Psychosexual Care for Women
with Gynaecological Cancers
Funded by Cancer Australia
Workshop 1:Multi Scenario
Activity: Dispelling common myths about
sexuality
•
•
•
•
•
•
•
Sex causes cancer.
Older people aren’t interested in having sex.
People with cancer don’t want to have sex.
Discussing sex isn’t nice.
People who want to know about sex will ask.
People who are dying are not interested in sex.
Sexuality is only about intercourse.
Session objectives
• Identify dimensions of sexuality
• Identify the common psychosexual effects of diagnosis and
treatment for gynaecological cancer
• Describe principles for communicating about sexuality
• Outline a model for undertaking a psychosexual assessment
• List principles for psychosexual care
Activity: What is sexuality?
• How do you define sexuality?
• Who or what has shaped your definition of sexuality?
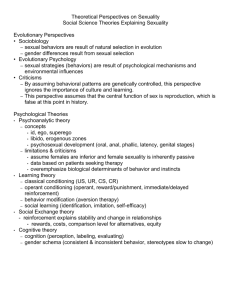
What is sexuality?
• The term 'sexuality' has any number of meanings.
– It can be linked with loving relationships and intimacy
– It can be associated with physical appearance and interpersonal
behaviours
– It can be associated with sexual activity
What is sexuality?
• a person's behaviours, desires, and attitudes related to sex and
physical intimacy with others
National Cancer Institute
http://www.cancer.gov/dictionary/?CdrID=476620]
Factors influencing an Individual’s Sexuality
• Sexuality can be influenced by a range of social, cultural,
psychological and biological factors
Activity: Factors influencing an Individual’s
Sexuality
• Identify clinical situations where you’ve cared for an individual from
a different cultural group to your own.
– Reflect on in ways in which culture may have influenced the
meaning of sexuality to them
– In what ways is this similar and/or different to your own view of
sexuality
Defining Sexual Health and Sexual
Dysfunction
• Sexual health is a state of physical, emotional, mental and social
well-being relating to sexuality. It's not merely the absence of
disease, dysfunction or infirmity.
• Sexual dysfunction is 'the various ways in which an individual is
unable to participate in a sexual relationship … he / she would wish'.
World Health Organization
How common is sexual dysfunction?
• Experiencing sexual dysfunction is relatively common in the
community
• A survey of Australian women reported that 70% experienced sexual
difficulties (including the inability to orgasm and not feeling like sex)
in the year before the survey
Richters J, Grulich, A.E., Visser, R.O., Smith, A.M., Rissel, C.E. (2003).
Australian and New Zealand Journal of Public Health Volume 27,
Issue 2 , pp. 164-170
Identifying Sexual Dysfunction
• DSM-IV identifies the following male and female sexual and gender
identity disorders, which can have organic or psychogenic causes:
– sexual desire disorders
– sexual arousal disorders
– orgasmic disorders
– sexual pain disorders
– gender identity disorder
– sexual dysfunction due to a medical condition
– sexual dysfunction NOS (not otherwise specified)
Gynaecological Cancer and Sexual
Dysfunction
Sexual dysfunction can occur:
• in the months preceding a definitive diagnosis, due to:
– the onset of disease related symptoms including vaginal bleeding
and discharge, pain and fatigue
• during treatments as a result of:
– functional and physiological effects of surgery, radiotherapy,
chemotherapy or other treatment,
– psychological and social effects of a diagnosis and bodily changes
• following completion of treatment, due to:
– longer term physiological, psychological and social sequelae of the
disease and treatments.
Causes of Sexual Dysfunction in
Gynaecological Cancer
• Anatomical changes to the vagina, resulting in vaginal stenosis, or
decreased lubrication
• Hormonal changes, resulting in menopausal symptoms including dry
vagina
• Alterations to reproductive function, resulting in changes to fertility
• Altered bowel and bladder function, resulting in concerns about
incontinence
• Functional limitations, resulting from treatment related fatigue, or
lymphodoema
• Psychosocial effects, for example concerns about body image, fear
of pain, and altered roles and relationships
Case Study: Jane
• 58 year old post-menopausal woman, married to Dave
for 6 years
• Second marriage for both
• Recent TAHBSO and PLND for stage 2 endometrial
cancer
• Adjuvant vault brachytherapy
• Jane has a consultation with the Radiation Oncology
Nurse about her recovery from treatment.......
