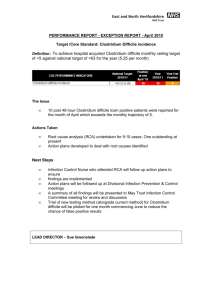
Standards of Care “CARES”
advertisement

STUDENT ORIENTATION HANDBOOK Fort Loudoun Medical Center 550 Fort Loudoun Medical Center Drive Lenoir City, TN 37772 865-271-6000 1 Table of Contents • Welcome Letter • Purpose, Vision, Values • Organizational Structure • Phone List: Frequently Called Numbers • Patient Care Philosophy • Ethics Committee • Behavior Expectations • Care of Equipment & Supplies • Chaplain Services • Infection Control • Risk Management • National Safety Standards • Abandoned Baby-Surrender of Infant • Suicide Precautions • Safety & Security: Emergency Response / System Failure CLINICAL STAFF INFORMATION • Nursing Standards of Care • Abuse • Restraints FORMS & REQUIRED DOCUMENTATION • Receipt of Handbook Signature Form • Post-Test for Infection Control • Post-Test for Safety/Security • Post-Test for Clinical Content 2 WELCOME !!!!! …..to Fort Loudoun Medical Center. We are glad you’re here. This orientation handbook was designed to help familiarize you with our facility policies. Please take time to look through this information. At the end of this booklet, you will find a test for Infection Control and Safety/Security. All students are required to complete these tests. The last section of this handbook is for clinical staff and students only. All clinical staff and students are required to complete the above mentioned tests and the postclinical test. You may use the information enclosed to help you obtain the answers. The completed tests and signed confidentiality agreement are due before you begin your rotation. Please send them to your clinical instructor, who will then forward to the Education Department. If you have any questions, please feel free to contact us @ 271-6508. Again, welcome to Fort Loudoun! 3 Our Purpose We serve the community by improving the quality of life through better health. Our Vision Through its people Covenant Health will be recognized as the premier health services system in Tennessee Our Values Working together in service to God, our values are: Integrity Quality Service Caring Developing People Using Resources Wisely 4 Human Resources Department Ethel Owens 531-5066 We want your employment and/or clinical rotation here to be satisfactory for both you and your manager. We are here to help you with any concerns or problems. Comment boxes are provided for all employees, visitors, or patients to provide feedback on our organization and the services we provide. Please complete the suggestion/comment card and drop in the comment box. 5 Most Frequently Called Numbers: FLMC Main Line 271-6000 Administration 271-6500 Benefits Info Line 531-5469 Cardiac Rehab 271-6030 Cardiopulmonary 271-6284 Case Manager/Patient Representative 271-6509 CCU 271-6290 Chaplain Notify Nursing Supervisor 417-4263 Dietician 271-6308 Dining on Call 271-6300 Engineering 271-6445 Employee Assistance Program 531-4500 Education / Employee Health 271-6508 Environmental Services 271-6440 Help Desk 374-4900 HIM (Medical Records) 271-6010 Human Resources 271-6040 Imaging 271-6045 Infection Control 271-6509 Laboratory 271-6050 Materials Management 271-6400 Med-Surg 271-6455 Pharmacy 271-6370 Quality / Risk 271-6507 Surgery Waiting 271-6085 While on campus, you must dial the number 5 and the last 4 digits of the number. HR cannot transfer personal calls except on an emergency basis. If you use the main hospital number as your work number, be sure to indicate your department. The hospital operator may not have this information. 6 PATIENT CARE PHILOSOPHY Every patient who enters a Covenant Health facility is to be treated with courtesy, compassion, respect, and dignity. As an employee or student, you have accepted the high and special challenge of providing advanced technological care while maintaining a personal and close awareness of the individual human needs of our patients. In any activity conducted by, for, or in the organization affecting care and treatment of patients, there will be no separation, discrimination or other distinction on the basis of race, color, disability, or national origin. All cultural diversity is acknowledged and incorporated into the patient plan of care. In working with the sick and injured, it is important to remember that you are dealing with persons in exceptional circumstances. You will discover that many patients have fears and resentments that may manifest themselves as irritability, lack of cooperation and apprehension. Courtesy, kindness, and above all, sincere understanding are important steps in overcoming these problems. Always remember that what is routine for you may be a great emergency in the mind of the patient and his/her family. Your thoughtful consideration will often be remembered long after the medical services performed have been forgotten. STAFF RIGHTS Requests by a staff member not to participate in any aspect of patient care where there is perceived conflict with the staff member’s cultural values or religious beliefs will be addressed in the following manner: 1.The Ethics Committee is available to employees as a forum and source of ideas for resolution of ethical conflict. 2.Employees may transfer to a position in another department, if available. 3.If the ethical conflict occurs when the employee is on duty, and the patient’s need for care or treatment is imminent, the staff on duty should decide who will care for the patient. If no decision can be reached, the staff member in charge should refer the issue to the manager, Director, Administrative Supervisor, or Administrator On-call to render a decision to ensure that the patient receives7 appropriate care. These guidelines provide a mechanism to address the concerns of staff while ensuring that a patient’s care will not be negatively affected. ETHICS COMMITTEE Covenant Health is committed to the care of people in a manner that ensures patient and family dignity, privacy, and respect. Affirming the rights of the patient to participate in the planning and decisionmaking processes affecting his or her treatment is facilitated through the provision of a multidisciplinary Ethics Committee at each facility. Access to the Ethics Committee at Fort Loudoun regarding any issue is available through contacting Quality Support Services, Administration, or the Nursing Supervisor. The objective of the Ethics Committee is to provide education for its members, the staff, and the patient/family; to be involved in the development of policy and procedure issues concerned with ethical issues; and to be available for case reviews. Any individual, be it staff, patient, family, or the general public, may request a review by the Ethics Committee. 8 CAFETERIA The cafeteria is open Monday through Friday for breakfast and lunch. Breakfast 7:30am-9:00am Lunch 11:00am-1:30pm LOST & FOUND •All property found on the FLMC campus must be turned over to Security, who shall serve as a central clearing point for all personal articles, property, or other valuables that are found. 9 BEHAVIOR EXPECTATIONS DRESS, APPEARANCE AND HYGIENE: This policy is intended to provide guidelines regarding appropriate appearance standards at Covenant Health. It cannot address every potential item of clothing or accessory; therefore, Managers are expected to apply good judgment in maintaining professional and appropriate appearance of their employees. The image we portray through our dress and appearance is an important reflection of our professionalism and commitment to quality. Therefore, our employees should meet the following guidelines regardless of where they work: Clothing and Fit All clothing, regardless of whether it is a uniform or other dress, should be clean, fit properly, in good repair and pressed or ironed as needed. Any article of clothing that portrays a printed message, which could be offensive to the general public, shall not be worn. Denim is not appropriate in the workplace, although departments may occasionally allow denim attire when the work being performed warrants it. Uniforms Students should adhere to the school uniform policy for clinical rotations, except in areas where facility provided scrubs are required, such as Surgery. Tops/Blouses Tops and blouses should not have a revealing neckline or midriff. Sweatshirts, tank tops, and shirts with printed messages are not permissible. 