Respiratory Pharmacology Week 6
advertisement

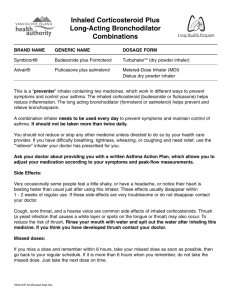
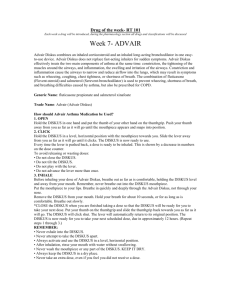
Respiratory Pharmacology Week 6 Inhaled Steroids Mode of action at the tissue level ◦ Restoration of epithelium ◦ Reduction of thickening of basement membrane ◦ Reduction of mucosal edema ◦ Reduction of leukocyte infiltrate ◦ Reduction of mast cell number Inhaled Steroids Mode of action at the molecular level: ◦ Blockage of active sites of pro-inflammatory genes Mode of action at the cellular level: ◦ Inhibition of release of pro-inflammatory molecules Inhaled Corticosteroids Mode of action ◦ Modify response of the cell in order to inhibit inflammatory response of the airway ◦ May require hours to days to gain full benefits ◦ Daily compliance is essential to maximizing effects Inhaled Corticosteroids Indications ◦ Anti-inflammatory maintenance therapy of persistent asthma and COPD ◦ Control of seasonal allergic or non-allergic rhinitis ◦ May be administered as orally inhaled aerosol or intranasal aerosol ◦ http://www.youtube.com/watch?v=LcM7f1iwOGo Aerobid is now Aerospan Flovent: DPI/MDI. 3 doses. Asmanex: twisthaler, grey or pink depending on dose Qvar: 40/80 ug dose Advair: MDI or DPI, 3 doses, combo drug Symbicort: 2 doses, combo drug Pulmicort: turbahaler or respules Inhaled Corticosteroids Adverse effects ◦ Decrease type and severity of side effects compared to systemic administration ◦ Adrenal insufficiency ◦ Acute asthma Inhaled Corticosteroids Adverse effects (systemic mostly) ◦ Osteoporosis ◦ Growth suppression ◦ Oropharyngeal infections Inhaled Corticosteroids Adverse effects ◦ Dysphonia ◦ Cough ◦ Bronchoconstriction Corticosteroids Used in Aerosol Administration Beclomethasone dipropionate QVAR MDI: 40 and 80 µg/puff. Adults > 12 years: 40 to 80 µg twice daily, or 40 to 160 µg twice daily Children > 5 years: 40 to 80 µg twice daily Triamcinolone acetonide (No longer made) Azmacort MDI: 100 µg/puff. Adults > 12 years: 2 puffs three times of four times daily Children > 6 years: 1 or 2 puffs three or four times daily Flunisolide (No longer made) Aero-Bid MDI: 250 µg/puff Adults and children > 6 years: 2 puffs twice daily; adults no more than 4 puffs; children < 15 years no more than 2 puffs daily Corticosteroids Used in Aerosol Administration Fluticasone propionate Flovent MDI: 44, 110, and 220 µg/puff Adults > 12 years: 88 µg twice daily; 88 – 220 µg twice daily; or 880 µg twice daily Children 4 – 11 years: 88 µg twice daily DPI: 50, 100, and 250 µg Adults: 100 µg twice daily; 100 – 250 µg twice daily; or 1000 µg twice daily Children 4 – 11 years: 50 µg twice daily Budesonide Pulmicort DPI: 200 µg/actuation Adults: 200 – 400 µg twice daily; 400 – 800 µg twice daily Children > 6 years: 200 µg twice daily SVN: 0.25 mg/2 ml; 0.5 mg/2 ml Children 1 – 8 years: 0.5 mg total dose once daily or twice daily in divided doses 1 mg given as 0.5 mg twice daily or once daily Corticosteroids Used in Aerosol Administration Fluticasone propionate/ salmeterol Advair Diskus Budesonide / formoterol fumarate Symbicort Advair HFA DPI: 100 µg fluticasone / 50 µg salmeterol 250 µg fluticasone / 50 µg salmeterol 500 µg fluticasone / 50 µg salmeterol Adults and children > 12 years: 100 µg fluticasone / 50 µg salmeterol, one inhalation twice daily, about 12 hours apart Children > 4 years: 100 µg fluticasone / 50 µg salmeterol, one inhalation twice daily, about 12 hours apart MDI: 45 µg fluticasone / 21 µg salmeterol 115 µg fluticasone / 21 µg salmeterol 230 µg fluticasone / 21 µg salmeterol Adults and children > 12 years: 2 inhalations twice daily, about 12 hours apart MDI: 80 µg budesonide / 4.5 µg formoterol 160 µg budesonide / 4.5 µg formoterol Adults and children > 12 years: 160 µg budesonide / 9 µg formoterol twice daily; maximum daily: 640 µg budesonide / 18 µg formoterol Advair Advair Diskus combines an inhaled corticosteroid and an inhaled long-acting bronchodilator in one easy-to-use device. Advair Diskus does not replace fast-acting inhalers for sudden symptoms. Advair Diskus effectively treats the two main components of