Making basic sciences clinically relevant
advertisement

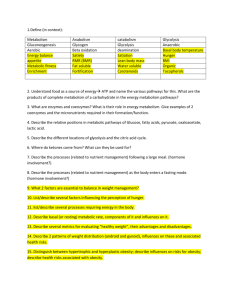
Making basic science clinically relevant for learners: the biochemistry example Eric Niederhoffer SIU-SOM Considerations • Wants and needs Curriculum design, objectives, goals; USMLE • Biochemistry as a foreign language Web lessons, resource pages, animations • Resource sessions Complement self-directed learning Applied to patient case Start simple, discuss difficult Big picture, relevant details Overlap and redundancy Build upon previous knowledge • Clinical probes for content and concepts Self-assessment questions, examinations • Glucose metabolism as an example Red Blood Cell Biochemistry A 4-year-old African boy presents with a 2-day history of painful extremities. RBC Structure - size, spectrin, channels Metabolism - glycolysis (2,3-BPG), pentose phosphate pathway (G6PDH, NADPH), glutathione Hemoglobin - Genes, heme, Mb/Hb (normal), O2 binding, HbS (defect), fibers (sickling and inflammation) Students’ Notes Red Blood Cell Biochemistry RBC Structure - size, spectrin, channels Metabolism - glycolysis (2,3-BPG), pentose phosphate pathway (G6PDH , NADPH), glutathione Hemoglobin - Genes, heme, Mb/Hb (normal), O2 binding, HbS (defect), fibers (sickling and inflammation) Eric Niederhoffer SIU-SOM Devlin, T. M. (ed.). 2006. Textbook of biochemistry with clinical correlations, 6th ed. John Wiley & Sons, Inc., New York. This is very good for most of what you need. Mehta, A. B., and A. V. Hoffbrand. 2000. Haematology at a glance, Blackwell Science, Malden, Mass. Salway, J. G. 2006. Medical biochemistry at a glance, 2nd ed. Blackwell Science, Malden, Mass. This is very good for general principles and topics, and metabolic pathways and regulation. Good focused clinical correlations. RBC Metabolic Pathways GSH Glc G6P NADP+ + H+ PGI GSSG GR F6P PFK NADPH F16BP aldolase DHAP G3P G3PDH BPG mutase 1,3-BPG PGK 2,3-BPG 3PG G6PDH lactonase 6PGDH CO2 6PG PPP PGM 2,3-BPG phosphatase 2PG enolase PEP Lactate No O2 LDH H2O GP HK Glycolysis H2O2 PK Pyr 3-7 C metabolites (R5P, F6P, G3P) Students’ Notes RBC Metabolic Pathways H2O2 GSH Glc GP HK G6P NADP + + H+ GSSG PGI GR F6P PFK Glycolysis H2O NADPH F16BP aldolase DHAP G6PDH lactonase 6PGDH G3P G3PDH BPG mutase 1,3-BPG PGK 2,3-BPG CO2 6PG PPP 3PG PGM 2,3-BPG phosphatase 2PG 3-7 C metabolites (R5P, F6P, G3P) enolase PEP Lactate Glc: glucose No O2 LDH PK Pyr HK: hexokinase G6P: glucose-6-phosphate G6PDH: glucose-6-phosphate dehydrogenase PGI: phosphoglucose isomerase PFK: phosphofructokinase DHAP: dihydroxyacetonephosphate BPG: bisphophoglycerate PEP: phosphoenolpyruvate Pyr: pyruvate NADP+/NADPH: nicotinamide adenine dinucleotide R5P: ribulose-5-phosphate G3P: glyceraldehyde-3-phosphate GSH: reduced glutathione (GSH = Glu-Cys-Gly) PK: pyruvate kinase (2 genes, 4 isozymes) F6P: fructose-6-phosphate GSSH: oxidized glutathione LDH: lactate dehydrogenase PPP: pentose phosphate pathway 6PGDH: 6-phosphogluconate dehydrogenase GR: glutathione reductase GP: glutathione peroxidase 3PG: 3-phosphoglycerate 6PG: 6-phosphogluconate Defect in HK, PGI, aldolase, or BPG mutase/2,3-BPG phosphatase decreased [2,3-BPG]; defect in PK increased [2,3-BPG] BPG mutase(or synthase)/2,3-BPG phosphatase is a bifunctional enzyme (one protein, two activities), regulated by hypoxia and T3 MIultiple inositol polyphosphate phosphatase acts on 2,3-BPG to give 2-PG Fetal Hb - lower affinity for 2,3-BPG compared with adult Hb; 2,3-BPG binds to and stabilizes deoxyHb; it is easily displaced from oxyHb Common deficiencies: G6PDH - X-linked PGI - autosomal recessive Sodium fluoride inhibits enolase, used to preserve blood samples for glucose determinations. PK - autosomal recessive Hemoglobin Structure Changes http://www.mfi.ku.dk/PPaulev/chapter8/images/8-3.jpg Factors Affecting Binding of O2 Depends on pH ([H+]), CO2, BPG (DPG), Temp pH BPG or T _; left shift pH _ BPG or T ; right shift Review Questions • What metabolic pathways are used in erythrocytes? • What clinical observations would you make