT allow the residents to send you home early as there is much you can learn even without access to the computer! Page your resident and meet the team upon completion of all of the above. We no longer have noon conference so you may be able to eat lunch with your team. You MUST pick up a patient on your first day. Please email the name and dx of the patient to Dr. Novoa-Takara before you leave the hospital. If you are assigned team to the night team, MSIVs may leave and return at 6 pm to take call with the team until 10 pm. MSIIIs assigned to the night team may leave after the computer orientation and will return on Tuesday night after their afternoon lectures. If you are on nights the first week you MUST try out your computer passwords and ensure that they are working before you leave the hospital. A typical day (INPATIENT wards) Arrive at the hospital usually around 6 am. You want the first chance at seeing, examining, and determining a plan for the day on your patients. You need to know everything about your patients. Be sure to check the chart—look at the previous day’s notes for consultant’s notes and cross cover notes that were put in after you left as well as the current day. Be sure to look at their vitals, review the med list, cultures, labs and studies. Call your intern to check in after you have seen your patients (sooner if they look sick!) They may have new patients for you to see. Write your notes and sign them before attending rounds. Be sure to send the note to your resident. Discuss your patients with your resident BEFORE morning report and attending rounds 11-11:30 am (Mon,&Wed) 11-12 on Thurs Morning Report, Conference Room C (Mandatory) 9:15am – 12:30pm Tuesdays AHD, Amphitheater. Come prepared with knowledge of the subject being discussed (i.e., do the assigned reading found on goodsamim.com; if the reading is not posted on the website, ask your resident as some articles get emailed out). Work Rounds/Teaching Rounds before Am report, exact time determined by attending some will start at 8 others later. PM Academic Half Day for MSIII: This occurs on Tuesday afternoons and is your core curriculum. We understand you have a big time commitment to the lecture series. The residents understand this, but if for some reason there is a problem, please let us know. Return back to check on your patients (what has happened during the day). After lecture, call your team to let them know you are done and if there are new patients you should see. 8-9 am (Fridays only) Grand Rounds, Amphitheater (Mandatory) MSIV (accompanied by resident) will sign out their patients at night to the call team You are encouraged to go to any and all Journal Clubs, Happy Hours, etc Flow Rounds vs Typical Rounds Typical rounds: you come in early, see your patients and review their charts, you discuss with your resident and then your team with meet with the attending later and discuss patients. Flow rounds: a new concept which might be confusing for both housestaff and students. With flow rounds, the residents and students do not have time to preround on everyone before they meet with the attending at bedside. With flow rounds, residents and students are literally expected to be one patient ahead of the attending. Example: each team has an A side and a B side. The attending will start with the first patient on the A side. The intern and student will have a 30 minute period before the attending meets them at bedside. During this time the intern and student should review the chart, see the patient, and start writing their note on that patient. The attending and resident will come at the appointed time and the intern or the student will present at bedside. The intern and student should come up with a tentative plan, the resident and attending will discuss the plan at bedside and make any changes to the plan right then and there. A workstation on wheels should be taken into the room so orders can be entered immediately. Interns and students will finish their notes and then move on to the next patient the attending will see with them. While the resident and attending have been seeing the patient on the A side, the B side intern and student are seeing the next patient that the resident and attending will see. Some teams will be doing only flow rounds and others may be doing a hybrid—seeing the sickest patients, new patients, or patients being discharged on flow rounds. Ask your team how they plan on rounding. Flow Rounds Workflow (MEDICAL STUDENT) Philosophy: This style of rounding allows for more efficient and effective patient care and resident education. It also offers more autonomy for housestaff, and more opportunity for direct observation. 6:30am – Arrive 6:30am-7:45am – Pre-round Pre-round on patients you are personally following! o Labs/Images/Vitals/Notes from overnight o Examine patients that you are personally following! This will ensure efficient workflow throughout the day for you, and allow maximal face-to-face education throughout team rounds. Touch base with your senior residents for meeting time/place. This is also a good time to briefly discuss the assessment and plan for your patients with your senior resident. 7:45am – Meet with senior resident(s) and attending to get information for the day, set up a time to discuss outside research you’ve done, and take care of morning incidentals. 