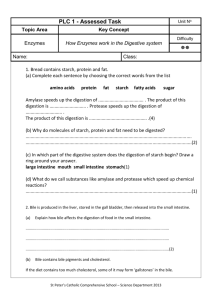
GI Anatomy And Physi..
advertisement

GI Anatomy and Physiology Presented by Derrick Anderson S 1 2 Definitions: Digestive Process S Ingestion Taking food in S Propulsion moving food through alimentary canal S S Peristalsis Mechanical digestion S Chewing, churning by the stomach, segmentation S Chemical digestion: Breaking down molecules S Absorption: Taking in molecules S Defecation eliminating indigestible substances 3 Where does the GI system start??? Mouth 4 Gastrointestinal Tract 5 Peritoneum S The serous membrane of the abdominopelvic cavity S Peritonitis inflammation of the peritoneum S Two Parts S Visceral Peritoneum S Covers external surface of most digestive organs S Continuous with the parietal peritoneum S Parietal Peritoneum S Lines the body wall S Continuous with the visceral peritoneum 6 Peritoneal Cavity S Potential space containing slippery fluid secreted by the serous membranes S Filled with serous fluid lubrication S Following diagram depicts the “potential space” of the peritoneal cavity 7 8 Mesentery S Double layer of peritoneum extending to the digestive organs from the body wall S Provide routes for blood vessels, lymphatics and nerves to reach digestive viscera S Hold organs in place S Stores fat S Can be dorsal or ventral 9 10 Continuous Pathway S Alimentary canal – continuous, muscular canal S aka gastrointestinal S Mouth, pharynx, esophagus, stomach, small intestine, large intestine S Accessory digestive organs S Teeth, tongue, gallbladder, salivary glands, liver and pancreas 11 Histology of the Alimentary Canal* S Four basic layers (“tunics”) from the esophagus to the anal canal S Mucosa S Submucosa S Muscularis externa S Serosa * All layers are presented starting from the innermost layer 12 Alimentary Canal 13 Mucosa S Aka mucus membrane S Innermost layer S Epithelial membrane S Lines the lumen of the alimentary canal 14 Functions of the Mucosa S Secrete mucus, digestive enzymes and hormones S Absorb end products of digestion into the blood S Protect against infections S Depending on the region of the mucosa one or all of these functions may be occur 15 Mucosa Sublayers S Epithelieum S Lamina propria S Muscularis mucosae 16 Mucosal Epithelium S Simple columnar epithelium S Contains mucus-secreting cells S Protects the GI tract from the digestive enzymes S Eases passage of substances 17 Lamina Propria S Loose areolar connective tissue S Capillaries nourish epithelium and absorb nutrients S Contains lymphoid follicles S MALT mucosa-associated lymphatic tissue S Defend against pathogens 18 Muscularis Mucosa S Smooth muscle cells S Local movements of the mucosa S Exist as many folds in the small intestine 19 Alimentary Canal 20 Submucosa S Areolar connective tissue S Rich supply of blood and lymphatic vessels, lymphoid follicles and nerve fibers S Contains elastic fibers S Allows stomach to return to normal shape after being stretched from storing food S Extensive vascular network supplies surrounding tissue 21 Alimentary Canal 22 Muscularis Externa S Aka muscularis S Responsible for peristalsis and segmentation S Inner circular layer of smooth muscle S Thickens in some areas to form sphincters which prevent backflow S Contraction = smaller lumen S Outer longitudinal layer of smooth muscle S Contraction = shorter tube 23 Alimentary Canal 24 Serosa S Protective outermost layer S Same as Visceral peritoneum S Areolar connective tissue covered with mesothelium S Mesothelium = single layer of squamous epithelial cells S Replaced by adventitia in the esophagus S Fibrous connective tissue binding the esophagus to the surrounding structures 25 Alimentary Canal 26 Enteric Nervous System S Nerve supply for the GI S Regulate digestive system activity S Semiautonomous S 2 major intrinsic nerve plexuses S Submucosal S Myenteric S Also subject to control by the CNS and ANS 27 Submucosal Nerve Plexus S In the submucosa S Sensory and motor neurons S Regulates activity of glands and smooth muscle in the mucosa 28 Myenteric Nerve Plexus S Between the circular and longitudinal smooth muscle of the muscularis S Provide major nerve supply to GI tract wall and control GI motility 29 Mouth and Associated