Childhood Apraxia of Speech - South Carolina Speech Language
advertisement

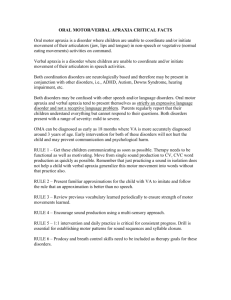
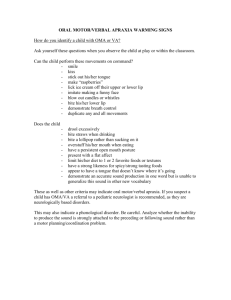
Catherine H. Earnhardt, MCD, CCC-SLP Financial: Catherine H. Earnhardt does not have any relevant financial information to disclose. Non-Financial: Catherine H. Earnhardt has a son with childhood apraxia of speech, she is the VP of Clinical and Professional Affairs on the SCSHA Executive Board, is the ASHA CE Administrator for SCSHA, and is the SCSHA convention co-chair. Definition and Terminology Characteristics of Childhood Apraxia of Speech Evaluation Challenges Differential Diagnosis Treatment Approaches Multi-Cultural Issues The Importance AAC with CAS Case Study “Childhood apraxia of speech (CAS) is a neurological childhood speech sound disorder in which the precision and consistency of movements underlying speech are impaired in the absence of neuromuscular deficits (e.g. abnormal reflexes, abnormal tone). CAS may occur as a result of known neurological impairments in association with complex neurobehavioral disorders of known and unknown origin, or as an idiopathic neurogenic speech sound disorder. The core impairment in planning and/or programming spatiotemporal parameters of movement sequences results in errors in speech sound production and prosody” (ASHA, 2007a, Definitions of CAS section, para. 1). Source: http://www.asha.org/Practice-Portal/Clinical-Topics/Childhood-Apraxia-of-Speech/ Childhood Apraxia of Speech (CAS) Dyspraxia Verbal Dyspraxia Developmental Apraxia of Speech Developmental Verbal Apraxia According to ASHA.org, the term Childhood Apraxia of Speech is preferred term. Source: http://www.asha.org/Practice-Portal/Clinical-Topics/Childhood-Apraxia-of-Speech/ The term “Developmental” is seen by many professionals and payor sources as a “delay” in development. Prefix “A” implies Absence and the Prefix “Dys” implies Partial. This is usually used as a personal preference, based on a geographic area, or based on the educational institution. The term “Apraxia” is widely used to describe the adult form of Apraxia. ASHA.org states that the term Childhood Apraxia of Speech is used as a “unifying cover term for all presentations of apraxia of speech in childhood, whether congenital or acquired or associated with a specific etiology”. Source: http://www.asha.org/Practice-Portal/Clinical-Topics/Childhood-Apraxia-of-Speech/ Source: http://www.apraxia-kids.org/guides/slp-start-guide/the=terminology/ Suspected Childhood Apraxia of Speech: It is considered best practice to diagnose any child under the age of 3 with Suspected Childhood Apraxia of Speech Vs. Childhood Apraxia of Speech. Once the child turns three years of age a reevaluation is completed and the diagnosis of Childhood Apraxia of Speech can be given at that time. Automatic Speech vs. Volitional Speech Automatic Speech: Speech activities that have become rote and does not require motor planning (i.e. 1-10, DOW, MOY). Volitional Speech: Involves motor planning and sequencing of sound segments for correct articulator movement and speech production 1-2 children per 1,000 3.4% to 4.3% of all children referred for evaluation of speech disorder Boy to girl Ratio: 2 or 3:1 (more boys than girls) Increase Prevalence Rate with certain comorbidities (i.e. galactosemia and fragile x syndrome). Source: http://www.asha.org/Practice-Portal/Clinical-Topics/Childhood-Apraxia-of-Speech/ ASHA’s Ad Hoc Committee on Childhood Apraxia of Speech Cites and Increase prevalence in CAS cases with Complex Neurobehavioral Disorders to include: Autism Epilepsy Fragile X Syndrome Galactosemia Rett Syndrome Chromosome Translocations Involving Deletions and Duplications In most cases there is no known cause Considered to be a Neurological Deficit Higher prevalence with certain Genetic Disorders/Syndromes Damage to areas of the brain controlling motor planning (i.e. Brain Injury/Stroke) Not every child with CAS present the same Inconsistent errors are a key characteristic Not all characteristics are present. This a major reason why not every child with CAS will present the same. It is not a disorder that can be “out grown” and there is no cure (This is a major reason why we must be careful with diagnosing a child as having CAS). Typically once something is learned, it is difficult to correct if it is incorrect (example: daycare calling a child “Hunter E” if there are two