Update Pain Management
advertisement

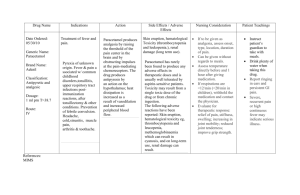
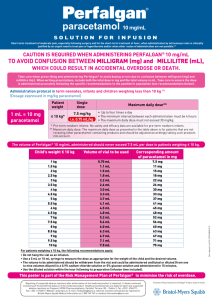
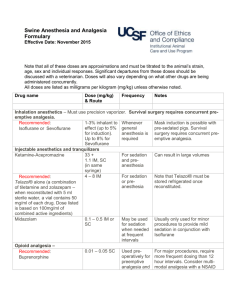
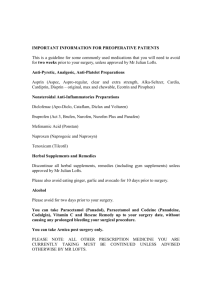
Presenter : Moderator : Dr Norlida Binti Suhaimi Dr Wan Rohaidah Intravenous Paracetamol PCA Oxynorm Bupenorphine patch Perioperative lignocaine infusion “A Fatal Accident Inquiry in Scotland in 2011 concluded that a young adult died from liver failure due to an overdose of paracetamol. The Sheriff found ‘there was, at the time of the death, a prevailing culture of assumed familiarity with the administration of IV paracetamol, a familiarity derived from the common use of oral paracetamol’. The patient, who weighed 35kg, died nine days after receiving paracetamol 1g IV on a sustained and regular basis.” IV paracetamol was licensed in the UK in 2004 and is used routinely in anaesthetic practice. Paracetamol is frequently used for perioperative analgesia, alone or in combination with an opioid. Clinical studies have shown that paracetamol has potent analgesics and reduce opioid consumption. for the short-term treatment of moderate pain especially following surgery for the short-term treatment of fever when administration by IV route is clinically justified by an urgent need to treat pain or hyperthermia and/or when other routes of administration are not possible. in patients with hypersensitivity to paracetamol in cases of severe hepatocellular insufficiency. Precautions for use: IV Paracetamol should be used with caution in cases of: hepatocellular insufficiency severe renal insufficiency (creatinine clearance ≤ 30 mL/min) chronic alcoholism chronic malnutrition (low reserves of hepatic gluthatione) Paracetamol has essentially no effect on cyclooxygenase in vitro – but it has been classified as a NSAID because of its moderate analgesic and antipyretic properties. The drug is not associated with the increased incidence of platelet dysfunction, gastritis, and renal toxicity that are sometimes associated with NSAIDs MOA Unclear it is thought to exert its analgesic activity by inhibiting the synthesis of prostaglandins in the CNS (central acting) and peripherally blocking pain impulse generation. In addition, it has been proposed that acetaminophen has a serotonergic (5-HT) mechanism and a cannabinoid agonism mechanism, which may contribute to its analgesic effect. It has been proposed that its antipyretic actions are due to : - inhibition of the hypothalamic heatregulating center, - inhibition of prostaglandin synthesis within the central nervous system , by inhibition of COX-3 (a COX – 1 ) variant. - cannabinoid agonism. The pharmacokinetics of intravenous acetaminophen have been described in several studies, and the serum therapeutic level required to produce an analgesic effect is 16 mcg/mL in adults and 10 mcg/mL in children. IV PCM has a faster onset and results in more predictable pharmacokinetic than oral or rectal PCM formulations Blood concentration Intravenous Intramuscular Effervescent tablet Suppository provides onset of pain relief within five to 10 minutes after administration. Effective concentration Tablet 1 hour 2 hours mean IV C max (maximum plasma concentration of drug) was nearly twice that observed with oral administration and nearly four times that observed with rectal administration. The lag time after oral administration is 20-30 min The lag time after rectal administration often exceeds 1 hour A major benefit is that IV PCM may be administered before or during surgery, permitting the initiation of effective analgesic therapy in the early phase of the postoperative period. When patients are able to tolerate oral intake, they may be switched from IV to oral PCM to maintain the predictable analgesia established by the IV route. Distribution: The volume of distribution of paracetamol is approximately 1 L/kg. Oral bioavailability 80% Paracetamol is not extensively bound to plasma proteins (10%) Following infusion of 1 g paracetamol, significant concentrations of paracetamol (about 1.5 μg/mL) were observed in the Cerebro Spinal Fluid as and from the 20th minute following infusion. Paracetamol metabolized by the liver mainly to glucuronide conjugates but also sulphate and cysteine conjugates These are