concerning patients with SCD? Metabolism in Skeletal Muscle and Nervous Tissue • Metabolism in skeletal muscle • Pathways overview • Regulation in skeletal muscle • Metabolism in nervous tissue • Pathways overview • Clinical aspects • Clinical aspects • Clinical/laboratory findings • GSD, PDHCD • Glycogen storage disease type VII • Pyruvate dehydrogenase complex deficiency • Inborn errors of metabolism Metabolism in Skeletal Muscle A 21-year-old woman comes to the physician with pain in her right mid-arm. A 5-year-old boy is brought to the physician to have sutures removed. • Glycolysis • Glycogenolysis -oxidation (ketone bodies) • Krebs (tricarboxylic acid) cycle • Branched-chain amino acids • Electron transport chain • Calcium regulation • Key enzyme regulation Pathways Overview Ketone bodies Fatty acids Glucose Glycogen Glycolysis Glycogenolysis Ca2+ PKa Lactate No O2 BCAA Ile, Leu, Val G6P Pyruvate Krebs cycle -Oxidation Ca2+ PDH Acetyl-CoA Ca2+ ISDH, aKGDH Production of ATP Electron Transport Chain Regulation in Skeletal Muscle Ep AR Glc Glycolysis ATP Citrate AC cAMP PKA ATP Ca2+ PKa G6P F6P PP PFK-2 PFK-1 Pi IMP AMP NH4+ AMP Pi F16BP Glycogen Glycogenolysis PEP PK PDHP Ca2+ PDHP PDHK PDH F26BP Pyr PDH Acetyl-CoA Metabolism in Nervous Tissue A 21-year-old woman comes to the physician with pain in her right mid-arm. A 19-year-old man is brought to the emergency department after a diving accident. A 63-year-old woman is brought to the physician for her “parkinsonism.” • Glycolysis • Glycogenolysis (stress) -oxidation (ketone bodies) • Krebs (tricarboxylic acid) cycle • Branched-chain amino acids • Electron transport chain Pathways Overview Glucose Glycogen Glycolysis Glycogenolysis Lactate (glial) Lactate No O2 BCAA Ile, Leu, Val Fatty acids Ketone bodies -oxidation G6P Pyruvate Acetyl-CoA Krebs cycle Production of ATP Electron Transport Chain Clinical Aspects for Inborn Errors of Metabolism in Muscles Toxic accumulation disorders • Protein metabolism disorders (amino acidopathies, organic acidopathies, urea cycle defects) • Carbohydrate/intolerance disorders • Lysosomal storage disorders Energy production/utilization disorders • Fatty acid oxidation defects • Carbohydrate utilization, production disorders (glycogen storage, gluconeogenesis, and glycogenolysis disorders) • Mitochondrial disorders • Peroxisomal disorders • Metabolic acidosis (elevated anion gap) • Hypoglycemia • Hyperammonemia Clinical Aspects for Inborn Errors of Metabolism in Nervous Tissue Evidence of familial coincidence Progressive decline in nervous functioning Appearance and progression of unmistakable neurologic signs General symptoms • State of consciousness, awareness, reaction to stimuli • Tone of limbs, trunk (postural mechanisms) • Certain motor automatisms • Myotatic and cutaneous reflexes • Spontaneous ocular movements, fixation, pursuit; visual function • Respiration and circulation • Appetite • Seizures Clinical/Laboratory Findings Clinical findings AA OA UCD CD GSD FAD LSD PD MD Episodic decompensation X + ++ + X + - - X Poor feeding, vomiting, failure to thrive X + ++ + X X + + + Dysmorphic features and/or skeletal or organ malformations X X - - X X + X X Abnormal hair and/or dermatitis - X X - - - - - - Cardiomegaly and/or arrhythmias - X - - X X + - X Hepatosplenomegaly and/or splenomegaly X + + + + + + X X Developmental delay +/neuroregression + + + X X X ++ + + Lethargy or coma X ++ ++ + X ++ - - X Seizures X X + X X X + + X Hypotonia or hypertonia + + + + X + X + X Ataxia - X + X - X X - - Abnormal odor X + X - - - - - - Primary metabolic acidosis X ++ + + X + - - X Primary respiratory alkalosis - - + - - - - - - Hyperammonemia X + ++ X - + - - X Hypoglycemia X X - + X + - - X Liver dysfunction X X X + X + X X X Reducing substances X - - + - - - - - Ketones A H A A L/A L A A H/A Laboratory Findings* Glycogen Storage Disease Pyruvate Dehydrogenase Complex Deficiency Glucose Glycogen Glycogenolysis Glycogenesis G6P Pentose Phosphate Pathway R5P nucleotides Glycolysis F6P PFK Tarui disease Glycogen Storage