8:00am-12:00pm – Team Rounding – Resident and attending meet intern outside patient’s room just after intern has completed patient exam (resident signs into the Workstation On Wheels). Medical students should rotate with the attending, alternating between interns’ lists. This will allow for the most clinical exposure, and the most face-to-face teaching with senior residents and attending physicians. Intern, or medical student if this is a patient that you are personally following, presents brief history, overnight events, significant vitals, labs, other tests, and plan of care to team in room when appropriate. Discuss updates to plan w/senior resident and attending. Inside the Patient Room: Resident examines the patient, attending verifies pertinent findings Discuss plan of care with patient in room 2:00pm – Afternoon Huddle – meet with whole team to review updates, discuss discharge plans for the next day. Medical students should offer to assist with updating “the list” and assist in any additional work to be completed for successful/efficient handoff to night team. Medical Student Tips: Get your resident/intern contact info on your first day working with them. You may need to show up at 6:00am initially to get used to the workflow, but you should quickly be able to adjust to show up at 6:30am. More efficient flow will lead to more study time! Remind the team that you’d like to share the research you’ve done outside of the hospital! Each day you should make notes of interesting treatments/patients/tests/topics that come up, and come with at least one topic that you’d like to share with the team, daily. If something interesting is happening (e.g., patient is getting a stress test, echo, EKG) you should ask to watch how it is done! And, while you’re watching, have the doctor/nurse/technician explain everything they’re doing. A good way is to say “Tell me everything you can about what you’re doing and looking for because right after this my attending is going to ask me what I learned!” Flow rounds may seem stressful at first because it is different, but you will get far more face-toface teaching time and you will find that because it is more efficient you end up with more study time than your colleagues doing standard rounding. Ask to have any interesting findings on physical exam pointed out to you! Then, take the time to really learn from that exam. You won’t always have someone to point out a friction-rub, but if you get a chance to hear one, don’t miss it! H & Ps, Progress notes, and chart documentation Independently perform a comprehensive history and physical examination on patients they admit. Formulate a complete problem list with differential diagnosis on active problems. Formulate diagnostic and treatment plans for active problems. Discuss the history, physical, assessment and plan (complete H&P) with their senior resident on the day of admission. Have H&P signed by the supervising resident. Present each new admission to the attending physician, typically on rounds. H and Ps/Initial Consultation Notes Please note that the H and P should have a FULL REVIEW OF SYSTEMS AND FULL PHYSICAL EXAMINATION (except pelvic, breast and rectal exams unless indicated). The HPI should include: location, quality, severity, timing/duration, context, modifying factors, and associated signs and symptoms. Your review of systems must include at least 10 systems: Constitutional-fever, weight loss, etc Eyes Ears, nose mouth, throat Cardiovascular Respiratory Gastrointestinal Genitourinary Musculoskeletal Integumentary (skin,breast) Neurological Psychiatric Endocrine (with as many diabetic patients as we have, this should never ever be blank in a pt with diabetes) Hematologic/lymphatic Allergic/immunologic NEVER ever should I see in a chart, “all 10 systems negative unless otherwise indicated”. You must fill out a minimum of two things under each system to be given credit for billing purposes (not pertient to you now but when you are a resident it will matter). A thorough past medical history, family history (particularly first degree relatives), and social history is needed. Do NOT say ‘negative’—give details of what was ‘negative’ Your physical exam must include 10 organ systems: Constitutional (vitals, appearance) Eyes Ears,nose, mouth, throat Cardiovascular Respiratory Gastrointestinal Genitourinary Musculoskeletal Skin Neurologic Psychiatric Hematologic, lymphatic, immunological Unfortunately, the computer system does not allow students to write orders. You can write paper admission orders and daily orders which your resident should review. Another opportunity for getting more practice in decision making and management: when you pre-round with the resident, discuss with them your assessment and specific plan (specific medications, dosages, routes as if you were actually writing the order). Students will also write progress notes in the computer, on assigned patients. DO NOT COPY THTE RESIDENT’S OR INTERNS H&P OR NOTES!!!! The student should write their own note and may copy their note forward for subsequent days. A word about documentation in charts-be very careful what you say and how you say it! The chart is a legal document. The chart is read by EVERYONE, including patients, family members, and potentially attorneys. Always give the other party (consulting service etc.) the benefit of the doubt. Chose your words very carefully, be diplomatic. Oral Presentations Use this format when presenting a NEW patient during attending rounds: HPI: ROS: Goals: accurate, chronological, concise, builds an argument Two paragraph method: o Paragraph 1: Chronological history Characterize the pt’s complaint (chronological story); use this to mentally generate & help your listeners to generate a top 5 DDx. o