10 Pants Pants may be worn if appropriate; however, the following styles should not be worn: overalls, warm-up or sweat pants, clamdiggers, pedal pushers, tight stirrup pants, or leggings. Capri pants may be worn by staff in the nonclinical departments; however, they must cover ¾ of the leg or reach the bottom of the calf. Skirts, Dresses, and Shorts Skirts and dresses should be of appropriate length. Culottes, city shorts, and skorts are not permitted. Sundresses and tank tops are not permitted. Shoes Shoes must be appropriate to the dress and job for a given department. Clinical: white or black leather or canvas athletic shoes. They are to be clean and polished. Colored athletic shoes are not permitted. Athletic shoes may have a conservative amount of color. Colored shoestrings must not be worn. Non-clinical: Causal sandals are not to be worn; however dressy open toe, open back, or sling back shoes are acceptable. 11 Undergarments Appropriate undergarments (including hosiery/socks) will be worn to present a neat and professional appearance. Hair Employees and students must keep their hair clean and in an orderly fashion that does not present a safety hazard. Color, style, and length should be appropriate; mustaches, sideburns and beards are to be neatly trimmed. For employees who are required for safety reasons to wear a respirator, beards may not be worn since they would interfere with the proper fit of the respirator. Hats Hats may be worn only as part of an approved overall work uniform. Jewelry Jewelry may be worn but should not depict an insignia offensive to the general public. Excessive or dangling jewelry may be a safety hazard to the patient or employee. Male employees and students may not wear earrings while on duty. Certain departments may have a “no jewelry” policy. Females may wear a maximum of two earrings per ear. No tongue piercing or any visible body piercing is permissible. Makeup and Fragrances Make-up and personal body fragrances, including perfume and aftershave may be worn but should not be overly strong. People who are ill may be especially sensitive to odors, which may cause nausea or allergic reactions. Certain departments may have a “no fragrance” policy due to patient concerns. 12 Fingernails Non-clinical: All employees and students not having direct patient care should keep fingernails clean and neatly trimmed. Artificial nails may be worn but must be properly maintained. If nail polish is worn, it must be free of cracks, chips, and peeling. Clinical: All employees and students who assist in patient care or provide services that come in contact with patients will maintain short, clean and well manicured nails. Nails should be short enough to allow the individual to thoroughly clean underneath them, not cause glove tears, and not cause injury to patients when moving or positioning patients. Artificial nails will not be worn. If nail polish is worn, it must be free of cracks, chips, or peeling. Artificial nails are defined as substances or devices applied to the natural nail to augment or enhance the nails. They include, but are not limited to, bonding, tips, wrapping, and tapes. Identification Badges All employees and students are required to wear an identification badge (name and picture facing out) at all times while on duty enabling them to be readily identified by patients, visitors, physicians, and other employees. Pins of a professional nature may be worn on the badge as long as the pin does not cover or damage the printing, photo, or bar code on the badge. No tape or stickers should be placed on the badge. 13 CARE OF EQUIPMENT AND SUPPLIES Medical equipment is one of the most important resources we use in treating patients. It is vital that you be alert to any malfunction or disrepair of any equipment and that you report it to your Supervisor or Manager immediately. Remove the malfunctioning equipment from service and tag apporpriately for repair. Do not attempt to use any equipment for which you have not been properly trained. Always ask for assistance with unfamiliar equipment. Supplies are expensive, and you should try to prevent waste and spoilage. If you should find that you could not satisfactorily complete your duties because of inadequate supplies, you should report the shortage immediately to your Supervisor or Manager. Cafeteria items such as trays, plates and silverware are not to be removed from the cafeteria. If you wish to carry out food, ask for and use paper plates and plastic utensils. If you should find cafeteria utensils outside the cafeteria, please return them to the Food Services Department. As part of the organization’s involvement in and commitment to the national cost containment program, we ask your help in treating all equipment and supplies with extreme care. Losses in these areas mean increased costs for the organization, which result in increased costs for our patients. 14 CHAPLAIN SERVICES The Chaplains are here for YOU, our patients, and their loved ones. • Chaplain services are provided by Volunteer Chaplains who are on call on a rotating basis. • The Chaplains are here to serve our patients, their loved ones, and our employees. If you have questions or would like to speak with a Chaplain, feel free page the nursing supervisor. The on-call Chaplain will be contacted for you. • YOU are our most important asset…the Chaplains would like to stress the importance of employees taking care of themselves as well as their patients. You are welcome to visit the chapel at any time to enjoy a quiet moment in a peaceful setting. 15 INFECTION CONTROL FLMC has an Infection Control / Exposure Control Plan to prevent the transmission of blood borne pathogens such as: HIV, HBV, HCV, and other potentially infectious agents by: –Reducing reasonably anticipated exposure to blood and other potentially infectious materials –Establishing engineering and work practice controls –Providing appropriate employee training and follow-up, and monitoring of work practices HANDWASHING IS THE SINGLE-MOST EFFECTIVE WAY TO PREVENT THE SPREAD OF DISEASE / INFECTION. IT IS OUR DUTY TO PROTECT THE PATIENTS!!! The following pages will provide detailed information on disease-specific pathogens. –Standard Precautions –Hepatitis B –Hepatitis C –HIV –C Diff –VRE –MRSA –Exposure Policy 16 ISOLATION IMPLEMENTATION Type of Isolation Infections Isolated What to do for each type of isolation MAXIMUM CONTACT MRSA, VRE, C. diff, major draining wounds, Chicken Pox, Shingles, multi-drug resistant gram negative bacteria PPE cart/cabinet stocked Hand wash with soap/water or hand sanitizer Glove before entry into room Gown if potential contact with contaminated surfaces Alert other departments of patient’s isolation status Dedicated equipment (BP cuff, stethoscope, thermometer, etc) AFB (Acid-fast bacilli) Pulmonary Tuberculosis (TB) *(Severe Acute Respiratory Syndrome (SARS) –requires negative air room) *(Smallpox –requires negative air room) *Contact Inf Control/Health Dept Place patient in negative air pressure room (Med/Surg, CCU, ED, and Recovery) Employee fitted for the particulate respirator Wear respirator to enter room Keep door closed at all times (even when the patient is temporarily out of the room) Negative Air Pressure turned on Patient wears a surgical mask (if possible) to leave room Visitors instructed to wear the particulate respirator One hour after patient discharge for unprotected entry into room