Hunters and the child starting to say their name as “Hunter E”. It can be very difficult to reteach a child with CAS to say “Hunter”. There is frustration because the child understands what is going on around them but they can’t express their wants and needs. “There is something wrong with my mouth.” “Everything I say is wrong.” “Why won’t my mouth work?” “Why don’t you understand me?” “There is something wrong with me.” A person’s perception is their reality. Imagine if this was your reality. Motor Planning Disorder Difficulty with sequencing sound segments Not related to muscle weakness or paralysis Inconsistency with errors Provided that there is not a cognitive deficit present, the child knows what they want to say but the muscles will not move in the correct sequence to make the correct sounds. Source: http://www.asha.org/public/speech/disorders/childhoodApraxia Inconsistent errors with Sound Segments Inappropriate Prosody Groping High incidence of vowel distortions Frequent sound distortions and distorted consonant substitutions Initial Consonant Deletion Voicing Errors Schwa additions/insertions to consonant clusters Greater ease with use of frequently used phrases that become much like automatic speech phrases: “I love you” Difficulty with accurate movement of speech musculature when trying to imitate words not previously mastered Inconsistent suprasegmental characteristics (rate, pitch, loudness) Increased errors with increased MLU and longer/more complex syllables and words. Atypical Regression Sequencing Errors Source: http://www.asha.org/Practice-Portal/Clinical-Topics/Childhood-Apraxia-of-Speech/ Limited vowel repertoire; less differentiation between vowel distoritions Idiosyncratic error patterns (Many times these errors are impossible to transcribe) Errors increase with MLU and complexity of words and sound segments Prosody disturbances including overall slow rate The child may be able to say the target sound correct in one utterance but will produce the same target sound incorrectly in another utterance. Impaired diodochokinetic tasks (unable to maintain consistent rate of sequences such as /pa/ /pa/ /pa/ and/or accuracy with sequencing such as /pa/ /ta/ /ka/ “Choppy” monotone speech Groping or observable physical struggle with muscle movement to produce a target sound Impairment with non-speech movements may be present if the child also has oral apraxia Source: www.apraxia-kids.org/guides/slp-start-guide/key-charactoristics-of-cas/ http://www.google.com/url?sa=i&rct=j&q=&esrc=s&source=images&cd=&cad=rja&uact=8&ved=0CAYQjB1qFQoTCMCn0rf8i8kCFYlZJgodmD YPCQ&url=http%3A%2F%2Fwww.thedcladies.com%2F2014%2F07%2F15%2Fwhat-is-childhood-apraxia-ofspeech%2F&psig=AFQjCNEZj1ZONTZVORBhpOgFnWbABrDKiw&ust=1447455058756580 ASHA Position Statement Childhood Apraxia of Speech Ad Hoc Committee on Childhood Apraxia of Speech http://www.asha.org/policy/PS2007-00277/ “Review of the research literature indicates that, at present, there is no validated list of diagnostic features of CAS that differentiates this symptom complex from other types of childhood speech sound disorders, including those primarily due to phonological-level delay or neuromuscular disorder (dysarthria).” Source: http://www.asha.org/policy?PS2007-00277/ “Three segmental and suprasegmental features that are consistent with a deficit in the planning and programming of movements for speech have gained some consensus among investigators in apraxia of speech in children: (a) Inconsistent errors on consonants and vowels in repeated productions of syllables or words. (b) Lengthened and disrupted coarticulatory transitions between sounds and syllables (c) Inappropriate prosody, especially in the realization of lexical or phrasal stress.” Source: http://www.asha.org/policy?PS2007-00277/ Inconsistencies with voice, prosody, rate, articulation, and errors. Cat Target Production 1: mat Target Production 2: bet Target Production 2: moj Etc. Groping and uncoordinated muscle movements can be misdiagnosed as a stutter CAS is a motor speech disorder that effects the ability to sequence sound segments at the word, phrase, and sentence level. Therefore, the child has difficulty learning to put the sounds together to say the word. The typical child acquires speech sounds in the initial, final and then middle position of the words. The child with CAS must learn each word. Typical Prosody: Intonation rises at the beginning