Disease Type VII F16BP Pyruvate PDH complex deficiency PDH Acetyl-CoA Krebs cycle Glycogen Storage Disease Type VII (Tarui Disease) Classic, infantile onset, Late onset Exercise intolerance, fatigue, myoglobinuria Phosphofructokinase • Tetramer of three subunits (M, L, P) • Muscle/heart/brain - M4; liver/kidneys - L4; erythrocytes - M4, L4, ML3, M2L2, M3L General symptoms of classic form • Muscle weakness, pronounced following exercise • Fixed limb weakness • Muscle contractures • Jaundice • Joint pain Laboratory studies • Increased serum creatine kinase levels • No increase in lactic acid levels after exercise • Bilirubin levels may increase • Increased reticulocyte count and reticulocyte distribution width • Myoglobinuria after exercise • Ischemic forearm test - no lactate increase with ammonia increase Pyruvate Dehydrogenase Complex Deficiency Neonatal, infantile, childhood onset Abnormal lactate buildup (mitochondrial disease) Pyruvate dehydrogenase complex • E1 - a (thiamine dependent) and subunits, a22 tetramer • E2 - monomer (lipoate dependent) • E3 - dimer (riboflavin dependent) common to aKGDH and BCAKDH • X protein - lipoate dependent • Pyruvate dehydrogenase phosphatase Nonspecific symptoms (especially with stress, illness, high carbohydrate intake) • Severe lethargy, poor feeding, tachypnea • Key feature is gray matter degeneration with foci of necrosis and capillary proliferation in the brainstem (Leigh syndrome) • Infants with less than 15% PDH activity generally die Developmental nonspecific signs • Mental delays • Psychomotor delays • Growth retardation Laboratory studies • High blood and cerebrospinal fluid lactate and pyruvate levels • Elevated serum and urine alanine levels • If E2 deficient, elevated serum AAs and hyperammonemia • If E3 deficient, elevated BCAA in serum, aKG in serum and urine Inborn Errors of Metabolism Carbohydrates (Glycogen storage diseases) Amino acids (Maple syrup urine disease) Organic acids (Alkaptonuria) Mitochondrial function (Pyruvate dehydrogenase deficiency) Purines and pyrimidines (Lesch-Nyhan disease) Lipids (Familial hypercholesterolemia) Porphyrins (Crigler-Najjar syndromes) Metals (Hereditary hemochromatosis) Peroxisomes (X-linked adrenoleukodystrophy) Lysosomes (GM2 gangliosidoses - Tay Sachs disease) Hormones (hyperthyroidism) Blood (Sickle cell disease) Connective tissue (Marfan syndrome) Kidney (Alport syndrome) Lung (a1-antitrypsin deficiency) Skin (Albinism) Review Questions • How does muscle produce ATP (carbohydrates, fatty acids, ketone bodies, branched-chain amino acids)? • How is skeletal muscle phosphofructokinase-1 regulated? • What are the key Ca2+ regulated steps? • How does nervous tissue (neurons and glial cells) produce ATP (carbohydrates, fatty acids, ketone bodies, branched-chain amino acids)? • How do glial cells (astrocytes) assist neurons? • What are some key clinical features (history, physical, laboratory test results) associated with defects in metabolism that affect muscles and nervous tissue? Carbohydrate Metabolism in Diabetes A 59-year-old man is brought to the emergency department for evaluation of his semiconsciousness and minimal responsiveness • For the third example taken from the ERG Unit, what would you choose for the resource session? Carbohydrate Metabolism in Diabetes • Regulation of glycolysis, glycogenesis, glycogenolysis, gluconeogenesis by insulin/glucagon PFK-2 (PKA, AMP-dependent PK) PK (PKA) PDH GS (PKA, PPK, GSK-3, PP-1) GP (PKA, PPK, PP) PEPCK (glucagon) G6Pase (glucagon) • Regulatory differences among tissues Liver Muscle Cardiac muscle • Key clinical features (history, physical, laboratory test results) associated with carbohydrate metabolism that occur in diabetes Summary • Remember curriculum wants and needs • Practice new language skills • Use resource sessions effectively Complement self-directed learning Applied to patient case Start simple, discuss difficult Big picture, relevant details Overlap and redundancy Build upon previous knowledge • Clinical probes for content and concepts