Chicken Pox, Shingles – also requires CONTACT isolation Keep door closed at all times Only immune-competent staff should be assigned to care for the patient Negative air pressure room recommended if extensive draining lesions and in mouth or nares Can be airborne transmitted if lesions are in nares and mouth or from handling contaminated linen Contact transmission from hands/items contaminated with drainage from lesions DROPLET Flu, Pertussis (whooping cough), Neisseria meningitidis, Mycoplasma pneumonia, Parvovirus B19, Haemophilus Influenza meningitidis, Rubella, Adenovirus, pharyngeal Diphtheria, mumps, Group A strep Wear surgical mask to enter room Eye protection as required Patient wears surgical mask, if possible, to leave room PROTECTIVE Patients with WBC less than 1,000 Cancer patient receiving chemo Organ transplant patient receiving immunosuppressive steroids Other immune conditions that physicians feel need protective isolation All persons must wash their hands before entering the room. No fresh fruits or plants in the room (no decorative leafy garnish on the food tray) Employees with respiratory infections, fevers, draining wounds, herpetic lesions, or other potentially communicable conditions may not enter the patient’s room. All equipment that will come into contact with the patient must be disinfected with alcohol prior to and after use. Remove all soiled linen ASAP; do not keep hamper in the room Do not remove ice pitcher from the room. Carry the ice to the room in a closed paper or plastic bag. Restrict visitors to immediate family; Restrict persons with known infection. Patient wears surgical mask upon leaving the room. Implementation Checklist 1)Stock isolation cart/cabinet 2)Place isolation sign on door 3)Place isolation sticker on chart 4)Make sure alcohol hand sanitizer dispenser has solution 1)Be sure to alert other departments of patient’s status 2)Appropriate hand hygiene 3)Explain isolation to family/patient Additional information, fact sheets, etc available from infection 17 control @ 271-6509 AIRBORNE / CONTACT WHAT YOU SHOULD KNOW ABOUT HEPATITIS B WHAT IS HEPATITIS B? •Virus that causes inflammation of the liver—one of your body’s most vital organs •Found in blood HOW IS IT SPREAD? Mainly through blood •Infected needles and sharps •Shared personal care items •Unprotected sex •Membranous exposure (eyes, nose, mouth) •Bites and wounds •Perinatal transmission HEPATITIS B CAN RESULT IN: •No symptoms •Mild illness •Acute (severe) illness •Chronic infection •Liver damage, such as cirrhosis •Liver Cancer •Death due to liver failure WHAT ARE THE SYMPTOMS? May appear 1-9 months later •Asymptomatic •Flu-like (vomiting, nausea, diarrhea, sore muscles and joints, mild fever, headaches) •Fatigue •Stomach pain •Loss of appetite/weight •Jaundice •Dark urine HOW DO WE TEST FOR HEPATITIS B? •Physical exam to check if liver is swollen •Blood test for liver profile •Liver biopsy HOW DO WE TREAT HEPATITIS B? •No treatment PREVENTION Vaccine is very effective •Health care workers: Use standard precaution, get vaccinated, exposure management •HBV + individuals: Protected sex, don’t donate blood or organs, don’t share personal care items 18 WHAT YOU SHOULD KNOW ABOUT HEPATITIS C WHAT IS IT? •A virus that can cause serious liver disease •Found in blood HOW IS IT SPREAD? Mainly through infected blood •Infected needles (IV drug, body piercing, and tattoo needles) •Shared personal care items (razors and toothbrushes) •Unprotected sex (less common cause) •Blood transfusion before 1992 HOW DOES IT AFFECT YOUR HEALTH? Damages your liver •Approximately 85% develop chronic disease found 20-30 years after initial infection •Cirrhosis (30-40%) •Cancer (2-4%) •Liver failure •Problems with your immune system WHAT ARE THE SYMPTOMS? Usually acute infection is without symptoms •Flu-like (fatigue, nausea, vomiting, diarrhea, sore muscles and joints, mild fever, headaches) •Loss of appetite •Weight loss •Right upper abdomen tenderness •Jaundice •Abdominal swelling •Itching •Dark urine HOW DO WE TEST FOR HEPATITITS C? •Physical exam to check if your liver is swollen •Blood test for liver profile •Liver biopsy HOW DO WE TREAT HEPATITIS C? •Avoid alcohol and non-prescriptive medications like acetaminophen •Eat a well-balanced diet •Get adequate rest •Exercise •Take medication as prescribed by your doctor PREVENTION STEPS No vaccine or medication can prevent the spread of Hepatitis C Health care workers: Use standard precaution practices if there is risk of exposure Follow hospital policy for exposure management If you are Hepatitis C positive: Use condoms during sex 19 Don’t donate blood products, body tissue, organs Don’t share needles, razors, toothbrushes, manicure tools, or other personal items WHAT YOU SHOULD KNOW ABOUT HIV WHAT IS IT? Virus that enters bloodstream, invades immune system, overwhelms immune system Causes AIDS (auto-immune disease syndrome) HOW IS IT SPREAD? Infected needles and sharps Shared personal care items Unprotected sex Membranous exposure (eyes, nose, mouth) Broken skin exposure Perinatal transmission HOW DOES IT AFFECT YOUR HEALTH? Stages of the disease May not show symptoms for years Swollen glands, lesser diseases Inability to fight off life-threatening diseases WHAT ARE THE SYMPTOMS? Weakness Fever Sore throat Nausea Diarrhea White coating on tongue Weight loss Swollen lymph glands HOW DO WE TEST FOR HIV? Antibody test Western Blot HOW DO WE TREAT HIV? No vaccine or cure Anti-retroviral Protease inhibitor PREVENTION Health care workers: Use standard precautions, exposure management HIV + individuals: Protected sex, don’t donate blood or organs, don’t share personal care items 20 Clostridium difficile (C. difficile) Fact Sheet What is C. difficile? Anaerobic gram-positive spore-forming bacteria producing toxins that cause disease such as C. difficileassociated diarrhea (CDAD). What causes C. difficile? Diarrhea may occur as a result of antibiotic use for various reasons but is most severe if caused by C. difficile. Types of diarrhea-associated C. difficile are a) Nonspecific diarrhea which is self-limited, and relatively mild b) CDAD is an infectious diarrhea which is almost always acquired by patients who have taken antibiotics recently (usually within 2 months). The mechanism by which antibiotics induce C. difficile disease is not well understood and c) Pseudomembranous colitis (PMC) is a more severe form of CDAD characterized by the presence of pseudomembranes that are yellow, white, or gray neutrophilic mucosal plaques in the colon. How is C. difficile transmitted? The organism is most often transmitted via the hands of health care personnel who have had contact with contaminated feces or contaminated environmental surfaces. Infection results from ingestion of C. difficile spores, which survive the acid environment of the stomach, convert to the vegetative forms in the colon, and produce toxins that result in the clinical symptoms. Commodes, baby baths, and electronic thermometer handles are among the environmental sites implicated in the transmission of C. difficile. What prevention and control measures can be taken? • • • • • • • • Contact Isolation precautions. Isolation cart outside patient’s room. Alcohol hand sanitizers will not kill C. difficile spores, therefore washing with soap and running water is important to physically remove the kill-resistant spores. Alcohol hand sanitizers are effective for the vegetative forms of C. difficile but not C. difficile spores. Wear gloves before entering the isolation room. Gowns should be worn to prevent contamination to your clothes. Dedicate equipment for that patient’s use only. Adequate disinfection of medical devices is important (especially items likely to be contaminated with feces such as thermometers). Non-critical care items such as blood pressure cuffs and stethoscopes should be bagged