actively excreted in the urine, only small fraction being excreted unchanged. N- acetyl-p-amino-benzoquinoneimine is a highly toxic metabolite of paracetamol that produced in small amount in therapeutic doses. It is rapidly conjugated with hepatic glutathione to render it harmless Following toxic dose – gluthatione is exhausted, NAPQI accumulates – then free to form covalent bonds with sulphydryl groups on hepatocytes resulting cell death and centrilobular hepatic necrosis Treatment: - with oral methionine(enhances gluthatione synthesis) and/or oral or IV acetylcysteine which is hydrolysed to a precursor of glutathione Composition: One ml contains 10mg paracetamol One 50 ml vial contains 500mg paracetamol One 100 ml vial contains 1000mg paracetamol The 100 ml vial or 100 ml bag is restricted to adults, adolescents and children weighing more than 33 kg. The 50 ml vial is adapted to infants, toddlers and children weighing less than 33 kg. IV Paracetamol should be given by infusion over 15 minutes minimum dose interval should not be less than four hours (six hours in patients with renal impairment). Once the vacuum seal of the glass vial has been penetrated, the dose of IV must be administered within 6 hours. IV Paracetamol is a single-use vial, and the unused portion must be discarded. To prevent the possibility of an air embolism, it is important to observe the end of the infusion can also be diluted in a 0.9% sodium chloride solution or 5% glucose solution Use the diluted solution within the hour following its preparation (infusion time included). NON–WEIGHT-BASED DOSING: For 1000 mg (10 mg/mL) doses, deliver from the bottle Use aseptic technique to prepare the vial and IV line Insert a vented IV set into upright vial; open vent Hang bottle; adjust flow for 15-minute infusion Monitor the end of the infusion in order to prevent the possibility of an air embolism WEIGHT-BASED DOSING: For extracted doses <1000 mg (10 mg/mL), deliver from separate container For small-volume pediatric doses up to 60 mL Using aseptic technique, withdraw appropriate dose from vial and into a syringe as above Administer over 15 minutes using a syringe pump Since introduction, there have been concerns about accidental overdose of IV paracetamol due to errors in drug prescription and administration, particularly in children, small adults, the elderly, alcoholics and those with pre-existing hepatocellular insufficiency. Reported errors include: - incorrect dose in adults with high or low body mass index; - accidental overdose in children associated with use of 100mlvials; - 10-fold drug calculation errors; - confusion between dose volume in millilitres and dose of drug in milligrams; - errors when setting up infusion pumps; - and duplication of doses between the ward and the operating theatre or recovery. IV paracetamol should be prescribed carefully, according to the weight, age and co-morbidities of the patient. The upper dose limit for each single dose and in each 24-hour period should not be exceeded. 50ml vials of IV paracetamol should be used for patients less than 33kg. In infants and small children, doses should be measured accurately using a syringe. Enquiry about recent paracetamol ingestion should form part of routine pre-operative assessment. All doses of paracetamol administered in the operating theatre should be recorded on the drug administration chart and in the anaesthetic record. Advice should be sought from the local poisons information service in all cases of overdose of intravenous paracetamol. Treatment with acetylcysteine is suggested following a single dose greater than 60mg/kg. IV paracetamol remains under intensive monitoring by the MHRA. All suspected adverse reactions to IV paracetamol should be reported to the Yellow Card Scheme and discussed with the local poisons information service. Oxycodone is a semi-synthetic derivatives, full opioid agonist with no antagonist properties. It has an affinity for kappa, mu and delta opiate receptors in the brain and spinal cord. Oxycodone is similar to morphine in its action. - The therapeutic effect is mainly analgesic, anxiolytic and sedative. Oxynorm… belongs to a group of medicines called strong analgesics Indication: * commonly used as an analgesic in moderate to severe acute