asthma at the same time: constriction, the tightening of the muscles around the airways, and inflammation, the swelling and irritation of the airways. Constriction and inflammation cause the airways to narrow and reduce airflow into the lungs, which may result in symptoms such as wheezing, coughing, chest tightness, or shortness of breath. The combination of fluticasone (Flovent-steroid) and salmeterol (Serevent-bronchodilator) is used to prevent wheezing, shortness of breath, and breathing difficulties caused by asthma, but also be prescribed for COPD. Advair Generic Name: fluticasone propionate and salmeterol xinafoate Trade Name: Advair (Advair Diskus) How should Advair Asthma Medication be Used? 1. OPEN Hold the DISKUS in one hand and put the thumb of your other hand on the thumbgrip. Push your thumb away from you as far as it will go until the mouthpiece appears and snaps into position. 2. CLICK Hold the DISKUS in a level, horizontal position with the mouthpiece towards you. Slide the lever away from you as far as it will go until it clicks. The DISKUS is now ready to use. Every time the lever is pushed back, a dose is ready to be inhaled. This is shown by a decrease in numbers on the dose counter. Advair To avoid releasing or wasting doses: • Do not close the DISKUS. • Do not tilt the DISKUS. • Do not play with the lever. • Do not advance the lever more than once. 3. INHALE Before inhaling your dose of Advair Diskus, breathe out as far as is comfortable, holding the DISKUS level and away from your mouth. Remember, never breathe out into the DISKUS mouthpiece. Put the mouthpiece to your lips. Breathe in quickly and deeply through the Advair Diskus, not through your nose. Combos Symbicort (Contains formoterol, a long-acting beta -adrenergic 2 agonist (LABA) and budesonide (steroid); given BID, two doses 160/4.5 mcg, 80/4.5 mcg; MDI) Dulera (mometasone furoate/ formoterol fumarate dihydrate, BID, 100/5 or 200/5 mcg dose MDI) Non-Steroidal Anti-Asthma Drugs Mast cell stabilizers ◦ Indicated for prophylactic control of mild to moderate asthma ◦ Inhibits degranulation of mast cells in response to allergic and non-allergic stimuli ◦ Used typically as alternatives to inhaled corticosteroids, especially in children Non-Steroidal Anti-Asthma Drugs Leukotriene inhibitors ◦ Indicated for prophylactic control of mild to moderate asthma ◦ Used in combination with inhaled steroids to reduce the dose of the steroid Non-Steroidal Anti-Asthma Drugs Cromolyn sodium Intal Nasalcrom MDI: 800 µg / actuation Adults and children > 5 years: 2 inhalations four times daily SVN: 20 mg / ampule or 20 mg / 2 ml Adults and children > 2 years: 20 mg inhaled four times daily Spray: 40 mg / ml (4%) Adults and children > 2 years: 1 spray each nostril, 3 to 6 times daily every 4 – 6 hours Nedocromil sodium Tilade MDI: 1.75 mg / actuation Adults and children > 6 years: 2 inhalations four times daily Zafirlukast Accolate Tablets: 10 and 20 mg Adults and children > 12 years: 20 mg twice daily, without food Children 5 – 11 years: 10 mg twice daily Non-Steroidal Anti-Asthma Drugs Montelukast Singulair Tablets: 10 mg; 4 and 5 mg chewable; 4 mg packet of granules: Adults and children > 15 years: one 10 mg tablet daily Children 6 – 14 years: one 5 mg chewable tablet daily Children 2 – 5 years: one 4 mg chewable tablet daily Children 6 – 23 months: one 4 mg packet of granules daily Zileuton Zyflo Tablets: 600 mg Adults and children > 12 years: one 600 mg tablet four times per day Aerosolized Anti-Infective Agents Pentamidine isethionate (Nebupent) ◦ Indicated for the prevention of Pneumocystis carinii pneumonia (PCP) ◦ Not recommended for use in treatment of PCP (however typically given) Pentamidine Isethionate (Nebupent) Action: The drug interferes with protozoal nuclear metabolism inhibitionof DNA, RNA, phospholipid and protein synthesis. It is known to have activity against pneumocystis carinii. Indication: Prevention of Pneumocystis carinii pneumonia (PCP) in high risk, HIV-infected patients. Dosage: 300mg once every 4 weeks (nebulized) Pneumocystis pneumonia (PCP) Pneumocystis