of the phrase or utterance and then falls at the end of the phrase or utterance. This rising and falling of intonation are markers that identify the phrase or utterance boundaries. Prosody with CAS: Trouble with natural inflection and natural stress to mark phrase and utterance boundaries. There is often also inconsistency with prolonged pauses making a smooth transition difficult. “Importantly, these three features are not proposed to be the necessary and sufficient signs of CAS. These and other reported signs change in their relative frequencies of occurrence with task complexity, severity of involvement, and age.” Source: http://www.asha.org/policy?PS2007-00277/ ASHA.org Childhood Apraxia of Speech http://www.asha.org/public/speech/disorders/ ChildhoodApraxia/ Delayed Language Development Difficulty with fine motor movements/coordination (writing, buttoning clothes, etc.) Difficulty with sequencing other motor movements (riding a bike, karate, swimming, etc) Word order difficulty Hypersensitivity and/or Hyposensitivity in their mouths (may not like certain textures in the mouth – toothbrush, mixed consistencies, crunchy consistencies, etc) Difficulty learning to spell, read and write Source: www.asha.org/public/speech/disorders/ChildhoodApraxia/ Children with CAS present differently Not all characteristics of CAS are present No validated list of characteristics for differential diagnosis at this time. Limited Speech Samples Must rule out: Auditory deficits Severe Phonological Disorder In some cases you may need to rule out velopharyngeal Insufficiency (VPI) 1. 2. 3. 4. 5. 6. ASHA’s Practice Portal Cites that there are a variety of reasons that it is difficult to diagnose CAS under the age of 3: “the potential presence of developmental disabilities and/or comorbid conditions” “The lack of a single validated list of diagnostic features that differentiates CAS from other types of childhood speech sound disorders (e.g., those due to phonological-level deficits or neuromuscular disorders)” The fact that some primary characteristics of CAS (e.g., word inconsistency, a predominant error pattern of omission, etc.) are characteristics of emerging speech in typically developing children under the age of 3 years” “The lack of a sufficient speech sample size for making a more definite diagnosis” “The challenge of sorting out inability versus unwillingness to provide a speech sample or to attempt a speech target” “The possibility that changes occurring prior to age 3 (e.g., developmental maturation, social and linguistic peer exposure, and beneficial effects of therapy) may alter the diagnostic label” Source: http://www.asha.org/PRPSpecificTopic.aspx?folderid=8589935338&section=Assessment/ ASHA’s Practice Portal Cites: “Diagnosis below age 3 is best categorized under a provisional diagnostic classification, such as “CAS cannot be ruled out,” “Signs are consistent with problems in planning the movement required for speech,” or “suspected to have CAS.” Source: http://www.asha.org/PRPSpecificTopic.aspx?folderid=8589935338&section=Assessment/ Case History Hearing Screening Oral-Motor Evaluation Articulation/Speech Production Prosody Voice Language ASHA Practice Portal Also Cites the Use of Additional Tasks for Differential Diagnosis to Include: “nonspeech articulatory postures (e.g., smile) and sequencing (e.g., kiss-smile) versus speech sounds and words” “Well practice/automatic versus volitional speech (for children who are older and/or have some speech)” “Speaking tasks that require single postures versus sequences of postures (e.g., single sounds such as /a/ vs. words such as /mama/” “Speech production at the syllable, single-word, bisyllable, multisyllable, phrase and sentence levels” “sequential/alternating movement repetitions (e.g., /papapapa/ versus /pataka/, formerly called diadochokinesis)” 1. 2. 3. 4. 5. 6. 7. 