Paragraph 2: Symptoms, risk factors, PMH relevant to the DDx Discuss the Sx/ROS that would argue for/against each item in your DDx. Discuss any risk factors/PMH that would argue for/against each item in your DDx. If pertinent to CC, include in Paragraph 2 of HPI. Otherwise, state here if will be on the problem list. PMH, SHx, FamHx, etc.: Should NOT be a regurgitation of the note (we’ll read that later) If pertinent to HPI/top 5 DDx, discuss in paragraph two of HPI … do NOT need to repeat here (we can remember from the HPI) Otherwise, will we think about it/treat it during this hospitalization? Will it be on the problem list? If so, then state briefly. If not, then leave it for the note. Meds: List names (be prepared to give doses/frequency if asked). Indicate if recent change/problem. Physical Exam: Report positive or negative findings related to most likely diagnosis Report pertinent positive or negative findings that argue for/against other possible diagnoses in top 5 Report any other significant (abnormal) exam findings (will it be on the problem list?) Diagnostic Studies: Report labs/studies that argue for/against the most likely diagnosis Report labs/studies that for/against other possible diagnoses in top 5 Are there any other abnormal labs or studies that we will think/worry about or address? ED Course: It depends but usually discuss right before the A&P (or can talk with your attending about possibly building into your A&P). If ED vitals very abnormal, can state this in PE. State results of studies/labs obtained above. Assessment/Plan: Assessment o Identify Problem #1, give leading diagnosis. Briefly state evidence supporting this. o State top 3-4 other leading diagnoses, with brief evidence against. Plan o Diagnostic studies (completed or to do) o Therapeutic plan Repeat for Problem #2, etc. Time Frame: around 9 minutes total HPI: 2 min ROS, PMH, Meds: 30-45 sec SHx, FamHx, etc.: 15-30 sec Physical Exam: 60-75 sec Labs/Studies: 30 sec Assessment/Plan: 2-3 min Practice, Practice, Practice! Present to your intern/senior resident before rounds, ask for feedback regularly, etc. Long/Short Call and Days Off Short call All teams admit every day until 5pm on the weekdays and 11am on the weekends. The team switching to nights on Sunday will not admit the Saturday before. Long Call The designated long call team will admit until 6 pm on Monday through Saturday and 4 pm on Sundays. No Doc days AMS covers ‘no doc’ Tuesday 7pm-Wed 7 pm and Thursday 7pm-Fri 7 pm. So typically you will have new patients to see on Wednesday and Friday mornings and can expect to get admission during the day on Wednesday and Friday. Night Float You will take in house call night float call with their team. The team is on nights every fifth week. When you are assigned to the night team, you will be working nights that week. Students are expected to participate in cross coverage duties with their assigned intern. The night team starts at 6 pm and leaves the hospital at 8 am Sunday through Friday. On Sunday, the night team starts at 4 pm and leaves at 8 am the following day. The patients that the night team admits will be distributed to the day teams in the morning. Patients admitted on the final night of the team’s night rotation will be kept by that team as the team switches to being a day team. The night team will round with their attending from 7-8am. Topics discussed will be determined by the residents and attending. The team may round (bedside) on one of the sicker patients, the team may want to talk about management issues etc. The attending may also chose to review H and Ps with respective team members. One of the day teams will be responsible for Saturday daytime admissions (11am-6pm) and another assigned to Sunday daytime admissions (11 am and 4 pm). Discuss the schedule specifics with your senior resident to see when your team is scheduled for nights, etc. Days Off MSIII: The team you work with will be dividing up days off to allow for continuity of patient care. They may suggest you take off a weekday, but according to U of A policy, “Medical students on the clerkship are not to take days off during the week. In general they will be given one of the weekend days off, but this will be coordinated with their attending.” One day off per week is the policy. If a 3 day holiday should fall on your rotation, you may NOT take those 3 days off, or you will be in violation of the school’s policy. MS IVs will have one day off a week. Days off will be arranged with the resident and approved by the attending at the beginning of the rotation. MSIVs Please notify Dolores and Dr. Novoa-Takara of your days off by the third or fourth day on the rotation. Weekend Days Once again, although your day off will likely be on a weekend, these are not automatically “off” It is highly preferred your day off be on a weekend. The reason for this being that your regular teaching attending is here Monday through Friday and a different attending will typically cover the weekend. If your team is on long call on a weekend day, expect to be in the hospital on that day. Absences There will be no planned absences during this rotation. Any absences should be reported to: 1) your school, 2)Dolores in medical education, and 3)your attending MS III Patient logs Keeping a log of the diagnoses you have seen during your training is an LCME requirement (accreditation for the medical school). You should be logging these, as well as your procedures, on E*Value. These account for 5% of your total grade. Any questions regarding patient logs or