in clear plastic and sent to Sterile Processing for gas sterilization. Reusable critical care equipment should be disinfected and steam or gas sterilized based on the manufacturer’s recommendation. Wheelchairs, intravenous poles, and stretchers that are contaminated by infected patient should be cleaned by vigorously wiping surfaces with an approved disinfectant/cleaner. Reusable bedpans should be cleaned daily with disinfectant and terminally in the cart washer. The environment of the room may be highly contaminated with C. difficile spores depending on the severity of the diarrhea. Thoroughly clean and disinfect the isolation room. A sporicidal agent is preferred. Areas for attention include toilets, reusable bedpans, furniture, floors (in the bathrooms, patients’ rooms, and soiled utility room), sinks, bedrails, and telephones. Mops and water are changed for each isolation room. Special cleaning attention should be given to areas around the toilet. Walls should be spot cleaned for all visible soiled areas. Used linen should be bagged in the patient’s room. Minimizing or preventing anitmicrobial use in patients such as restricting Clindamycin use and controlled use of extended-spectrum cephalosporins. How is C. difficile disease treated? 21 The first line of treatment is to discontinue the causative antimicrobials or select agents such as metronidazole, vancomycin, aminoglycosides, or possibly fluroquinolones, which are less likely to cause CDAD. Vancomycin-Resistant Enterococcus (VRE) What is Enterococcus? Enterococcus is gram-positive bacteria normally found in the gastrointestinal tract and female genital tract. It can cause infection of the following: urinary tract, abscesses and wounds, decubitus ulcers, diabetic foot ulcers, bloodstream infections, and endocarditis. Vancomycin is a drug that is frequently used to treat many types of infections. If Enterococcus is resistant to vancomycin it is referred to as VRE (vancomycin-resistant Enterococcus). Frequently, VRE is also resistant to many of the other drugs used to treat Enterococcal infection. Therefore, infections caused by VRE can be life threatening. How Does VRE Infection Occur? Infection often results from the patient’s endogenous carriage (residing on or in the patient’s body). The bacteria leave the area of colonization such as the GI tract or GU tract, enters a site, multiplies and causes an infection (i.e., wounds or migration along a catheter). VRE can also be transmitted from the contaminated hands of HCW’s (with or without gloves) or contaminated items or contaminated environment to a patient. How Do You Prevent Transmission of VRE? Infections caused by VRE require enhanced precautions beyond Standard Precautions in order to prevent transmission to a distant site on the colonized patient or transmission to another patient. Practicing good patient care and maintaining required aseptic and sterile technique is important. Reasons for enhanced precautions include the potentially serious outcomes of infection, the ease by which VRE contaminates the environment and its ability to live for days on the environment, objects, and fabrics. Therefore these patients are placed in Contact Isolation. How Do You Implement Contact Isolation? After you are alerted to the patient’s VRE status you will do the following: •Obtain and place a contact isolation cart outside the patient’s door. The cart will be stocked with gloves, gowns, disinfectant, and thermometer. •Dedicate devices such as blood pressure cuffs and stethoscopes to prevent transmitting Enterococcus to yourself and others. If reasons necessitate the use of such devices on another patient, you must clean and disinfect the device with an appropriate cleaner/disinfectant such wiping with 70% isopropyl alcohol or other FDA registered product. •Post the contact isolation sign on the patient’s door or door frame so that it is noticeable to people who will be entering the room. •Place the contact isolation label on the front of the chart so that those who look at the chart can easily see it. •Handwashing must be performed before and especially after leaving the room. 10-15 seconds of lathering with soap and water. 15-20 seconds of rubbing with the alcohol hand sanitizer. Be sure to also focus under and around the fingernails and jewelry if worn. •Gloves must be worn in order to enter the room. Gowns must be worn if you anticipate contact with the patient or the environment. •Alert other departments if the patient is to be transferred for diagnostic testing (i.e., surgery and radiology) or if transferred to a different unit. •Whenever possible, communicate the VRE isolation to the physician, other clinicians, dietary and housekeeping. Encourage and educate others to appropriately follow isolation precautions. Family and Patient Fact Sheet for VRE If the family requests information about VRE or if you determine that such information would be of benefit 22 to the family, contact Infection Control at 271-6509. Methicillin-resistant Staphylococcus aureus (MRSA) What is Staphylococcus aureus? Staphylococcus aureus is Gram-positive bacteria frequently found on the skin, nares, groin, and GI system. It may cause infection in the sputum, blood, surgical wounds, burn wounds, decubitus ulcers, perineum, rectum, tracheostomy, or grastrostomy sites. Methicillin is a drug frequently used to treat Staphylococcus aureus. If Staphylococcus aureus becomes resistant to Methicillin it is called Methicillinresistant Staphylococcus aureus (MRSA). MRSA strains are frequently resistant to other classes of drugs, therefore MRSA is very serious or may even be life threatening to your patient. How Does Infection Occur? MRSA is usually transmitted from patient to patient via hand carriage of Health Care Workers in the hospital setting. Also, patients may be colonized (carries it somewhere on their body). Colonized patients may become infected with their own bacteria, such as MRSA on the patient’s skin migrating into a Foley catheter. How Do You Prevent Transmission of MRSA? Infections caused by MRSA require enhanced precautions beyond Standard Precautions in order to prevent transmission to a distant site on the colonized patient or transmission to another patient. Practicing good patient care and maintaining required aseptic and sterile technique is important. Reasons for enhanced precautions include the potentially serious outcomes of infection, the ease by which MRSA contaminates the environment and its ability to live for days on the environment, objects, and fabrics. Therefore these patients are placed in Contact Isolation. How Do You Implement Contact Isolation? After you are alerted to the patient’s MRSA status you will do the following: • Place a contact isolation cart outside the patient’s door. The cart will be stocked with gloves, gowns disinfectant, and thermometer. • Dedicate devices such as blood pressure cuffs and stethoscopes to prevent transmitting Staph aureus to you and others. If reasons necessitate the use of such devices on another patient, you must clean and disinfect the device with an appropriate cleaner/disinfectant such wiping with 70% isopropyl alcohol or other FDA registered product. • Post the contact isolation sign on the patient’s door or door frame so that it is noticeable to people who will be entering the room. • Place the contact isolation label on the front of the chart so that those who look at the chart can easily see it. • Handwashing must be performed before and especially after leaving the room. 10-15 seconds of lathering with soap and water. 