pain * also used in moderate to severe cancer pain, and sometimes in chronic non-cancer pain Reseptor type Location Action when stimulated µ receptor *brain especially areas involved with sensory & motor perception and integration - Abundant in preaqueductal grey. *Spinal cord - analgesia - physical dependence - resp depression - reduced peristalsis - euphoria - meiosis δ receptor * brain - Analgesia - anti depressant - physical dependence Reseptor type Location Action when stimulated Ƙ receptor * Brain * Spinal cord - Spinal analgesia - Sedation - Meiosis NOP receptor ( nociceptin Orphanin FQ Peptide receptor - Most recently identified * Brain * spinal cord - Anxiety - Depression - Affect learning and memory - involved in tolerance Other pharmacological effects of oxycodone : - respiratory depression, antitussive, bronchospasm - smooth muscle (constipation, reduction in gastric, biliary and pancreatic secretions, spasm of sphincter of Oddi and transient elevations in serum amylase) - nausea and vomiting : CTZ stimulation via 5HT3 and dopamine receptors - cardiovascular system (release of histamine and/or peripheral vasodilatation, possibly causing pruritus, flushing, sweating and/or orthostatic hypotension). Opioids may influence the hypothalamic-pituitaryadrenal or –gonadal axes. - Some changes that can be seen include an increase in serum prolactin, and decreases in plasma cortisol and testosterone. Clinical symptoms may be manifest from these hormonal changes. Absorption - 40% to 85% bioavailability after oral administration - presence of methoxy group at C3 position of the phenanthrene structure protects drug against glucuronide conjugation, and hence first pass effect -100% bioavailability after iv administration Distribution: Distributed to skeletal muscle, liver, intestinal tract, lungs, spleen and brain. - tissues with mu, kappa and delta opiod receptors Pka 8.5. at pH 7.4, 7.4% unionized Vd 2-6 L/kg 45% protein binding Metabolism & Elimination: Oxycodone has an elimination half-life of approximately 3 hours metabolised principally in the liver to noroxycodone and oxymorphone. Oxymorphone has some analgesic activity but present in plasma in low concentrations and is not considered to contribute to oxycodone’s pharmacological effect. CYP3A4 and CYP2D6 are involved in the formation of noroxycodone and oxymorphone, respectively. Metabolites mainly excreted in urine and sweat, accumulates in patients with renal impairement. Concentration: Oxycodone hydrochloride 10 mg/ml Dilute to 1 mg/ml in 0.9% saline, 5% dextrose or water for injections. Setting: * Bolus doses : 0.03 mg/kg (e.g. 1-2mg per 70 kg) * lock-out time : minimum 5 minutes. * Background infusion : nil * Four hour dose limit : 30 mg Discontinuation of PCA... PCA should be discontinued when minimal use is required and the patient is able to tolerate oral analgesia Full explanation and reassurance must be given to the patient. Ensure that adequate analgesia is prescribed. Continue regular pain assessment after the pain control system has been discontinued and act accordingly. Transferring patients between oral and parenteral oxycodone… The dose should be based on the following ratio: 2 mg of oral oxycodone is equivalent to 1 mg of parenteral oxycodone. It must be emphasized that this is a guide to the dose required. Inter-patient variability requires that each patient is carefully titrated to the appropriate dose. is a semisynthetic, highly lipophilic derivative of the opium alkaloid thebain approximately 25-50 times as potent as morphine, usual dose ~ 0.3-0.6 mg Buprenorphine is a partial agonist .has high affinity for, but low intrinsic activity at, mu receptors. however, its maximal opioid effects are less than that of full agonists, and reach a ceiling where higher doses do not result in increasing effect. produces analgesia and other effects similar to morphine, including CVS peak blood concentration appear at 5 min/i.m., and at 2 hrs/s.l. or oral plasma protein binding is ~ 96% plasma half-life is ~ 3 hrs, however, the duration of action is longer, sometimes up to 6 hrs, probably due to tissue binding both N-dealkylation and conjugation occur in the liver, however most of the drug is excreted unchanged in the faeces Transdermal buprenorphine may be