9-Reproductive Health
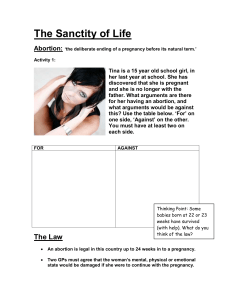
advertisement

Reproductive Health Ch 46, 47 Nursing Role in Women’s Health • • • • Health promotion Illness prevention Provide support & counseling Encourage women in their health goals and behaviors – personal hygiene, detecting & preventing diseases (STDs), diet & exercises, sexuality issuesmenopause, contraception, preconception, pre/postnatal care, stress management & well-being, healthy lifestyles, & avoiding risky behaviors Nursing Role in Women’s Health • Nurses need to model that lifestyle for patients • Recommend & promote regular examinations • Non-judgmental, understanding & sensitive • Screen for/and recognize s/sx. abuse • Recognize cultural differences & beliefs • Respect sexual orientation External genitals of the female Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Female Reproductive System oviduct oviduct ovary uterus urinary bladder pubic symphysis fimbriae ovary cervix rectum urethra vagina anus uterus vagina Function of Female Reproductive System • Ovulation – ova begins to mature & enlarge until discharged – Migrates toward & enters oviduct where possible fertilization may take place • Mentrual Cycle – involves production of estrogen & progesterone • Menopausal period – end of woman’s reproductive capacity. • Early menopause – surgical removal of ovaries, chemotherapy, radiations, unknown etiology Assessment • Health Hx. – past illnesses, STDs, treatments, hx sexual/physical abuse, • Sexual Hx. – PE findings, lab results • Female genital mutilation – – Cutting, partial/total removal of external genitalia – Cultural passage to womanhood: Africa, Middle East. Crime in the U.S. – Type I, II, III, IV p 1620 Assessment • Domestic violence – Physical: for child, elderly; men & women – Emotional degradation, coercive control, threats, intimidation. – Sexual assaults • The need to maintain control of a partner is rooted in sex role inequality. • Sensitive care is required if a woman states that she is being hurt. • Report & provide safety for pt. (p.1621) Physical Assessment • Periodic examination/ pelvic & breast • Routine cancer screening • Positioning: supine lithotomy, upright lithotomy vs. Sims position (left side) • Proper equipment • Inspection : lesions of the labia majora/minora (venereal warts, melanoma lesions) trauma to the vaginal wall, cystocele, rectocele, presence of a hymen Assessment • Women with disabilities experience increase risk for abuse – Inquire about barriers to health care – Any healthcare limitations – Cognitive or developmental changes affecting understanding • Gerontology considerations – Facing health disparities or end-of-life issues Physical Assessment Speculum Examination: • Cervix – 2-3 cm, smooth vs. laceration • Malignant changes • cysts, polyps • Discoloration • Cauliflower-like growth (cancer) • Vaginal discharge Inspection of the Cervix Diagnostic Testing • PAP Smear – cytology for detecting cervical cancer – Atypical cells: Human papillomavirus (HPV) • Colposocpy – visual examination with a portable microscope • Cervical biopsy – analysis of cervical tissue • Cryotherapy/laser therapy – freezing cervical tissue with nitrous oxide • Cone Bx Loop Electrosurgical Excision Procedure (LEEP) – surgical procedure using laser beam Diagnostic Testing • Endometrial Aspiration Bx. – allows for detection of cellular changes in the endometrium • Dilation & Curettage (D&C) – surgery; dilation if cervical canal and scraping of endometrial/endocervical tissue for cytology • Endoscopic laparoscopy – visualization of the pelvic structures Diagnostic Testing • Hysteroscopy – visualization of all the parts of the uterine cavity • Hysterosalpingography or Uterotubography – x-ray of uterus & fallopian tubes. • Computed Tomography (CT) – transverse radiographic images • Ultrasonography – ultra sound images. • Magnetic Resonance Images (MRI) – definitive images using magnetic waves Management of Physiologic Processes • Menstruation – 28-day cycle during reproductive years – Understand cutural beliefs, customs & values, psycological consideration, NSAID • Perimenopause – 1st sign of menopause: hot flashes, vaginal dryness, irregular menses. – Consider issues in sexuality, fertility, STD,oral contraceptives, breast cancer, Management of Physiologic Processes • Menopause – permanent physiologic cessation of menses • Associated with decrease ovarian function, some breast & genital organ atrophy • Irregular menses, breast tenderness, mood changes, hot/warm flashes, noc sweats, sleep disturbances, gradual thinning of pubic hair, shrinkage, fatigue, forgetfulness • Be sensitive to all possible side effects • Tx – hormone therapy Management