15-20 seconds of rubbing with the alcohol hand sanitizer. Be sure to also focus under and around the fingernails and jewelry if worn. • Gloves must be worn in order to enter the room. Gowns must be worn if you anticipate contact with the patient or the environment (including activities such as holding clipboard in the room, dispensing meds to the patient, etc.). • Alert other departments if the patient is to be transferred for diagnostic testing (i.e., surgery and radiology) or if transferred to a different unit so that they can take the same precautions you are expected to take with your patient. • Whenever possible, communicate the MRSA isolation to the physician, other clinicians, dietary and housekeeping. Encourage and educate others to appropriately follow isolation precautions. Family and Patient Fact Sheet for MRSA 23 If the family requests information about MRSA or if you determine that such information would be of benefit to the family, contact Infection Control at 271-6509 to obtain a copy of the patient/family fact sheet. NEEDLESTICK/BODY FLUID EXPOSURE POLICY Policy Statement Any work-related percutaneous (needlestick, laceration, bite) or permucosal (ocular, mucous membrane) exposure to blood or body fluids MUST be reported to Employee Health. CDC guidelines will be followed for assessment and treatment. Objective To control transmission of hepatitis B (HBV), hepatitis C (HCV), and HIV among health care workers. Procedure 1. WASH all exposure sites with soap and water. Eyes and mucous membranes exposures should be flooded with water. 2. Accidents must be reported immediately to the employee's supervisor or the house supervisor and an Incident Report completed. The employee will then go to Employee Health with the report. If the injury occurs during a time in which Employee Health is closed, the employee will contact the House Supervisor for evaluation and follow-up by Employee Health. 3. A tetanus booster is given per protocol, if indicated. 4. Subsequent management of the employee depends on the serological status of the source patient and the vaccination and/or serological status of the employee (see EOHS, Blood/Body Fluid Exposures Policy and FLMC Exposure Control Plan – Policy EC.SF.004). Students will be managed and treated at their request . Insurance will be billed for costs incurred. 24 RISK MANAGEMENT Fort Loudoun Medical Center has adopted an occurrence reporting mechanism to enable the hospital to carry out its responsibility for provision and continuous improvement of quality care in a safe environment. DEFINITION: A reportable occurrence can be defined as any event that is not consistent with the normal or usual operation of the hospital. Injury does not have to occur. The potential for injury and/or property damage is sufficient for an occurrence to be considered reportable. Examples: 1. Any occurrence which could or does cause patient/visitor injury or harm 2. Testing and treatment errors or delays/omissions 3. Failure to follow policy and procedure 4. Failure to follow MD orders 5. Incorrect transcription of MD orders 6. AMA discharges 7. Problems with other departments 8. Equipment which malfunctions or is damaged REPORTING RESPONSIBILITIES: Any employee who is involved in, observes, or hears about a reportable event is responsible for reporting it to his/her manager/supervisor at the time of the incident and for initiating the Systems Improvement Report. The manager/supervisor will assist in the completion of the report if necessary. A. Occurrences involving a patient will be reported immediately. If the occurrence has an extreme outcome, the Risk Manager should be notified by telephone, day or night. A Risk Manager is always on call for the Covenant System. B. In case of personal injury to a visitor or volunteer on hospital property, the Risk Manager, Nursing Director/House Supervisor should be notified immediately and a report completed. C. In case of theft, disturbance, or soliciting, Security should be notified immediately any time day or night. An officer will investigate and complete a Security Incident Report. D. In case of equipment malfunction or damage, the Engineering Department should be notified. A tag shall be filled out and attached to the piece of equipment. The piece of equipment shall be taken out of circulation. EXCEPTION: Essential equipment may be tagged and left in use as per decision of Engineering, Risk Manager, or Administrator-on-Call. 25 National Safety Goals: Improve the accuracy of patient identification: – Use at least two patient identifiers (the patient’s name and date of birth – NEVER use the patient’s room number to identify the patient) whenever taking blood samples or administering medications or blood products. Prior to the start of any surgical or invasive procedure, conduct a final verification process, such as a “timeout,” to confirm the correct patient, procedure and site, using active – not passive – communication techniques. – Improve the effectiveness of communication among caregivers: – Implement a process for taking verbal or telephone orders that require verification “readback” of the complete order by the person receiving the order. Standardize the abbreviations, acronyms and symbols used throughout the organization, including a list of abbreviations, acronyms and symbols NOT to use. Measure, assess and, if appropriate, take action to improve the timeliness of reporting, and the timeliness of receipt by the responsible licensed caregiver, of critical test results and values. Implement a standardized approach to "hand off" communications, including an opportunity to ask and respond to questions. – – – Improve the safety of using medications: – Standardize and limit the number of drug concentrations that are available in the organization. Identify and, at a minimum, annually review a list of look-alike/sound-alike drugs used in the organization, and take action to prevent errors involving the interchange of these drugs. Label all medications, medication containers (e.g., syringes, medicine cups, basins), or other solutions on and off the sterile field in perioperative and other procedural settings. – – Eliminate wrong-site, wrong-patient, wrong-procedure surgery: – Create and use a preoperative verification process, such as a checklist, to confirm that appropriate documents, (e.g., medical record, imaging studies) are available. Implement a process to mark the surgical site, and involve the patient in the marking process. – Reduce the risk of healthcare acquired infection: – – Comply with current CDC hand hygiene guidelines Manage identified cases of unanticipated death or major permanent loss of function associated with a healthcare acquired infection as a sentinel event. Accurately and completely reconcile medications across the continuum of care- - Develop a process for obtaining and documenting a complete list of the patient’s current medications upon the patient’s admission to the organization and with the involvement of the patient. This process includes a comparison of the medications the organization provides to those on the list. A complete list of the patient’s medications is communicated to the next provider of service when it refers or transfers a patient to another setting, service, practitioner or level of care within or outside the organization. Reduce the risk of patient harm resulting from falls. - Implement a fall reduction program and evaluate the effectiveness of the program. 