pneumonia (PCP) form of pneumonia, caused by the yeast-like fungus (which had previously been erroneously classified as a protozoan) Pneumocystis jirovecii Pneumocystis is commonly found in the lungs of healthy people, but being a source of opportunistic infection it can cause a lung infection in people with a weak immune system. Pneumocystis pneumonia is especially seen in people with cancer, HIV/AIDS and the use of medications that affect the immune system. also known as Pneumocystis jiroveci[i] pneumonia Pentamidine Isethionate Adverse effects ◦ Cough ◦ Bronchial irritation, bronchospasm ◦ Shortness of breath ◦ Given using a scavenger nebulizer/SPAG Pentamidine Isethionate Adverse effects ◦ Fatigue ◦ Pharyngitis ◦ Chest Pain Aerosolized Anti-Infective Agents Ribavirin (Virazole) ◦ Indicated as anti-viral agent to treat respiratory syncytial virus (RSV) ◦ Administered via small particle aerosol generator (SPAG) Ribavirin-injection Ribavirin is also used with an interferon medication to treat hepatitis C in people who have not been treated with an interferon before. Ribavirin is in a class of antiviral medications called nucleoside analogues. It works by stopping the virus that causes hepatitis C from spreading inside the body. It is not known if treatment that includes ribavirin and another medication cures hepatitis C infection, prevents liver damage that may be caused by hepatitis C, or prevents the spread of hepatitis C to other people. Ribavirin Adverse effects ◦ Skin rash ◦ Eyelid erythema ◦ Occlusion of endotracheal tube ◦ Deterioration of pulmonary function Aerosolized Anti-Infective Agents Tobramycin (Tobi) ◦ Indicated for management of chronic infection with Pseudomonas aeruginosa; typically seen with CF and immune suppressed patients ◦ Treat or prevent colonization Tobi Action: Aminoglycoside antibiotic disrupts protein synthesis eventually resulting in cell death (gram negative organisms). Dosage: One 5 mL ampule contains 300mg of tobramycin. Given B.I.D. / Q12 with recommended nebulizer (Pari type neb) Tobramycin Adverse effects ◦ Ototoxicity and tinnitus ◦ Bronchospasm ◦ Fetal harm (deafness) Aerosolized Anti-Infective Agents Zanamivir (Relenza) ◦ Indicated for treatment of uncomplicated illness due to influenza virus Relenza used in the treatment and prophylaxis of influenza caused by influenza A virus and influenza B virus. The bioavailability of zanamivir is 2%. After inhalation, zanamivir is concentrated in the lungs and oropharynx, where up to 15% of the dose is absorbed and excreted in urine. Dosing is limited to the inhaled route. This restricts its usage, as treating asthmatics could induce bronchospasms Zanamivir Adverse effects ◦ Bronchospasm ◦ Under treatment of bacterial infection appearing as viral infection Aerosolized Anti-Infective Agents Amphotericin B ◦ Indicated for the treatment of fungal infections, especially in lung transplants amphotericin B amphotericin B binds the main component of fungal cell membranes, forming a transmembrane channel that leads to monovalent ion (K+, Na+, H+ and Cl−) leakage, which is the primary effect leading to fungal cell death. Amphotericin B Adverse effects ◦ Nausea ◦ Vomiting ◦ Bronchoconstriction Aerosolized Anti-Infective Agents Pentamidine isethionate Nebupent 300 mg powder in 6 ml sterile water, once every four weeks Ribavirin Virazole 6 g powder in 300 ml sterile water (20 mg / ml solution); given every 12 – 18 hr / day for 3 – 7 days by SPAG Tobramycin TOBI 300 mg / 5 ml ampule: Adults and children > 6 years: 300 mg bid, 28 days on drug, 28 days off drug Zanamivir Relenza DPI: 5 mg / inhalation: Adults and children > 7 years: 2 inhalations (one 5 mg blister / inhalation) bid, 12 hours apart for 5 days Amphotericin B Fungizone 10 mg three times per day for six to 8 weeks Nitric Oxide Indicated for the treatment of pulmonary hypertension in neonates Causes relaxation of vascular smooth muscle, producing pulmonary vasodilation Nitric Oxide Contraindicated in neonates with right to left shunts Nitric Oxide Adverse effects ◦ Hypotension ◦ Formation of Methemoglobinia ◦ Withdrawal