Organs 30 Mouth S Lined with stratified squamous epithelium S Withstand friction S Epithelium of the gums, hard palate and dorsal tongue are slightly keratinized S Contains antimicrobial peptides called defensins 31 Salivary glands S Paired tubuloalveolar glands S Saliva S Cleanses mouth S Dissolves food chemicals so that they can be tasted S Moistens food and aids in forming a bolus S Contains enzymes that begin chemical breakdown of starchy food 32 Salivary Glands S Parotid gland S Largest S Anterior to ear S Mumps S Submandibular gland S Sublingual gland 33 Salivary Glands S 2 types of secretory cells S Serous S Produce watery secretion containing enzymes ions and mucin S Parotid gland only has these S Mucus S Produce mucus S Sublingual contains mostly these S Submandibular contains equal amounts of both cell types 34 Esophagus S Joins stomach at cardiac orifice S Cardiac orifice surrounded by gastroesophageal or cardiac sphincter S Physiological sphincter slight thickening S Not a true sphincter emesis; heartburn 35 Esophagus S Nonkeratinized stratified squamous mucosa S Changes to simple columnar epithelium at the esophagus-stomach junction S Specialized for secretion S Submucosa contains mucus-secreting esophageal glands S “greases” the lumen of the esophagus to ease passage of the bolus S Muscularis externa (Muscle type transition) S Upper (skeletal)Middle(skeletal and smooth)Lower (smooth) muscle S Adventitia (serosa layer) S Fiborus Connective tissue 36 Stomach Tissue 37 Digestive Process: Mouth to Stomach S Mastication = chewing S Mechanical breakdown S Voluntary and reflexive S Deglutination = swallowing S 2 phases S S Buccal phase S In the mouth; voluntary S Tongue forces bolus down Pharyngeal-esophageal phase S Triggered by bolus reaching receptors in the pharynx S Involuntary; controlled by swallowing center located in the brain stem S Respiration temporarily inhibited 38 39 Stomach S Upper left quadrant of the peritoneal cavity S “Storage tank” S Size S Empty = 50 ml S Can expand to a volume of 4 L (about 1 gallon) S Chemical breakdown of proteins begins S Food converted to creamy paste called chyme 40 Stomach 41 Stomach S Contains folds called rugae S Regions S Cardiac region (near the heart) or cardia S Surrounds cardiac orifice S Fundus Body S Pyloric region S Pyloric antrum wider and more superior S Pyloric canal narrower S Pylorus S Pyloric sphincter a true sphincter S Controls stomach emptying 42 Stomach 43 Stomach 44 S Omenta mesenteries extending from the greater and lesser curvatures S Tether stomach to abdominal wall S Lesser omentum S Greater omentum extends down to cover the small intestine S Contains a lot of fatty tissue and lymph nodes S Arterial supply comes form celiac trunk S Subject to para control 45 Abdominal Omentum 46 Microscopic Anatomy S Modified muscularis and mucosa S Muscularis has an additional innermost layer of smooth muscle fibers running obliquely S Allows stomach to mix, churn move and pummel food S Mucosa is simple columnar epithelium comprised entirely of mucus cells S Mucus cells produce protective two-layer coat of alkaline 47 Stomach Mucosa S Deep gastric pits S Mucous cells form the walls of the gastric pits S Pits lead into gastric glands produce gastric juice S Mucus neck cells upper region of gastric glands S Produce thin soluble mucus different from mucus from the mucus cells 48 Parietal And Chief Cells 49 S Parietal Cells middle region of glands S Secrete hydrochloric acid (HCl) and intrinsic factor S Have microvilli increased surface are for more HCl secretion S HCl creates extremely acidic environment of the stomach which is required for optimal activity of pepsin (enzyme) S Intrinsic factor is a glycoprotein required for vitamin B12 absorption in the small intestine 50 S Chief Cells mostly basal region of gastric glands S Produce pepsinogen (inactive form of pepsin) S Pepsin digests protein S At first, pepsinogen is converted to pepsin due to presence of HCl S However, once pepsin is present, pepsin itself catalyzes activation of pepsinogen S Positive feedback S Also release lipase 51 Parietal and Chief Cells 52 S Enteroendocrine cells deep in gastric glands S Release variety