used in chronic severe pain when lower doses of strong opioids are indicated; especially in patients who need continuous, around-the-clock narcotic pain relief for an extended period of time. However, the place of transdermal buprenorphine in pain management is not well established. The 7-day patch formulation may have a particular role for patients who are vomiting or have swallowing difficulties. Transdermal buprenorphine is not suitable for the management of acute pain because it has a slow onset and extended duration of action. transdermal buprenorphine 5 mg (releasing buprenorphine 5 micrograms per hour) every 7 days 10 mg (10 micrograms per hour) every 7 days 20 mg (20 micrograms per hour)every 7 days Transdermal buprenorphine patches deliver buprenorphine at a constant rate over 7 days. The dose equivalence of transdermal buprenorphine and oral morphine is not established. The manufacturer suggests that the dose range covered by the three patch strengths may be equivalent to oral morphine up to 90 mg/day. Other literature and the dose relativities suggested that the buprenorphine 20-microgram-per-hour patch might be equivalent to oral morphine up to 36 mg/day or 53 mg/day Buprenorphine: a partial agonist Buprenorphine is a partial agonist so there is a ceiling dose to its analgesic effect — that is, above a certain dose there is no further analgesic effect. The dose at which this occurs in humans is not established but it is unlikely at the doses in the transdermal patches. Buprenorphine may trigger opioid withdrawal symptoms in people who have developed physical dependence on other opioids. Buprenorphine has high affinity for mu opioid receptors and is not easily displaced by opioid antagonists. Consequently, the effects of buprenorphine in overdose are only partially reversed by naloxone Buprenorphine produces typical opioid adverse effects (such as constipation, headache, nausea, vomiting, dizziness). Local irritation may occur at the application site. Buprenorphine has a long half-life, so plasma concentrations fall slowly after the patch is removed. Another opioid should not be started within 24 hours of removing a patch Dependence and abuse potential Physical dependence may develop with chronic use of buprenorphine. If a withdrawal syndrome does occur when buprenorphine is discontinued, it is usually of mild to moderate intensity, occurs within 2 days and resolves within 2 weeks. Avoid prescribing buprenorphine to people who may be dependent on other opioids because it can precipitate withdrawal symptoms, including pain. Transdermal buprenorphine may have lower abuse potential than other buprenorphine dosage forms because of the relatively low plasma concentrations achieved, the slow onset of effect and because it is likely to be difficult to extract the drug from the matrix design. Misuse could take the form of using excessive amounts of the intact patch or applying it to sites that would enhance systemic absorption. It should be used with caution in people with a past history of dependence on alcohol or other drugs. In overdose the effects of buprenorphine are only partially reversed by naloxone. The manufacturer states that the dose of naloxone should start in the usual range but that naloxone 5–12 mg intravenously may be required. Repeated naloxone doses may be needed because naloxone has a shorter duration of action than buprenorphine. Management of overdose should focus on maintaining adequate ventilation. the effect of buprenorphine on respiratory depression reaches a ceiling, with higher doses not increasing respiratory depression to a significant degree. However, if buprenorphine is used in combination with other central nervous system depressants, such as benzodiazepines, the combined effect on respiration can be life threatening. Opioid-naïve patients should start at the lowest strength. Supplemental analgesics should be continued as needed during titration because buprenorphine concentrations rise slowly. Patients converting from other opioids (up to the equivalent of oral morphine 90 mg/day) can also begin on a low strength of buprenorphine and should continue with their previous regimen during titration. The dose should be titrated to effect and should not be increased at intervals of less