8. Limited early sound play Sound inventory restrictions Expressive language deficits in contrast to receptive language Imitation superior to Volitional Skills Sequencing/Movement difficulties Word/Sentence complexity breakdown Prosodic deviances Inconsistencies Source: Hammer, David, M.A., CCC-SLP Childhood Apraxia of Speech: New Perspectives on Assessment and Treatment: Spnonsored by CASANA; 2008 9. Voiced/Voiceless sound errors 10. “Groping” behaviors 11. Vowel Distortions 12. Sound Omissions Source: Hammer, David, M.A., CCC-SLP Childhood Apraxia of Speech: New Perspectives on Assessment and Treatment: Spnonsored by CASANA; 2008 Multi-sensory Input Approach: Input that is visual, proprioceptive, tactile and auditory to teach sequencing of motor movements for speech production (CASANA) Motor Programming Approaches: sequencing of articulator movements for speech production (asha.org/policy) Combined Linguistic-Motor Programming Approaches: uses tactile cues along with descriptive phrases/cues for sound production (asha.org/policy) Sensory and Gestural Cueing Approaches: Electropalatography of tongue movement to provide visual feedback (asha.org/policy) Integral Stimulation Approach (modified for the use with children as Dynamic Temporal and Tactile Cueing): Most commonly used method in treating speech disorders; involves the child imitating target utterances produced by the clinician “listen to me, watch me, do what I do” (CASANA) Prosodic Cueing Approach: Incorporates rhythm, stress and melody to produce speech production; example: Melodic Intonation Therapy (MIT); usually used with less severe deficits or later in therapy (CASANA) CASANA “Treatment Approaches for Children with Childhood Apraxia of Speech (CAS)” http://www.apraxia-kids.org/apraxiainformation-downloads/ Developed by Nancy R. Kaufman, who is the owner of Kaufman Children's Center for Speech, Language, Sensory-Motor, and Social Connections, Inc. Breaks the target into smaller units and builds back up to the larger speech target using cues, fading cues and cueing before failure. (ASHA – Portal) Video 3 Year Old Male with CAS https://www.youtube.com/watch?v=pCw3Jn7NW_s Build on current expression Use starter positions Label sounds, but try to incorporate placement/manner cues Make a core vocabulary book Benefits: Organizes a starting vocabulary for facilitation of a mutal focus between therapist, parents, other caregivers and communication partners in the child’s life Enables the child a sense of success Allows parents/caregivers to immediately feel a part of the “team” Provides a foundation for AAC device if necessary. Also allows for low tech AAC vocabulary and expanding on current core vocabulary Procedures: Use photographs containing pictures of people, toys, objects, and verbs important in the child's life, as well as target words for therapy. Photographs placed in a “Grandma’s Brag Book” with written words at the top (when you point at the picture do not cover the word). Prompts for Restructuring Oral Muscular Phonetic Targets Providing tactile-kinesthetic-proprioceptive input for speech production Apraxia motor planning/sequencing deficits secondary to decrease independent articulator movement. Therefore, patient can learn sequence for one word instead of for specific sound to be carried over to other words. Must gain independent movement between lingual, labial and jaw movements Independent movement of labial and lingual movement is not possible without jaw stability Appropriate Referrals May Include: Audiological/ENT Evaluation VPI Evaluation Physical Therapy: gross motor skills are a concern Occupational Therapy: fine motor skills are a concern Speech Language Pathology Referral: Skilled and experienced Clinicians in motor speech disorders should assess CAS cases or be under the supervision of a Speech Language Pathologist with specific training/experience in motor speech disorders (ASHA Ad Hoc Committee on Childhood Apraxia of Speech). Key to allowing a child with CAS a successful means of communication. Can be low tech or high tech based on the child’s abilities and needs Key to expanding the core vocabulary Key to expanding expression Reduces aggressive behavior and frustration due to inability to express thoughts, ideas, wants and needs Increases progress towards verbal expression Lay down foundation for language (pre-linguistic skills not mastered due to limited early sound play) Bilingual/Multilingual Populations Factors to Consider Per ASHA’s Practice Portal: “Bilingual treatment may facilitate greater improvement than English-only treatment in a child with CAS” “Beginning treatment by first targeting phonemes that are shared between the languages spoken by a child may yield the greatest improvement in intelligibility across languages in the shortest amount of time.” “Cross-linguistic transfer is also most successful when stimuli are chosen that are shared between the two languages. Additionally, cross-linguistic transfer can be used