of chemical messengers directly into the lamina propria S Histamine, serotonin, somatastatin and gastrin 53 Vulnerable Stomach? S No! S Mucosal Barrier S Thick coating of bicarbonate rich mucus on stomach wall S Tight junctions between epithelial cells prevent leaking of gastric juices into underlying tissue S Damaged epithelial cells are shed quickly and quickly replaced by undifferentiated stem cells S Stomach mucus cells renewed every 3-6 days 54 H. pylori and Gastric Ulcers S Acid resistant bacteria that burrow through mucus and destroy protective mucosal layer S Release… S ammonia to neutralize the environment S Cytotoxin that damages stomach epithelium S Detected by a breath test S Treated with 2 week long antibiotic course 55 Gastric ulcers S For ulcers not caused by H. pylori usually caused by long-term use of NSAIDs (eg. Aspirin, ibuprofen) S Treated with H2 (histamine) receptor blockers S Cimetidine (Tagamet) S Ranitidine (Zantac) 56 Digestive Process in the Stomach S Protein digestion is the primary digestion that occurs in the stomach S HCl S Pepsin S In infants, stomach also secretes enzyme called rennin S Acts on milk protein casein 57 Alcohol and Aspirin S Lipid soluble substance S Absorbed directly from the stomach into the blood 58 Intrinsic Factor S Secreted by parietal cells S Required for intestinal absorption of vitamin B12 S B12 important for production of mature erythrocytes S Deficiency can cause anemia 59 Regulation of Gastric Secretions 60 S Both neural and hormonal control S Neural control S Long nerve reflexes (vagus nerve) S Vagus nerve stimulation = increased activity of nearly all glands S Sympathetic nerve stimulation = opposite S Short nerve reflexes (local enteric) S Hormonal control is mostly mediated with gastrin (stomach) and hormones from the small intestine S Stimulates secretion of enzymes and HCl 61 Phases of gastric secretion S Cephalic phase S Gastric phase S Intestinal phase 62 Cephalic phase S Occurs before food enters the stomach S Few minutes long S Stimulated by smell, taste, sight or thought of food and gets stomach ready 63 Cephalic Phase- Extrinsic S Activated olfactory receptors and taste buds send signals to the hypothalamus S Hypothalamus stimulates vagal nuclei of the medulla oblongata S Vagus nerves transmits motor impulses to parasympathetic enteric ganglia S Enteric ganglionic neurons stimulate the stomach glands 64 65 Gastric Phase S Occurs once food enters stomach S 3-4 hours S Provides 2/3rd of gastric juices released S Most important stimuli: S Distension activates stretch receptors and local (myenteric) and long (vagovagal) reflexes S Both reflexes cause acetylcholine (ACh) to be released which stimulates gastric juice secretion S Peptides S Low acidity 66 Gastrin S Chemicals from partially digested proteins, caffeine, and rising pH directly activate enterendocrine cells called G cells S G cells release gastrin S Gastrin stimulates HCl secretion S Highly acidic environment inhibits gastrin secretion S G cells also stimulated by neural reflexes S G cells inhibited by sympathetic nervous system 67 HCl and Parietal Cells S HCl secretion stimulated by 3 chemicals all of which work via 2nd messengers S ACh from parasympathetic fibers increase intracellular Ca2+ levels S Gastrin from G cells increase intracellular Ca2+ levels S Histamine from enterochromaffin-like cells acts through cAMP S When all 3 chemicals bind to parietal cells much HCl secretion S When only one binds not much HCl 68 HCl formation S H+ actively pumped into stomach lumen by H+ K+ ATPase for exchange of K+ ions into the cell S Cl- ions follow H+ ions into the lumen in order to maintain an electrical balance S Cl- comes from blood plasma S H+ comes from carbonic acid within the parietal cells 69 S As H+ is pumped into the stomach, bicarbonate ion (HCO3-) accumulates in cell and moves into the blood S HCO3- moves into blood via the HCO3- Cl- antiporter S As HCO3- moves into blood, Cl- moves in opposite direction into cell 70 Stomach-Blood vessel Interaction 71 72 Intestinal Phase S Has an excitatory and inhibitory component S Excitatory component S As food enters the duodenum intestinal mucosal cells are stimulated to