than 3 days. To increase the dose, remove the current patch and apply a higher strength patch or a combination of 2 patches. No more than two 20-microgram-per-hour patches should be used at once. Apply Buprenorphine patch to a hairless or nearly hairless skin site at the upper outer arm, upper chest, upper back or the side of the chest. These 4 sites (each present on both sides of the body) provide 8 possible application sites. Rotate Buprenorphine patch among the 8 described skin sites. New patches should always be applied to a different site from the previous one. Any site should not be re-used for 3–4 weeks to minimize the risk of local skin irritation immediately re-using a site can increase the rate of absorption of buprenorphine. Discuss the potential adverse effects of buprenorphine. Most adverse effects reduce with time. Constipation may persist; advise patients to drink adequate amounts of water, increase their fibre intake and remain as mobile as possible. Regular laxatives such as lactulose should be started when buprenorphine is initiated and continued for long as buprenorphine is used. Intravenous infusion of lidocaine decreases postoperative pain and speeds the return of bowel function. tested the hypothesis that perioperative lidocaine infusion facilitates acute rehabilitation protocol in patients undergoing laparoscopic colectomy. the concept of fast-track surgery has been developed to reduce postoperative morbidity and duration of hospitalization, and to accelerate postoperative recovery and convalescence. Acute rehabilitation programs combine preoperative optimization of patients’ physical and psychological status, attenuation of surgical stress, dynamic pain relief, enforced mobilization, and early oral (enteral) nutrition, as well as changes in surgical care de-emphasizing tubes and drains. Effective postoperative analgesia is key to acute rehabilitation. An alternative approach to accelerate postoperative recovery after colon surgery is administration of intravenous lidocaine, which has analgesic, antihyperalgesic, and antiinflammatory properties and has been reported to speed the return of bowel function after surgery. In a case series, acute rehabilitation after laparoscopic colectomy using intravenous lidocaine yielded outcomes similar to those reported using epidural. Furthermore,nontoxic plasma lidocaine concentrations reduce requirements for various volatile anesthetics in several animal species although the benefits in humans remain unclear. intravenous lidocaine is inexpensive, easy to administer, and relatively safe. enrolled 45 ASA status I–III patients scheduled to undergo elective laparoscopic colectomy for nonmalignant disease at the Centre Hospitalier Universitaire de Lie`ge. (Lie`ge, Belgium) Patients were enrolled from January 2003 until December 2004. Exclusion criteria : - age greater than 70 yr, - history of gastroduodenal peptic ulcer or renal failure hepatic insufficiency, - psychiatric disorder - steroid treatment - chronic treatment with opioid. - Protocol Patients fasted at least 6 h and were orally premedicated with 50 mg hydroxyzine and 0.5 mg alprazolam 2 h before surgery. Lactated Ringer’s solution (8 ml/kg/h) was infused throughout surgery. Anesthesia Patients were randomly allocated to two groups double blinded study. Just before induction of anesthesia, patients assigned to receive lidocaine (n " 22) : - given an intravenous bolus injection of 1.5 mg/kg lidocaine followed by a continuous infusion of 2 mg/kg/h. - The lidocaine infusion was continued at a rate of 1.33 mg/kg/h for 24 h postoperatively. Patients assigned to the control group (n " 23) were given equal volumes of saline General anesthesia was induced with 0.15 ug/kg sufentanil and 2 mg/kg propofol. Orotracheal intubation was facilitated with cis-atracurium, cis-atracurium was also used for intraoperative muscle relaxation full muscle relaxation during surgery Anesthesia was maintained with sevoflurane in a mixture of oxygen and air with 2 l/min fresh gas flow. Sevoflurane concentration was adjusted to maintain mean arterial pressure within 15% of the preinduction value. The use of opioid was restricted during surgery: Sufentanil, 5 ug, was injected only if mean arterial pressure increased more than 15% or