CONTRACEPTION
advertisement
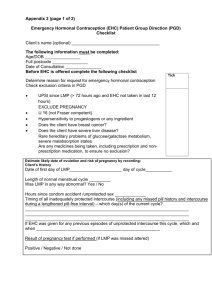
Prof. Roshan Ara Qazi Chairperson Obstetrics & Gynaecology LUMHS, Jamshoro The student will be able to: Describe contraception, importance of family planning & concept of “healthy timing & spacing of pregnancy” (HTSP) Describe major family planning methods including mechanism of action, benefits & limitations Contraception: Intentional prevention of conception or impregnation through use of various devices, agents, drugs, sexual practices or surgical procedures. Family Planning: It allows people to attain their desired number of children and determine the spacing of pregnancies. It is achieved through use of contraception 1) 2) In June 2005, WHO brought together more than 30 technical experts to review the global scientific evidence regarding optional birth spacing & answer the following questions Does pregnancy spacing affect the health of mothers and newborn? How long should a woman wait to get pregnant after childbirth? 3) How long should a woman wait to get pregnant after miscarriage or induced abortion? The set of recommendation called healthy timing & spacing of pregnancy is based on the results of this technical consultation. Ref: WHO 2006; Report of a WHO technical consultation on birth spacing, Geneva, Switzerland, 13-15 June 2005, WHO Geneva Short birth intervals are associated with multiple adverse outcomes for mothers & newborns An infant born after short birth interval is at increased risk of ◦ ◦ ◦ ◦ Preterm birth Low birth weight Small for gestational age Death A women who becomes pregnant too quickly following previous birth/miscarriage or induced abortion faces higher risks of ◦ ◦ ◦ ◦ Anemia Pre rupture of membranes Abortion Death AFTER LIVE BIRTH The recommended interval before attempting the next pregnancy is at least 24 months in order to reduce the risk of advise maternal perinatal & infant outcomes AFTER MISCARRIAGE OR INDUCED ABORTION The recommended minimum interval to next pregnancy should be at least 6months in order to reduce the risk of adverse maternal and perinatal outcomes DELAY ADOLESCENCE PREGNANCY Delay timing of the first pregnancy until age 18 to reduce risks of adverse maternal, perinatal & infant outcomes 6th most populous country of Pakistan with high unmet need of family planning about 25% Approximately 1 in 3 births occurs less than 24 months after a previous birth The shortest birth intervals occurs in women ages 15 – 19 who are already at highest risk of pregnancy related complications The client will be given full information about optimal pregnancy spacing and the benefits of HTSP as a part of FP health education and counseling. The importance of timely initiation of an FP method after childbirth, miscarriage, or abortion will be emphasized The client’s right to make a free and informed choice regarding eventual family size and fertility will be respected. Combined hormonal contraception Progestogen – only preparations ◦ The pill, patches, the vaginal ring ◦ Progestogen-only pills, injectables, subdermal implants Hormonal emergency contraception Intrauterine contraception Barrier Methods Sterilization (Voluntary Surgical Contraception) ◦ Copper intrauterine device (IUD), hormone-releasing intrauterine system (IUS) ◦ Condoms, female barriers, coitus interruptus, natural family planning ◦ Female sterilization, vasectomy Method of contraception Combined oral contraceptive pill Progestogen – only pill Depo – Provera ® Implanon Copper IUD Mirena Male condom Diaphragm Failure rate per 100 woman years 0.1 – 1 1–3 0.1 – 2 0.1 1–2 0.5 2–5 1 – 15 Natural family planning 2–3 Vasectomy 0.02 Female sterilization 0.13 A) B) Lactational Amenorrhea Method (LAM or Breastfeeding) Fertility awareness-based method 1) Calendar Based Method • Calendar based method • Standard days method (SDM) 2) Symptoms Based Methods • Ovulation method / cervical mucus method • Basal Body Temperature (BBT) method 3) Withdrawal Method Helps a couple know which days they should not have unprotected intercourse For women with menstrual cycles between 26 and 32 days long Couples who can avoid unprotected intercourse from day 8-19 Keeping a record of at least 6 menstrual cycles. Find the longest and shortest of the menstrual cycle Subtract 18 from the number of days in the shortest cycle to find the first fertile day of a current cycle. (e.g. 28-18=10days) Subtract 11 from the number of days in the longest cycle to find the last fertile day of a cycle. (e.g. 30-11=19days) Preventing pregnancy by breast feeding Mechanism of action: ovulation prevention Very effective: 1-2 pregnancies / 100 women in firs 6 months No side effects or health risks Health benefits for the baby Women who: ◦ Are fully or nearly fully breastfeeding ◦ Have not had return of menses ◦ Are less than 6 months postpartum Shift in BBT to identify post