release intestinal (enteric) gastrin, a hormone that encourages gastric glands to continue activity S As intestine distends, inhibitory component takes over because intestines can’t handle harsh acidic chyme 73 Enterogastric Reflex S Begins the inhibitory component of the intestinal phase S Inhibits vagal nuclei in medulla S Inhibits local reflexes S Activates sympathetic fibers to cause pyloric sphincter to tighten and prevent more food entering the small intestine 74 S Causes release of intestinal hormones called enterogastrones S Secretin S Cholescystokinin (CCK) S Vasoactive intestinal peptide (VIP) S All inhibit gastric secretion when stomach is very active 75 76 77 78 Small Intestine S Convoluted tube extending from pyloric sphincter to ileocecal valve where it joins the large intestine S Longest part of the alimentary canal S 3 subdivisions: duodenum, jejunum, ileum 79 Duodenum S Shortest S Bile duct and pancreatic duct unit at wall of the duodenum hepatopancreatic ampulla S Hepatopancreatic sphincter controls entry of bile and pancreatic juices 80 Liver 81 Jejunum and Ileum S Jejunum is in between duodenum and ileum S Ileum is longest S Ileum joins long intestine at the ileocecal valve S Jejunum and ileum are suspended by mesentery 82 Nerve Supply S Parasympathetic from the vagus nerve S Sympathetic from the thoracic splanchnic nerves S Both relayed through the superior mesenteric plexus 83 Arterial Supply S Mostly from the superior mesenteric artery S Veins parallel the arteries and drain into the superior mesenteric vein S Superior mesenteric vein then drains into the hepatic portal vein which carries nutrient-rich blood to the liver 84 Structural Modifications of the Small Intestine S Circular folds S Villi S Microvilli S All increase surface area 85 Circular Folds S Aka plicae circulares S Deep permanent folds of the mucosa and submucosa S Slow chyme movement to allow time for full nutrient absorption 86 Small Intestine 87 Villi S Fingerlike projections of the mucosa S Epithelial cells of villi are mostly columnar cells for absorption S Lacteal lymph capillary + dense capillary bed at the core of each villus S Nutrients are absorbed into the blood and the lymph 88 89 Microvilli S Densely packed S “brush border” of mucosa S Contain brush border enzymes which complete digestion of carbohydrates and proteins 90 91 Histology S Mucosa is mostly made up of simple columnar cells for absorption S Epithelium also contain mucus-secreting goblet cells S Pits between villi that lead into tubular glands called intestinal crypts 92 Intestinal Crypts S Secrete intestinal juices (watery with mucus) S Carrier fluid for nutrients S Enteroendocrine cells scattered through crypts S Source of enterogastrones (secretin and CCK) S Intraepithelial lymphocytes Type of T-cell S Immediately kill infected cells S S Paneth Cells S Secretory cells that release defensins and and lysozyme (antimicrobial enzyme) S Secretions kill some bacteria and keep others 93 94 Intestinal Submucosa S Contains typical areolar connective tissue and er peyer’s patches S Peyer’s patches S Aggregated lymphoid follicles S Increase in number along the length of the small intestine (more in the ileum) S Duodenal glands S Mucus secreting S Only in submucosa of duodenum S Produce alkaline mucus to neutralize acidic chyme 95 Peyer’s patch component of Gut Associated lymphoid tissue (GALT) Follicles lined by specialized M cells, short microfolds (the name M Cell) Lymphoid follicles with germinal centers Domed areas lacking villi Basolateral pockets of B cells 96 H&E Ileum SEM of surface of ileum Accessory Organs of the Small Intestine S Liver S Gallbladder 97 Liver S Largest gland in the body S Has 4 primary lobes S Ventral mesentery anchors liver to lesser curvature of the stomach S Digestive role = produce bile S Bile is a fat emulsifier S Also has metabolic functions 98 Liver Anatomy S Hepatic artery and hepatic portal vein enter liver at porta hepatis S Bile leaves liver through several bile ducts which fuse to form the common hepatic duct S Common hepatic duct travels towards duodenum and fuses with the cystic duct (drains gallbladder) to form the bile duct 99 S Liver lobules as