of Menstrual Disorders • PMS - prementstrual syndrome: • Irritability, fatigue, bloating, edema, HA, depression, low back pain, painful breast, mood swings • Tx symptoms, promote exercise, avoid caffeine & high-fat diets • Vit. B, E, magnesium, oil of primrose are used but show no evidence of effectiveness • Selective serotonin reuptake inhibitors (Prozac, Sarafem, Fluoxetime, Ibuprofen, Naproxenk Anaprox, diuretics, antianxiety, calcium supplements Management of Menstrual Disorders Nursing management: • Establish nurse/pt rapport, for good health history • Nutrition history • Minimize side effects, stress-coping strategies • Pt educ: avoid caffeine, alcohol, eating diet low in essential nutrients. Teach how to record timing & intensity of symptoms Menstrual Disorders Dysmenorrhea: painful menstruation, severe crampings • Tx: relieve discomfort, A.S.A. NSAIDs, low level local heat – Contraindicated with peptic ulcers Amenorrhea – absence of menstrual cycle • Allow pt to express concerns, PE, medical hx., stress level, pregnancy, eating disorders, anorexia & bulimia Menstrual Disorders • Menorrhagie – excessive menstruation; profuse, prolong flow during regular periods • Related to endocrine distrubances, inflammatory disturbances, uterine tumors • Can result in anemia; need to see MD – Count # pads, & saturation (absorbency) Menstrual Disorders • Metrorrhagie – heavy uterine bleeding between periods; irregular – May signal cancer, benign tumors of the uterus – Health hx., taking oral contraceptives or HR? • Hypomenorrhea – scanty flow • Oligomenrrhea – reduced frequency of periods Contraception • Abstinenece – practice celibacy; only effective method • Sterilization – Bilateral tubal ligation: laparoscopy procedure • Fellopian tubes are coagulated, sutured, or ligated with bands/clips. • Transcervical tubal occlusion – Vasectomy – excision of the vas deferens Contraception • More than half of pregnancies in the U.S. are unintended • Nurses can assist in providing information and support • Family planning resources • Listen, educate and take time to answer questions • Be unbiased and nonjudgmental • Understand the risks & benefits Contraception • Hormonal – use of estrogens & progestins by women. • Block ovarian stimulation, prevent release of FSH from the anterior pituitary gland. • Benefits: reduce incidence of benign breast disease, uterine & ovarian cancers, anemia, pelvic infections; Improves acne. • Risks: DVT, breast soreness, HA, nausea, leg cramps ** Inform pts that hormonal contraception protects against pregnancy but not from STD of HIV Contraception • Intrauterine device (IUD) – a plastic, t-shaped device inserted into the uterine cavity to prevent pregnancy. • Causes local inflammation, which is toxic to sperm & blastocysts; therefore prevents fertilization • May cause excessive bleeding, cramps, backaches, slight risk of tubal pregnancy, perforation of cervix and uterus is rare Contraception • • • • • • • • • Mechanical barriers – diaphragm Cervical cap Contraceptive spong Female condom (p1645) Male condom Spermicides Coitus interruptus (withdrawal) Rhythm & natural method – “safe period” Emergency contraception – morning after pill Contraception • Abortion – • Spontaneous abortion • Habitual (recurrent) abortion – After 2 consecutive abortion, pt is referred to genetic counseling and testing • Elective abortion – voluntary – Pt education & counseling on choices – Explore pts fears, feelings and options – Review use of birth controls methods Nursing management • For spontaneous abortion - provide bed rest, sexual abstinence, no straining on defecation • Allow expression of feelings: listen • Pt education: available forms of contraception, community resources • Counseling • Pelvic exam, lab studies, RhoGAM, STD screening Infertility • The couple’s inability to achieve pregnancy after 1 yr. of unprotected intercourse. • Ovarian/ovulation factors • Tubal factors • Uterine factors • Semen & other male factors Artificial Insemination • Deposit of semen into the female genital tract by artificial means – – – – Sperm cannot penetrate the cervical canal Donor or partner/husband semen is frozen Written consent Safeguards set in place for legal, ethical, emotional & religious issues • Must meet certain condition: the women should have no genital abnormalities, require patent fallopian tubes, available ovum. • Viable sperm: normal shape, amount, motility and endurance Ectopic Pregnancy • Decreasing in rate, but remains the leading cause of pregnancy related dealth in 1st trimester • Acute condition – require surgery • Relieve acute pain • Monitor potential complications– prevent hemorrhage, shock. • Provide emotional support