to target goals in one language while targeting properties of a second language. For example, treatment addressing multisyllabic words in Spanish may facilitate transfer to the phrase level in English.” Source: http://www.asha.org/PRPSpecific Topic.aspx?folderid=8589935338&section=Treatment Bilingual/Multilingual Populations Factors to Consider Per ASHA’s Practice Portal: “Errors that are only present in one language are unlikely to improve intelligibility in the other language when addressed in treatment. For example, if final consonants are targeted in English to improve intelligibility, but occur rarely in the child’s primary language, intelligibility in that language will not be positively influenced by addressing accurate final consonant productions in English.” “Clinicians consider the context in which a child uses each language identify vocabulary words that are likely to facilitate carryover, functional use, and repeated practice and exposure in each language.” “Treatment incorporates activities that facilitate cross-linguistic transfer of skills and improved intelligibility, including providing activities for home practice in the language used by the family.” “Goals and Targets in each language are chosen based on the properties and word shapes of each language. English has more monosyllabic words with consonant clusters and, thus, targets in English should be representative of the word shape.” Source: http://www.asha.org/PRPSpecific Topic.aspx?folderid=8589935338&section=Treatment 1:9 Male History of: oral, pharyngeal dysphagia with multiple hospitalizations for aspiration pneumonia. In speech therapy since 4 weeks of age but was moved to another speech therapist at 8 weeks of age because the mother felt the treatment was increasing risk of aspiration. malignant hypothermia visual field delay – resolved, Severe torticollis (neck angled to one side) resulting in torso weakness, right-sided weakness. Torticollis was resolved but was followed by hypersensitivity to the right side. Initial ENT diagnosis of conductive hearing loss. However, upon inspection of the tympanogram the mother determined that the results were not consistent with a conductive hearing loss and sought a second opinion that concurred with the mothers findings of a sensorineural hearing loss. ENT diagnosis of Laryngeal collapse and mild bilateral sensorineural hearing loss for all frequencies. Tubes were placed at 14 months – hearing loss resolved. Patient did not begin walking until 13 months due to torticollis Not yet toilet training at 1:9 Reported periods of gain followed by loss of acquired skill. Diagnosed by Occupational therapy as having hand and finger apraxia Physical therapy since 4 weeks of age and occupational therapy since 6 months of age. Recently discharged from physical therapy but continued with occupational therapy No babbling or playing with speech sounds Has a good /m/ and says /mama/ for all purposes Vowel distortions Inconsistent errors Use of simple signs (i.e. more, etc) Able to nod for yes/no Will use intonation with grunts Jaw pumping and “groping” with verbalization attempts, especially when attempting to initiate. Can follow 4-5 step directions and was tested as being cognitively 2 years above his chronological age Extreme frustrations with attempts to verbalize to the point that the pediatrician wanted to label the child autistic. The mother disagreed with this diagnosis, refused the referral for autism testing and sought another pediatrician. Continues to have significant drooling at 1:9 Interacts only with younger children that are nonverbal Likes playing with ‘Thomas the Train’ and things with faces. Severe separation anxiety if mother or grandmother is not present. 1. 2. 3. What are your impressions about the child based on the information provided by the parent? What are your impressions about the parent based on the information provided by the parent? What are your impressions related to differential diagnosis? “There is something wrong with my mouth.” “Everything I say is wrong.” “Why won’t my mouth work?” “Why don’t you understand me?” “There is something wrong with me.” A person’s perception is their reality. Imagine if this was your reality. “Why can’t I fix this for my child? I failed him.” 1. 2. 3. 4. 5. 6. 