structural and functional units S S S S Portal triad exist at each of the six corners to the lobules S S S Hepatic artery Hepatic portal vein Bile duct Liver sinusoids leaky capillaries found between hepatocyte cells S S S Hexagonal shaped Consist of hepatocytes “stacked” upon each other Hepatocytes radiate from a central vein Blood from hepatic artery and hepatic portal vein goes through liver sinusoids to the central vein Contains Kupffer cells which remove debris (bacteria and old blood cells) Secreted bile flows through bile canaliculi between hepatocytes towards the bile duct of the portal triads 100 101 Central Vein of Liver Bile S Yellow-green alkaline solution S Contains bile salts, bile pigments, cholesterol, triglycerides, phospholipids and electrolytes S Only bile salts and phospholipids help in the digestive process S Major mechanism of cholesterol elimination from the body S Too much cholesterol or low levels of bile salts cholesterol crystallization = gallstones 102 Bile salts S Cholesterol derivatives S Emulsify fats S Facilitate fat and cholesterol absorption S Help solubilize cholesterol S Not excreted but rater recycled via enterohepatic circulation process S Bile salts reabsorbed by the ileum S Returned to liver via hepatic portal blood S Resecreted in newly formed bile 103 Bilirubin S Primary bile pigment S Waste product of the heme of hemeglobin during breakdown of old erythrocytes S Metabolized in small intestine by resident bacteria S One of its breakdown products is responsible for the brown color of feces S Absence of bile = grey-white color of feces S Not fats are being digested or absorbed 104 Gallbladder S Thin-walled, green muscular sac S Stores bile S Concentrates bile (by absorbing water and some of it ions) S Contraction expels bile into the cystic duct which then flows into bile duct 105 Pancreas S Gland S Accessory digestive organ S Produces enzymes that breakdown all categories of foodstuffs S Pancreatic juice drains pancreas via main pancreatic duct which fuses with the bile duct (hepatopancreatic ampulla) as it empties into the duodenum S Smaller accessory pancreatic duct empties directly into duodenum 106 S Acini clusters of secretory cells surrounding ducts S Full of rough endoplasmic reticulum S Islets of Langerhans S Scattered among the acini cells S Endocrine glands S Release insulin and glucagon 107 Pancreas Cells 108 Pancreas Highly vascularized clusters of endocrine cells called Islets of Langerhans (endocrine pancreas) surrounded by more abundant acinar cells (exocrine pancreas) 109 Immunocytochemistry Identifies Which Islet Cell Secretes a Given Hormone Beta Cells Delta Cells Alpha Cells 110 F Cells Pancreatic Juice S Mostly water, enzymes and electrolytes S Acinar cells produce enzyme-rich component S Epithelial cells lining pancreatic duct release bicarbonate ions to make it alkaline S Amount of HCl produced in the stomach is exactly matched to the amount of bicarbonate secreted by the pancreas 111 S Pancreatic proteases are released in inactive form and activated in the duodenum S Prevents pancreas from digesting itself endopeptidase S Trypsinogen trypsin S Endopeptidase is an intestinal brush border protease S Trypsin activates more trypsinogen S Trypsin also activates procarboxypeptidase and chymotrypsinogen to carboxypeptidase and chymotrypsin, respectively S Amylases, lipases and nucleases released in active form 112 Small Intestine 113 Regulation of Bile and Pancreatic secretions S Bile salts are major stimulus for bile secretion S As more bile salts are recycled, more bile is secreted S Secretin released from intestine also stimulates liver cells to secrete bile S Live continuously makes bile, but it’s not released until gallbladder contracts S CCK (intestinal enzyme) is major stimulus for gallbladder contraction S CCK released into blood when acidic fatty chyme enters duodenum 114 CCK S Stimulates gallbladder to contract S Stimulates secretion of pancreatic juice S Relaxes hepatopancreatic sphincter so that bile and pancreatic juice enters duodenum S Stimulates acini to release enzyme-rich pancreatic juice S Potentiates effects of secretin 115 Secretin S Released in response to HCl in intestine