26 Abandoned Babies: • FLMC will offer protective shelter, medical care and treatment in a hospital setting to unwanted, unharmed infants aged seventy-two (72) hours or younger. • An “unharmed condition” can be interpreted as meaning the infant was not harmed through abuse or neglect after being born. • If medical assessment reveals injury or abuse to the infant or if the assessment determines that the infant is greater than 72 hours old, this policy will not be utilized and the appropriate authorities/agencies will be notified. PROCEDURE: • Any hospital employee or student will accept a newborn infant presented for surrender and assure person surrendering newborn that this is a safe haven. • Immediately notify the House Supervisor/designee. • House Supervisor will then obtain an Abandoned Baby-Surrender of Infant Packet. Each packet is coded with a number that corresponds with and ID band for the infant. This identifying number will be used to track infant during hospitalization. Corresponding number appears on self-addressed, stamped envelope provided for return of questionnaire. (Completed packets will be given to the facility Risk Manager for sequestering information necessary to maintain confidentiality. • House Supervisor will accompany parent/person to ER for infant triage and medical screening exam. If the person refuses, a numbered bracelet will be placed on the infant’s arm and leg. • House Supervisor will notify the Administrator on Call. 27 SUICIDE PRECAUTIONS • FLMC is obligated to exercise reasonable care in rendering services to all patients, and this includes the protection of suicidal or severely depressed patients from self-destructive acts. • Suicide Precautions is a set of rules which may be placed into effect by an RN concerned with the clinical care of a patient or by the patient’s attending physician or medical consultants. When ordered, the rules will be followed by all departments involved in the clinical care or other services rendered to a potentially suicidal patient. • Suicide Precautions will remain in effect until the patient is declared “non-suicidal” by the psychiatrist or attending physician and a written order to discontinue suicide precautions is given. • The following shall be considered potentially suicidal: – Any patient admitted for an apparent suicide attempt – Any patient making a suicide attempt while hospitalized – Any patient voicing threats of suicide – Any patient who, in the joint professional judgment of the primary nurse and appropriate nursing supervisor is considered suicidal – Any patient who, in the judgment of the attending physician, consulting physician or psychiatrist, is suicidal 28 EMERGENCY RESPONSE QUICK REFERENCE CHART SYSTEMS FAILURE AND BASIC STAFF RESPONSE Failure of: What to Expect: Who to Contact: Responsibility of User: Computer systems Systems down Information systems Use backup manual / paper system Electrical Power Failure; Emergency Generators Work Many lights are out. Only RED plug outlets work. Plant Ensure that life support systems are on emergency power (red outlets). Ventilate patients by hand as necessary. Complete cases in progress ASAP. Use flashlights. Electrical Power Failure, Total Failure of electrical systems Plant and Respiratory Therapy Utilize flashlights and lanterns, hand ventilate patients, manually regulate IV’s, don’t start new cases. Elevators Out of Service All vertical movement will have to be by stairwells Plant and all Managers Review fire and evacuation plans, establish services on first or second floor, use carry teams to move critical patients and equipment to other floors. Elevator stopped between floors Elevator alarm bell sounding Plant and Security Keep verbal contact with personnel still in elevator and let them know help is on the way. Fire Alarm system No fire alarms or sprinklers Plant Institute Fire Watch, minimize fire hazards, use phone, 2-way radios, or runners to report fire. Medical Gases Gas alarms, no O2, medical air, or Nitrous Oxide Plant and Respiratory Therapy Hand ventilate patients, transfer patients if necessary, use portable O2, and other gases, call respiratory for additional portable cylinders. Medical Vacuum No vacuum, vacuum system fail and in alarm mode. Plant Call Central Supply for portable vacuum, obtain portable vacuum from crash cart, rush cases in progress, don’t start new cases. Natural Gas Failure or Leak Odor, no flames or burners, etc. Plant Open windows to ventilate, turn off gas equipment, don’t use any spark producing devices, electric switches, etc. Nurse Call System No patient contact Bio-Med Use bedside patient telephone if available, move patients; use bells, assign a rover to check patients. Patient Care, Equipment systems including Diagnostic Imaging Equipment / system does not function properly Bio-Med Notify Bio-Med (through Engineering) and tag defective equipment. Sewer stoppage Drains backing up Plant Do not flush toilets, do not use water. Steam Failure No building heat, hot water, laundry; sterilizers inoperative, limited cooking Plant Conserve sterile materials and all linens, provide extra blankets, and prepare cold meals. Use chemical sterilization. Telephones No phone service Plant Use overhead paging, pay phones, use runners as needed. Water Sinks and toilets inoperative Plant Institute Fire Watch, conserve water, use bottled water for drinking, be sure to turn off water in sinks, use RED bags in toilets. Use alternate hand washing methods such as alcohol, foam and wipes. Water Non-Potable Tap water unsafe to drink Plant, Food Services and All Managers Place “Non-Potable Water-Do Not Drink” signs at all drinking fountains and wash basins. Ventilation No ventilation; no heating or cooking Plant Open windows (institute Fire Watch) or obtain blankets if needed, restrict use of odorous / hazardous materials. 29 EMERGENCY CODES AND BASIC STAFF RESPONSE CODE DESCRIPTION INITIAL RESPONSE SECONDARY RESPONSE CODE BLACK Notification of a bomb on campus, usually by an outside caller. Suspicious package or letter Notify PBX Operator of a “Code Black” situation. Obtain as much info as possible. Search the area for a suspicious object. DO NOT TOUCH ANYTHING ! Report all information to security CODE RED Fire and/or smoke present R.A.C.E. Rescue those in immediate danger Activate the alarm; pull manual alarm/call “Code Red” aloud Contain fire (close doors) Extinguish the fire (if safe to do so) Protect people from smoke & fire. Secure the area to prevent fire responders, visitors, and physicians from walking into a hazardous situation. Account for all persons in the area. HAZARDOUS MATERIALS SPILL Chemical, radiation, or infectious material spill presenting hazard to people and the environment. Remove persons from the hazard. Review appropriate spill plan in Safety Manual. Call Environmental Services for mercury spill. All other spills are cleaned up by trained users of the material. Notify the Safety Director. Seek/coordinate medical treatment of decontaminated victim. Person cleaning up the spill will complete a “Chemical Spill Report” and send to Safety Dept. CODE YELLOW Notification of a medical disaster in the community. Complete duties and report to immediate supervisor of availability to assist. Call-in additional staff as needed. Communicate with the Control Center for needs, resources & information. CODE YELLOW Internal evacuation Complete duties and report to immediate supervisor of availability to assist. Account for all persons who were in evacuated area. Communicate with the Control Center for needs, resources & information. CODE PURPLE Hostage Situation An individual is being held against their will by an armed perpetrator Clear the area and establish perimeter to prevent unauthorized entry. Report all pertinent information to Security and Police in charge of response. Provide debriefing for all affected staff. CODE WHITE Spill or release of radioactive substance or identified source of radiation Isolate the spill area (evacuate). Deny entry to others. Notify Nuclear Medicine who will coordinate response. Notify Radiation Safety Officer. Radiation Safety Officer to complete report of the incident and send to Safety Officer & appropriate agencies. CODE PINK Abduction of an infant Assess whether infant has been removed from premises. Notify immediate supervisor. When code pink is announced, search for the abductor. Refer to departmental procedures Marketing/ Public Relations to establish follow-up plan. CODE BLUE A person requiring immediate medical attention Designated team responds to area following PBX announcement. If needed, team requests additional assistance. Review done by Nursing Supervisor and Medical Director. CODE GREEN An employee is in immediate danger Designated team responds to area following PBX announcement. De-escalate violent behavior using verbal intervention Only after verbal intervention fails does team apply physical intervention techniques. Evaluate the response, complete incident report and route to Risk Manager. Notification of Severe Weather in our area Lower beds, close drapes, remove articles from window ledge, cover patients with extra blankets, close doors & windows Assess damage; assure that patients and staff are safe and unharmed. Communicate all building damage to Plant Engineering and/or Control Center. CODE GRAY FOLLOW-UP 30 Only clinical staff and students need to complete the following section. 