E*Value should be directed to Michelle Rios at the U of A. MS IV Evaluation Passports Should be filled out prior to the end of the rotations. See the additional section for subinterns. Feedback/Evaluations Ask for daily feedback from your team. At the 2-week mark, you need to arrange a face-to-face formal mid-month evaluation from your senior resident and attending. You cannot improve upon what you don’t know is a problem. MS III: Turn in one H&P per week to your attending for review, and SOAP notes as well, for feedback. You should get informal daily feedback from your intern/resident on these as well. MSIII: On each of your three sub-blocks in Internal Medicine, you will be required to complete one observed patient encounter (CEX- clinical competency exam) with your attending (a total of three for your entire medicine experience). Forms are on the website (www.goodsamim.com). Your final evaluation will be completed by one of your attendings. Often this will include information from other attendings with whom you worked as well as your resident. They should complete it in time for you to have formal verbal feedback in a timely manner, so plan ahead if necessary. Preparing for the Shelf Exam The book First Aid for the Internal Medicine Wards is a good one, too. There are copies if you do not wish to purchase it. See the department of medicine. MKSAP for Students: There are some copies available to borrow as another study resource. Attend the Exam Review with Dr. Gwisdalla as part of your core lecture series. If you have questions about the exam, see Dr. Gwisdalla. Students are expected to read about their patients on a daily basis. Students are encouraged to read from a textbook of medicine (Harrison’s, Cecil’s, etc) in addition to on line resources (e.g. UptoDate). Subspecialty textbooks are also a great reference. Your ID badge will get you into the library after normal business hours and on weekends. Students are also expected to read from medical journals. We tell our residents that they should be reading 108 minutes a day, you should be doing that too. Hospital Policies Students should dress neatly and be well groomed at all times. Please note the dress code. Sleeveless shirts, clam-diggers, and open-toed shoes are not appropriate. It is okay to ask your clerkship director if you are not sure about something. Students are required to wear name tags. Please try to refrain from waking patients up between 10 pm and 4 am. H and Ps will need to be done as well as cross cover assessments during this time. If your team has been called for a cross cover issue, you will need to wake the patient up. Use your judgement about the H and P—if you have forgotten something that is not vital and the patient is already alseep, you should probably wait until morning to address it with the patient. GME patient relationship policy A. Each resident/student is to introduce themselves by name and ensure that the patient and family know them by name. It is also important that resident/student explain their role in the care of each patient they attend. B. It is appropriate to address patients by their surname preceded by Mr, Ms., Dr., etc. Residents/students should address a patient by their first name only if invited to do so. Residents/students are encouraged to ask patients how they wish to be addressed. C. In the midst of the press of time and demands, it is important to remember that most patients are frightened, intolerant of their symptoms, frustrated, and often not coping as well as ordinary. Returning to this awareness increases one's tolerance of difficult situations and leads to genuinely rewarding relationships with patients and their families. Part of this is accurately identifying and acknowledging their feelings while avoiding judgment about these feelings. D. It is essential to take time to explain to patients what is happening to them, what is recommended for them, and the benefits and risks of your recommendations. E. Each resident/student is to dress neatly and be well groomed at all times. Students and residents are required to wear name tags/hospital ID badges. How to Excel on the Clerkship Care about your patients and take responsibility for them. Respect your peers. Don’t think that opportunists go unnoticed. Be a team player. Be timely- being consistently late for rounds, didactics, etc., is disruptive and construed as rudeness and disinterest. Perfect the basics-oral presentations, physical exam skills, and notes. Know your patients! You should be able to talk about them anytime, anywhere in the hospital without referring to the computer. You never know when you’ll run into one of your consultants… Take the time to prepare your thoughts before you present. Read, read, and read some more. Watch what the (stellar) intern does and try to emulate him/her. Work up your patients independently! Doing so with the “team” is insufficient to master this skill. You must return and spend additional time on the history and physical, as well as a comprehensive review of any previous medical records. Bring back and teach the knowledge you attain on your patients to the team. Ask your residents questions! They want you to ask questions and this shows that you are interested. Don’t appear to be trying to get out of work (Do I need to come back to the hospital, Do I need to see that patient now…), look for work (aka learning opportunities) Be sure to hang out with the team when you have down time. You will learn a lot of medicine even it if isn’t on your particular patient that you are following.