S Targets pancreatic duct cells for a bicarbonate-rich pancreatic juice 116 117 Roles of gastrin, secretin and cholecystokinin in digestion S 118 Large Intestine S Frames small intestine S Extends from ileocecal valve to the anus S Major digestive function is to absorb remaining water S Stores food residues temporarily S Eliminates remaining food residues in the form of feces S Not essential for life (nor major digestion occurs here) S Removal (which may occur in cases of colon cancer) does not inhibit life 119 Anatomical modifications of the Large Intestine S Teniae coli S The three bands which represent the reduction of the longitudinal layer of the muscularis S Haustra S Pocket-like sacs S Tone of teniae colie causes haustra S Epiploic appendages S Small fat-filled pouches of visceral peritoneum that hang from the surface of the large intestine S Significance is unknown 120 Large Intestine 121 Subdivisions S Cecum S Appendix S Colon S Rectum S Anal canal 122 Appendix S Contains masses of lymphoid tissue (part of MALT) S Small and twisted infection likely S Appendicitis inflammation of the appendix S Blockage that traps bacteria in the appendix S Appendix swells cuts off blood supply appendix decays S If rupture peritonitis (infection of peritoneum) 123 124 Colon S Ascending colon S Right colic/hepatic flexure S bend between ascending and transvers colon S Transverse colon S Left colic/splenic flexure S Bend between transverse and descending colon S Descending colon S Sigmoid colon S S-shaped S In the pelvis 125 126 Rectum S Located in the pelvis S Three lateral curves S Internally, these curves present as three transverse folds called rectal valves S Rectal valves separate feces from flatus (gas) S Prevent feces from being passed along with gas 127 128 129 Anal Canal S Located in the perineum S 2 sphincters S Internal anal sphincter S Involuntary S Smooth muscle S External anal sphincter S Voluntary S Skeletal muscle 130 131 Microscopic Anatomy S Mucosa is simple columnar epithelium except in the anal canal S No villi S No cells that secrete digestive enzymes S Thicker mucosa S Deeper crypts S Large number of goblet cells in crypts 132 S Mucosa of anal canal is stratified squamous epithelium (increased abrasion) S Anal canal hangs in longitudinal folds called anal columns S Anal sinuses are between the anal columns S Secrete mucus to ease feces movement 133 Motility S Fecal matter stays in large intestine for 12-24 hours S Haustral contractions slow segmenting movements S More frequent (every 30 minutes) S Mass movements long, slow-moving, powerful contractile waves over large areas of the colon S Less frequent (3-4 times a day) S Usually occur during or just after eating S Fiber increases strength of contractions and softens stool 134 Defecation S When mass movements force feces into rectum, rectal wall stretches and initiates defecation reflex S Sigmoid colon and rectum contract S Internal anal sphincter relaxes S If defecation is delayed reflex contractions end 135 136 Diarrhea and Constipation S Diarrhea S Watery stools S Results from any condition that rushes food through the large intestine (reduced time to absorb water) S Dehydration and electrolyte imbalance S Constipation S Hard stools S When feces remains in the large intestine too long S Lack of fiber, improper bowel habits, lack of exercise, emotional upset or laxative abuse 137 Chemical Digestion and Absorption S Chemical digestion is a metabolic process in which large food molecules are broken down to monomers S Hydrolysis enzymatic breakdown of food molecule S Involves addition of water molecule to each bond being broken 138 Carbohydrates S Broken down to monosaccharaides S Includes starch S Indigestible carbohydrates (cellulose) act as bulk and help move foodstuffs along the GI tract S Chemical digestion begins in the mouth with salivary amylase S Amylase works best in slightly acidic to neutral environment S Inactivated by stomach acid 139 S Digestion continues in small intestine with aid of pancreatic amylase S Amylases convert starch to oligosaccharides S Intestinal brush border enzymes convert oligosaccharides to monosaccharaides S Dextrinase, glucoamylase, maltase, sucrase, lactase