ovulatory infertile (safe) days Take temperature every morning before any activity Recorded daily on a graph paper Within twelve hours of ovulation , the BBT will rise (0.4 to 1 F) until start of next cycle Based Body Temperature Presence or absence of cervical mucus ◦ Dry (safe) days ◦ Wet (fertile) days Note mucus for: ◦ Color (yellow, white, clear, cloudy) ◦ Consistency (thick, sticky, stretchy) ◦ Feel (dry, wet, slippery, stretchy) Cervico Mucus Condoms are commonly made of thin sheaths of rubber (latex) or vinyl. They differ in, color, lubrication, thickness, texture and addition of spermicide. Prevent sperm from gaining access to female reproductive tract. Prevent microorganisms (STIs) passing from one partner to other. BENEFITS No systemic side effects Widely available No prescription or medical assessment necessary Only FP method that provides protection against STIs LIMITATIONS Effectiveness depends on willingness to follow instructions User-dependent (require continued motivation and use with each act of intercourse) Containing both estrogen and progestin (COCs) Prevents the release of the ovum or egg from ovaries Highly effective when taken daily (0.1 to 1) pregnancies per 100 women during the first year of use) Client can stop use Fertility returns soon after stopping Decrease menstrual flow (lighter, shorter periods) Decrease menstrual cramps Protect against ovarian and endometrial cancer Some nausea, dizziness, mild breast tenderness, headaches or spotting may occur Effectiveness may be lowered when certain drugs are taken barbiturates, carbamazetine, phenytoin and rifampicin Rare serious side effects possible Resupply must be readily and easily available Do not protect against STIs (e.g., HBV, HIV/AIDS) Women: ◦ Of any reproductive age or parity who want highly effective protection against pregnancy (within first 5 days of the menstrual cycle or any time if the client is not pregnant) ◦ Who are breastfeeding (6 months or more postpartum) ◦ Who are postpartum and are not breastfeeding (begin after third week) ◦ Who are post abortion (start immediately or within 7 days) ◦ With severe menstrual cramping or with irregular menses ◦ In need of emergency contraception Contains only progestin (single hormone) Mechanism of action ◦ Inhabits ovulation ◦ Thickness cervical mucous Used less often in Pakistan than COCs Contains both estrogen and progesterone Mechanism of action: preventing ovulation Given every 1 month Very effective at < 1 pregnancy / 100 women Health benefits and risk similar to COC Combined injectable contraceptive Only progestin: ◦ DMPA ◦ NET-EN Mechanism of action: preventing ovulation / thickness cervical mucous Given ◦ DMPA – every 3 months ◦ mNet-EN - every 2 months Very effective at < 1 pregnancy/100 women Progestin injectable contraceptive Very effective Reversible Do not affect breastfeeding Few side effects Protect against endometrial cancer and fibroids Return to health clinic for an injection every 3 months (DMPA) or every 2 months (NET-EN) Changes in menstrual bleeding patterns are common If using DMPA, return of fertility is temporarily delayed, but does not decrease fertility in the long term If using DMPA, 50% of women will stop having any bleeding by end of first year of use PICs do not provide protection against STIs, (e.g., HBV, HIV/AIDS). 1) 2) EC should be considered if unprotected intercourse has occurred, if there has been failure of a barrier method for example a burst condom or if hormonal contraception has been forgotten. Hormonal emergency contraception: single dose levonorgestrel 1.5mg within 72hours of unprotected intercourse IUD for emergency contraception: upto 5days of unprotected intercourse. Intrauterine Contraceptive Devices (IUCDs) Copper containing IUCD Hormone releasing intra uterine system (Levonorgestr el) Copper T 380 A Mirena Multiload Cu 375 LNG - IUCD Types of IUCDs Prevents Fertilization by: Changing endometrial lining Interfering with ability of sperm to pass through uterine cavity Highly effective and economical Does not interfere with intercourse Long lasting (Multiload up to 5 years and CuT up to 12 years) Quick return of fertility after removal no systemic effects Minor voluntary surgical procedure for permanently terminating fertility in men (vasectomy) and women (mini-laparotomy and laparoscopy) Vasectomy (no-scalpel or incisional): ◦ By blocking the vas deferens, sperm are no longer present in the ejaculate Minilaparotomy or laparoscopy: ◦ By blocking the fallopian tube (tying the cutting, rings, clips or electrocautery) ovum is prevented from meeting with sperm BENEFITS ◦ Highly effective, Permanent ◦ Simple surgery usually performed under local anesthesia ◦ No change in sexual functin LIMITATIONS ◦ Must be considered permanent (not reversible) ◦ Client may regret later ◦ Short-term discomfort/pain following procedure