if heart rate was greater than 100 beats/min despite the administration of sevoflurane to an end-tidal concentration of 3.5%. BIS was monitored allowed increases in inspired sevoflurane concentration if BIS exceeded 50. Core temperature was kept above 36.0°C using a forced-air warming system. All patients were given 0.625 mg droperidol and 2 mg tropisetron, a 5-hydroxytryptamine type 3 antagonist, as prophylaxis against postoperative nausea and vomiting 1h before the end of surgery. Surgical Procedure Two experienced laparoscopic surgeons (B.J.D., S.R.L.) performed procedures using a standard four- or fivetrocar technique. For right colectomy, after intracorporeal dissection of the ascending colon and the Bauhin valve, the specimen was exteriorized through a 5- to 6-cm minilaparotomy in the right lower abdomen. After resection of the pathologic colon, the anastomosis was hand-sewn and returned to the abdominal cavity. The minilaparotomy was then closed. In laparoscopic sigmoid colectomy, the sigmoid colon was first mobilized intracorporeally up to the rectosigmoid junction. The rectosigmoid junction was cut using a stapler. The sigmoid colon was retrieved through a 5- to 6- cm minilaparotomy in the left lower abdomen and then resected. The surgeons were unaware of the patient’s group assignment. Postoperative Analgesia Postoperative analgesia was provided in both groups by the combination of the paracetamol (acetaminophen) precursor propacetamol - 2 g propacetamol= 1 g paracetamol), 2 g intravenously 30 min before the end of surgery and then every 6 h, and ketorolac, 30 mg intravenously every 8 h. Patient-controlled analgesia with piritramide was used as rescue medication (bolus=1 mg, lockout interval =5 min, no basal infusion). Twenty-four hours after the end of surgery, the intravenous infusion of lidocaine or placebo was stopped analgesia was provided with oral paracetamol, 1 g every 6 h; - diclofenac 75 mg twice daily; - and 100 mg tramadol, if necessary. An abdominal drain was left in contact with the anastomosis for 24 h. The bladder catheter was removed on the first postoperative morning. An intravenous infusion of 5% glucose was started after surgery at a rate of 80 ml/h. Patients were allowed to drink water 6 h after surgery. If patients did not report nausea or vomiting, they were given 200 ml of nutritive supplement without residue (Clinutren® 1.5 kcal/ml; Nestle 1 h later. On the first postoperative day, patients had a light breakfast and lunch. If this food was tolerated, the intravenous infusion was stopped and a normal diet was resumed. Patients were asked to drink three 200-ml cartons of nutritive supplement each day. Active mobilization was started in bed 4 h after surgery. Assisted ambulation was enforced on the subsequent days: 20 m in the morning and 50 m in the afternoon on postoperative day 1, then 100 m in the morning and the afternoon on day 2. Defecation and tolerance of normal diet were required before discharge. Arterial pressure, heart rate, and end-tidal sevoflurane concentrations were measured on a Datex-Ohmeda S/5 monitor every 15 min during anesthesia. BIS scores were also recorded at 15-min intervals. After surgery, piritramide consumption was recorded every 4 h. Pain scores were obtained on a visual analog scale at rest, during mobilization from the supine to the sitting position, and during coughing at 2 and 6 h postoperatively and at 9:00 AM, 1:00 PM, and 5:00 PM on postoperative days 1 and 2. Postoperative fatigue scores and gastrointestinal discomfort (colic, abdominal fullness, internal discomfort) were also assessed on a visual analog scale at the same times. Times to first flatus, defecation, and hospital discharge were recorded. Episodes of postoperative nausea and vomiting were noted. Immediately after induction of anesthesia, the bladder was catheterized and emptied. In the first 30 patients (n " 15 in each group), urine was then collected to measure urinary secretion of cortisol, epinephrine, and norepinephrine to assess the stress response during anesthesia and surgery. Blood samples were drawn in the same patients before surgery and after surgery at 2, 6, 24, and 48 h. Plasma concentrations of glucose, C-reactive protein, cortisol, catecholamines, and leukocyte counts