S Digestion of carbohydrates ends with the small intestine (no digestion in large intestine) 140 141 Proteins S Digested to its amino acid monomers S Digestion begins in the stomach S Pepsinogen from chief cells is activated to pepsin which digests proteins S Optimal functioning in acidic environment (low pH) S Inactivated by high pH in duodenum S Activity restricted to stomach 142 S Trypsin and chymotrypsin from the pancreas continue to cleave protein bonds into smaller peptide bonds in the intestine S Carboxypeptidase (brush border enzyme) cleaves amino acids one-by-one at the carboxyl end S Aminopeptidase does the same from the amino end 143 144 145 Lipids S Digestion only occurs in the small intestine S Pancreas provides lipase S Triglycerides are insoluble in water, therefore “pre-treated” with bile salts S S S Bile salts emulsify and increase surface area of the triglycerides to aid in fat digestion Bile salts have both polar and nonpolar ends Polar and faces aqueous environment. Nonpolar end faces fat molecules S Digestion occurs with LIPASE. BILE SALTS DO NOT DIGEST S Breakdown into fatty acids and monoglycerides 146 147 148 Nucleic Acids S DNA and RNA in the nuclei of cells of food hydrolyzed to their nucleotide monomers S Pancreatic nucleases responsible S Nucleotides later broken down by brush border enzymes nucleosidases and phosphatases 149 150 Absorption S Most absorption complete by the time the chyme reaches the ileum S Ileum mostly responsible for reclaiming bile salts S Most nutrients absorbed via active transport S Tight junctions exist between mucosal epithelial cells, therefore nutrients must move through the cell 151 Carbohydrate Absorption S Glucose and galactose use secondary active transport (with Na+) to move into epithelial cells S Move out of epithelial cells and into blood via facilitated diffusion S Fructose moves entirely by facilitated diffusion 152 Protein Absorption S Several types of protein transporters move different amino acids S Most transporters are coupled to the active transport with Na+ S Short-chained amino acids are absorbed with H+ cotransport into the epithelial cell S Broken down to single amino acids before moving into circulation 153 Lipid Absorption S Monoglycerides and fatty acids associate with bile salts and lecithin (phospholipid) to form micelles S Micelles collections of fatty elements clustered together with bile salts S Micelles easily diffuse between microvilli S Fat absorption complete in the ileum 154 S Once inside the epithelial cells, they are resynthesized into triglycerides by the smooth ER S Triglycerides coated with a “skin” of proteins to form chylomicrons (water-soluble lipoprotein droplet) S Chylomicrons leave via exocytosis and enter lacteals to join the lymph (not blood) S Later emptied into venous blood in the neck region 155 S In the blood, chylomicrons liberate triglycerides S Triglycerides hydrolyzed to fatty acids and glycerol by lipoprotein lipase 156 Nucleic Acid Absorption S Pentose sugars, nitrogenous bases and phosphate ions from nucleotide breakdown are actively transported across epithelium by special carriers 157 Vitamin Absorption S Small intestine absorbs dietary vitamins S Large intestine absorbs K and some B vitamins S Fat soluble vitamins (A, D, E and K) dissolve in dietary fats and are absorbed in micelles S Water soluble vitamins (B and C) absorbed via diffusion or specific active or passive transporters S Exception: Vitamin B12 is very large. Requires intrinsic factor (stomach) S Intrinsic factor binds to B12. Intrinsic factor binds to its receptor in the ileum allowing for endocytosis of B12 158 Water Absorption S Mostly absorbed in the small intestine by osmosis S Osmosis in the large intestine S Water moves freely across intestinal mucosa in both directions but net osmosis occurs when there is a concentration gradient established by active transport of solutes into mucosal cells 159 160 161 162 163 General Organization and Structure of the Digestive/Alimentary tube From Kierszenbaum, 164 Basic mucosal forms: Secretory-only in stomach Protective-esophagus Absorptive/Protective- Large intestine Absorptive- entire small intestine 165