31 Standards of Care “C.A.R.E.S.” Comfort All patients treated by the nursing staff of FLMC can expect comfort to be optimized through effective utilization of appropriate comfort measures. heAling All patients treated by the nursing staff can expect healing to be promoted through maintenance of effective hydration and nutrition, appropriate medication administration and the recognition, acceptance and support of his/her psychosocial and spiritual needs. Respect All patients can expect to receive respect for his/her rights as a patient and individualized nursing care based on research findings, ethical principles and continuous quality improvement, according to his/her unique health care needs . Education Safety All patients can expect to receive education specific to his/her continuing health care needs. All patients can expect care to be delivered in a safe environment free of nosocomial infections and injurious insults. 32 ABUSE: Adult & Child DEFINITIONS: • Abuse or neglect means the infliction of physical pain, injury or mental anguish, or the deprivation of services by a caretaker which are necessary to maintain the health or welfare of a dependent adult. (See Tennessee Code 71-6-102.) • Child abuse, brutality or neglect means any wound, injury, disability, or physical or mental condition which is of such a nature as to reasonably indicate that it has caused an adverse effect upon the physical or mental health and welfare of a child. • All known or suspected abuse cases MUST be reported to the Case Manager. 33 ABUSE “The five letter word no one wants to think about” Identifying Victims of Abuse • Forms of Abuse: – Neglect: a form of physical abuse involving depriving the person of needed medical services or treatment; failure to provide food, clothing, hygiene, and other basic needs. – Material: misusing a person’s personal property or finances for personal gain. – Emotional: humiliation, harassment, ridicule, and threats of being punished; includes being deprived of needs such as food, clothing, care, a home, or a place to sleep. – Physical: grabbing, hitting, slapping, pushing, kicking, pinch8ing, hair pulling, or beating; includes corporal punishment – punishment inflicted on the body. • Two steps to take if violent abuse is suspected: 1. RECOGNIZE IT 2. REPORT IT TO THE PRIMARY NURSE / CASE MANAGER 34 RESTRAINTS Key Points: 1. The use of restraint should be the final choice for protecting a patient. Alternative interventions should be evaluated prior to restraint use. 2. Alternative interventions may include but are not limited to: 2.1) review of administration, discontinuation, or alteration of current medications 2.2) supervised activity as allowed 2.3) increased monitoring and supervision of the patient by staff 2.4) family or sitters staying with the patient 2.5) diversionary activities 2.6) modification of the patient’s environment 3. Frequent assessment of the patient’s psychosocial and physical status and careful thorough explanation of environment, procedures, and events should be implemented on admission and continue until discharge. This measure may help to prevent the need for restraint. 4. If restraints are deemed necessary, soft restraints are to be used unless the need for heavier restraint is indicated. 5. Restraint for infants and children: 5.1) Hospital policy requires that parents stay with infants and children under age twelve (12). Restraints should not be used unless the parent is unable or unwilling to assist with preventing the child from injuring himself/herself. 5.2) If restraints are indicated for an infant or child, the same procedures apply. Restraint should be the least restrictive that will control the child and should be removed as soon as possible. 6. Consider a constant attendant in addition to the restraint if patient is actively non-compliant, i.e., removing the restraint device. 35 RESTRAINTS DEFINITIONS: – A “physical restraint” is any manual method or physical or mechanical device, material, or equipment attached or adjacent to the patient’s body that he or she cannot easily remove that restricts freedom of movement or normal access to one’s body. – A “drug used as a restraint” is a medication used to control behavior or to restrict the patient’s freedom of movement and is not a standard treatment for the patient’s medical or psychiatric condition. – Seclusion refers to the involuntary confinement of a person alone in a room where the person is physically prevented from leaving. – Forensic and corrective restrictions for security, e.g., handcuffs, applied by a police guard, are not defined as restraint. – Voluntary Restraint – instituted following consent from a cognitively intact patient. Example: an elderly patient who has just taken a sleeping pill and has agreed to have a halter type device applied for the evening as a reminder not to get out of bed without pressing the call button to ask for assistance. – Routine treatment restraint – utilized to assist in a specific treatment or diagnostic procedure such as IV infusions, diagnostic x-rays, catheterizations,etc. Routine treatment restraint is not utilized primarily to involuntarily immobilize a patient. Treatment restraints may include immobilization used during surgery and during non-cognitive states. – Postural/safety supports – utilized to assist the patient in achieving or maintaining proper body position, alignment and balance or compensating for a specific defect. These may be used to prevent non-cognitive patient from falling out of bed or chair. 36 REQUIRED FORMS TO BE TURNED IN UPON COMPLETION OF THIS ORIENTATION SESSION: All Students: •Handbook Receipt •Confidentiality Agreement •Infection Control Post-Test •Safety/Security Post-Test 37 ACKNOWLEDGEMENT CARD AND RECEIPT FOR HANDBOOK The purpose of the Handbook is to provide employees with general information regarding the personnel guidelines the organization attempts to follow in most cases, but NEITHER THIS HANDBOOK NOT ANY PROVISION OF THIS HANDBOOK IS AN EMPLOYMENT CONTRACT FOR ANY OTHER TYPE OF CONTRACT. Due to the nature of Covenant Health operations and variations necessary to accommodate individual situations, the guidelines set out in the Handbook may not apply to every employee or in every situation. Covenant Health reserves the right to rescind, modify or deviate from these or other guidelines, policies, practices or procedures relating to employment matters from time to time as it considers necessary in its sole discretion, either in individual or organization-wide situations with or without notice. All employees at Covenant Health are employed for an indefinite term, and employment may be terminated with or without cause, at any time, at the will of either the employee or the organization. This status can only be altered by a written contract of employment that is specific as to all material terms and is signed by both the employee and a Senior Vice President of Covenant Health. I have read and understand the above statement and agree to read the employee handbook which