were measured. Blood samples were drawn at 5, 15, and 60 min after anesthetic induction, at the end of surgery, and 24 h after the end of surgery to measure plasma lidocaine concentrations A previous study at same institution using a similar protocol indicated that18 patients per group allowed detecting a 12-h difference in the recovery of bowel function between the groups, at an alpha level of 0.05 and with 80% power. therefore enrolled patients until 40 patients (n " 20 in each group) completed the study. Continuous variables are presented as mean ± SD; they were compared using analysis of variance for repeated measures for two criteria (time and treatment) followed by the Scheffe´ test for multiple comparisons or the Student t test, as appropriate. If the Kolmogorov-Smirnov normality test did not demonstrate gaussian distributions, the Mann–Whitney test was used; data are then presented as median [25–75% interquartile range]. Categorical data were analyzed with chi-square tests. P ≤0.05 was considered significant. Three patients in the control group, but none in the lidocaine group, requested tramadol after the interruption of piritramide patient-controlled analgesia between the 24th and 48th postoperative hours: These patients were given 100, 200, and 400 mg. patients in the lidocaine group tolerated a normal diet the day after surgery and had their intravenous infusion interrupted 24 h after surgery, whereas three patients in the control group required prolongation of postoperative fasting and intravenous infusion (31, 54, and 72 h) (P " 0.22). Four patients in the saline group but only one in the lidocaine group experienced nausea (P =0.17). Vomiting occurred in two patients in the saline group and none in the lidocaine group (P =0.23) Lidocaine plasma concentrations were measured in 15 patients and were 1.6 ±0.9 ug/ml at 5 min, 1.3 ± 0.4 ug/ml at 15 min, and 1.8 ±0.5 ug/ml at 60 min after the bolus injection of lidocaine; 2.4 ±0.6 ug/ml at the end of surgery 2.7 ±1.1 ug/ml at the end of the 24-h infusion. The highest plasma concentrations of lidocaine measured at each of these time points were 3.5, 2.1, 2.6, 4.0, and 4.6 ug/ml, respectively. This study demonstrated that perioperative intravenous infusion of nontoxic doses of lidocaine improved: - postoperative analgesia, - reduced postoperative opioid requirements, - accelerated postoperative recovery of bowel function, - attenuated postoperative fatigue, - reduced the duration of hospitalization, - facilitated acute rehabilitation in patients undergoing laparoscopic abdominal surgery. results further indicated that moderate plasma lidocaine concentrations reduced sevoflurane requirements necessary for maintaining intraoperative hemodynamic stability and anesthetic depth. Intravenous lidocaine is analgesic, antihyperalgesic, and antiinflammatory. These properties are mediated by a variety of mechanisms, including sodium channel blockade, as well as inhibition of G protein–coupled receptors and N-methyl-D-aspartate receptors. In this study, intravenous lidocaine reduced postoperative opioid consumption, as well as pain scores during activity. the analgesic effect persisted after the lidocaine infusion was discontinued, which suggests a prevention of spinal or peripheral hypersensitivity or both. Inhibition of N-methyl-D-aspartate receptors which play a major role in postoperative hyperalgesia Abdominal discomfort was significantly reduced by lidocaine, which is consistent with the ability of lidocaine to alleviate visceral pain in animal models. Systemic lidocaine also improved postoperative bowel function. Defecation occurred almost 1 day earlier in the lidocaine group. The reduction in ileus duration by intravenous lidocaine may be mediated by the reduction of postoperative opioid consumption, the antiinflammatory properties of lidocaine, and/or a direct inhibition of the sympathetic myenteric plexus. In summary, this study demonstrated that perioperative administration of low doses of intravenous lidocaine reduces intraoperative anesthetic requirements and has a clinically relevant beneficial effect on postoperative recovery after colectomy. These data suggest that intravenous local anesthetics can contribute to postoperative acute rehabilitation programs.