7. Kaufman Speech Praxis Test for Children (KPST) was given. Clinical Impressions and Diagnosis: Key characteristics for CAS noted: “Limited repertoire of vowels; less differentiation between vowel productions; and vowel errors, especially distortions” “variability of errors” “Unusual, idiosyncratic error patterns” “able to produce accurately the target utterance in one context but is unable to produce the same target accurately in a different context” More difficulty with volitional, self-initiated uttereances as compared to over-learned, automatic, or modeled utterances” At some point in time, groping or observable physical struggle for articulatory position” Impaired volitional nonspeech movements” 1. 2. 3. 4. The following Characteristics were noted that may describe children with CAS “Delayed onset of speech” “Limited babbling as an infant” “Restricted sound inventory” “Loss of apparently previously spoken words” 1. 2. Recommendations It is recommended that Hunter be enrolled in a treatment program with goals consistent with those addressed in treatment with CAS, including a primary focus of increasing functional communication through signs and gestures while building on sounds in his phonemic repertoire to increase verbal output. It is recommended that, if at all possible, Hunter’s treatment be administered in short, frequent sessions (20-30 minutes sessions 2-3 times per week). KPST results indicated a Severe speech praxis disorder. Due to his age, the mother asked, and the evaluating therapist agreed to place Hunter under a “Working Diagnosis of Childhood Apraxia of Speech”. One year later, he was re-tested with the KPST, by the same evaluating therapist, and was diagnosed as having Severe Childhood Apraxia of Speech. Hunter’s hand apraxia had improved with occupational therapy and hunter was starting on a low tech picture AAC with a core vocabulary. Between 2:9 and 3:9, he saw significant increase with expressive language due to: 1. 2. 3. Implementation of key components of the Kaufman and Hammer treatment modalities. AAC use for successful communication in restaurants, home, etc to increase independence and ability to express specific wants/needs. Although the severity of his CAS should have resulted in the use of ACC in the 4K, he entered 4k with the ability to successfully communicate expressively in 60% of attempts. No AAC was necessary in the school setting. He saw significant rates of progression with verbal expression and accuracy with the addition of PROMPT therapy modalities, although Kaufman and Hammer continued to be used as well. He also so significant increase in overall motor planning with activities that utilized proprioceptive input with gross motor movements. Swimming Riding Bike Soccer “Position Statement: Childhood Apraxia of Speech: Ad Hoc Committee on Childhood Apraxia of Speech”, ASHA 2007: http://www.asha.org/policy/PS2007-00277/ “Childhood Apraxia of Speech” ASHA http://www.asha.org/public/speech/disorders/ChildhoodApra xia/ “If I Could Only Tell You, I would Say …” CASANA http://www.apraxia-kids.org/apraxia-information-downloads/ “Treatment Approaches of Children with Childhood Apraxia of Speech (CAS): Fact Sheet”, CASANA http://www.apraxiakids.org/apraxia-information-downloads/ “About Childhood Apraxia of Speech” CASANA, http://www.apraxia-kids.org/apraxia-information-downloads/ Please Note: The presenter will not be providing printed copies of the session resources to ensure that there is no perception of copyright infringement. The presenter requests that you print a copy for your individual use. CASANA Video Hope Speaks: An Introduction to Childhood Apraxia of Speech https://secure2.convio.net/caosa/site/Ecommerce/1590065402?VIEW_PRODUCT=true&product_id=1121 &store_id=1241/ CASANA Video Treatment Strategies For Childhood Apraxia of Speech with David W. Hammer, M.A., CCC-SLP https://secure2.convio.net/caosa/site/Ecommerce/1590065402?VIEW_PRODUCT=true&product_id=1141 &store_id=1241/ “Technical Report: Childhood Apraxia of Speech: Ad Hoc Committee on Apraxia of Speech in Children”, ASHA 2007: http://www.asha.org/policy/TR2007-00278/ “Childhood Apraxia of Speech”, ASHA Practice Portal: http://www.asha.org/Practice-Portal/ClinicalTopics/Childhood-Apraxia-of-Speech/ “Speech-Language Pathologist Start Guide” CASANA: http://www.apraxia-kids.org/guides/slp-statrt-guide/ “PROMPS for Restructuring Oral Musculature Phonetic Targets” Introduction to Technique: Manual, The PROMPT Institute; Revised January 2012. “Childhood Apraxia of Speech: Resource Guide” Dr. Shelley L. Velleman