I hereby acknowledge having received. I also understand that Covenant Health is committed to providing a safe working environment for the employees and the patients we serve. Accordingly, I consent to undergo a drug and/or alcohol test if asked by a manager who has reasonable cause. I understand that refusal of such test will constitute grounds for termination. _________________________________________ Employee Signature _________________________________________ Date 38 INFECTION CONTROL ORIENTATION POST-TEST Name _______________________ School __________________ Date ___________ Circle the correct answer. Page 1 of 2 Bloodborne Pathogen Standard/Isolation 1. According to the Exposure Control Plan, the choice and use of Personal Protective Barriers is based primarily on specific patient diagnosis and not procedure or expected risk. a. True b. False 2. In any procedure where “splash” is a risk, eye protection is always required along with a mask. a. True b. False 3. Gloves – a. Must be changed when contamination has occurred. b. Can be used patient to patient if not visibly soiled. c. Should be worn in the hall since surfaces may be contaminated. d. Should always be worn when cleaning up a blood spill. e. A and C f. A and D g. All of the above 4. When Employee Health Services is closed, the Nursing Supervisor is always notified following a blood exposure incident (needlestick, etc.) a. True b. False 5. Hepatitis immunization is offered free to all employees who are at risk of occupational exposure to blood and other potentially infectious body fluids. a. True b. False 6. All “used” or dirty linen is considered potentially contaminated/infectious. a. True b. False All dirty linen is placed in __________________ colored plastic bags. 7. Needles can only be recapped by using a recapping device or a one-handed technique. a. True b. False 39 INFECTION CONTROL ORIENTATION POST-TEST 2 of 2 Name _____________________________School___________________Page Date________ 8. Full needle disposal boxes are placed inside red lined infectious waste containers for proper disposal and incineration. a. True b. False 9. When Clorox is used as a disinfectant, it should be: a. Diluted 1:10 – 1 part Clorox and 10 parts water b. Used within 24 hours of reconstituting/preparation c. Prepared for use in a labeled bottle d. All of the above 10. Which of the following is the correct procedure for cleaning up a blood spill? a. Notify environmental services immediately and secure the area b. Absorb the spill, spray Clorox solution on the area, bag all waste in a red bag and dispose of if the infectious waste container. c. Put on gloves, absorb the spill, clean area with a detergent, disinfect the area with either a Clorox solution or hospital grade germicide, and dispose of all waste in a red bag as infectious 11. Isolation for known or suspected TB requires which of the following? a. Negative pressure room, personal respirator (PR) b. Positive pressure room, isolation mask c. Any private patient room, as long as orange barrier masks are worn 12. TB skin test must be read 48 hours after placement. a. True b. False 13. In employee follow-up after exposure to blood or body fluid, it is not necessary to report to Employee Health Services as long as an Employee Accident Report Form is completed. a. True b. False 14. Standard Precautions” also known as Universal Precautions apply to all patients and includes the use of personal protective barriers, when contact with blood, any body fluids, non-intact skin and mucous membranes is anticipated. a. True b. False 15. Contact Isolation now includes the wearing of gloves upon entering the patient room. a. True b. False 40 SECURITY / SAFETY ORIENTATION POST-TEST Name _________________________ School ___________________ Date ______ Page 1 of 2 Please answer the following questions. You may refer to your Orientation Handbook for assistance. A score of 100% is required before you may provide patient care. SECURITY 1. What is a “no information” or “closed chart” patient? 2. How will you know if a patient is a “no information” or “closed chart” patient? 3. Weapons are allowed outside of facility (on facility grounds). True or False 4. What should you do if a patient prisoner arrives? 5. Security personnel may be called to escort you to your car. True or False SAFETY 1. What does R.A.C.E. mean? 2. What should you do when you hear a fire alarm? 3. The fire alarm should always be pulled during a real fire and during a fire drill. True or False 4. What can you do to protect yourself from body fluids and hazardous chemicals? 5. What should you do if you discover that the equipment you are using is defective and hazar4dous to a patient or user? 6. You do not have to report accidents that do not result in injury. True or False 41 SECURITY / SAFETY ORIENTATION POST-TEST Name _________________________________________ Page 2 of 2 SAFETY continued: 7. What should you do if there is an accident? Match the letter of the code with the correct response below: A. Code Black B. Code Purple C. Code Pink D. Code Blue E. Code Green F. Code Red G. Hazardous Material Spill H. Code Yellow I. Code White 8. _____ Complete duties and report to immediate supervisor for release to personnel staging area. 9. _____ Isolate the spill area (evacuate). Call nuclear medicine for spill clean-up. J. Evacuation 10. _____ Check for suspicious package and report to security. Immediately notify staff and PBX when bomb treat is received. 11. _____ Clear the area to avoid others from becoming a hostage. 12. _____ Notify all in area of need to evacuate. Evacuate ambulatory, wheelchair, then bedridden. Take records if safety permits. Notify PBX to activate internal evacuation alert. 13. _____ Assess whether infant has been removed from premises. Notify immediate supervisor. When code is announced, search for abductor. 14. _____ Potentially violent person exhibits anger or uncontrolled behavior toward staff. 15. _____ RACE 16. _____ Remove persons from hazard. Trained user cleans up spill. If you can do it safely, assist contaminated victims in decontamination process. 17. _____ Designated team responds to area following PBX announcement. 42 CLINICAL POST-TEST Name ____________________ School____________________ Date _________ Page 1 of 1 1. Define the acronym: C.A.R.E.S 2. The restraint policy states: Patients in restraints must be checked every ________. 3. A ____________ _______________ is any manual method or physical or mechanical device, material, or equipment attached or adjacent to the patient’s body that he or she cannot easily remove that restricts freedom of movement or normal access to one’s body. 4. Select the correct age group who most needs education on a healthy life-style. a. Geriatric c. Teen b. Adult d. All of the above 5. Individualized care based on patient needs and abilities generated by aging is referred to as: a. The Aging Process c. The Nursing Process b. Age Specific Care d. Geriatric Nursing 6. List the four types of abuse. 1. ________________________ 2. ________________________ 3.________________________ 4. ________________________ 7. What are the two steps YOU take if violent abuse is suspected? 1. ______________________________________________________________ 2. ______________________________________________________________ 8. The single most important tool a nurse can use to prove good nursing care is: a. Good hand washing technique c. Physician orders b. Nursing care plan d. Clinical documentation 9. Complete the following list to show all the necessary steps for implementing an Isolation set-up: 1. Stock cart/cabinet 5. ____________________ 2. Place sign on door 6. Alert other departments 3. ________________________ 7. appropriate hand hygiene 4. Ensure alcohol hand cleaner is available 8. _____________________ 10. List the steps you would follow if you are exposed to HIV. 43