Case Study: Jane
• Watch the video and answer the following question:
What are the possible psychosexual effects
associated with Jane’s cancer and cancer
treatment?
Jane’s Story part one
Jane’s story part 2
Case study: Susan
• 37 year old woman married to Pete, 2 school-aged kids
• Teacher, working part-time
• Husband has demanding management job, long hours,
frequent trips away
• Recurrent epithelial ovarian cancer
• Currently mid-way through chemotherapy with
Carboplatin and Caelyx
• Parents-in-law staying in family home to help with kids
Case study: Susan
Susan’s story part 1
Case Study: Susan
• During chemotherapy treatment Susan discloses to the nurse
that she is concerned about the impact of the diagnosis and
treatment on her marital relationship
• She is referred to the Clinical Psychologist........
Susan’s story part 2
Case Study: Joan
• 65 year old woman married to George, aged 73
• Presented to Emergency Department with symptoms of bowel
obstruction
• Underwent emergency laparotomy. Findings: stage 1c ovarian
cancer, adherent to bowel resulting in formation of colostomy.
Will require adjuvant chemotherapy
Joan’s story part 1
Case Study: Joan
• Stomal therapist discusses impact of colostomy on body image and
sexual function
• Joan discloses that George is diabetic, with erectile dysfunction. She
is referred to the Social Worker.......
Joan’s story part 2
Principles for Communicating with People
affected by Cancer
about Sexuality
1. Prepare for discussions
• Recognise the difficulty of initiating discussion about sexuality.
• Acknowledge how hard it is to talk about sensitive matters
and reinforce that articulating the problems is the first step
towards resolving them.
• Take a positive stance, reinforce that sexual problems
following cancer treatment are normal and expected, but are
usually temporary.
• Comfort in discussing sexuality improves with practice.
2. Time your discussion
• Psychosexual assessment is not a one-off event. If not identified
at the initial assessment, raise it later.
• Sexual difficulties may arise at different points in the recovery
process. Women vary in their responses.
• Women need to develop rapport and trust with health care
professionals before discussing sensitive matters. The
timeframe for developing this trust is variable.
• Ensuring that sexuality is on a checklist of questions gives
women permission to discuss concerns.
3. Use good communication skills
• Find words and phrases that sound authentic and convey a nonjudgmental value orientation.
• Ask clear, open-ended questions and allow adequate time for
the woman to find words to respond.
• Check with the woman that she understands what you are
asking and seek clarification that you understand.
• Be alert to non-verbal cues of discomfort or distress.
• Use bridging statements and then move from general to specific
questions to facilitate discussion about sexuality.
3. Use good communication skills – Some
examples
• “Now that we’ve talked about how you are managing at home
after the treatment, I would like to ask some questions about
how things are going with your sexual relationship. Is that OK
with you?”
• “I’m really pleased to hear that the treatment side-effects are
settling down. I find for most women at this stage another
area of concern may be sexual function. Are there any issues
there that you would like to discuss?”
4. Use appropriate language
• Don’t make assumptions about the person’s level of
knowledge and understanding.
• Check their understanding of sexual/reproductive anatomy and
function and correct misunderstandings.
• Use simple language rather than formal anatomical terms.
• Check with the woman/couple that your terminology is
understandable and try to use the terminology of the
woman/couple.
• Diagrams are often helpful.
5. Normalise and validate
• Sexuality concerns need to be normalised. Questions about
sexual function should be as routinely asked as questions
about pain, bladder and bowel function and all other treatment
side-effects.
• Acknowledge verbally to the woman that sexuality is a
sensitive and private matter that may be difficult to discuss.
• Seek permission from the woman to raise these matters and
normalise the incidence of post-treatment sexuality changes.
5. Normalise and validate: An example
• “I always ask how things are going with sexual relationships
because it’s really very common to have difficulties after
treatment. Is that something you would like to talk about?”
6. Sensitively address myths and
misconceptions
• Myths and misconceptions about sexuality are common and
may impede resumption of sexual activity, e.g.,
– Sex causes cancer
– Sex will be harmful
• Validation of concerns and encouragement to communicate
with the partner and with health professionals may assist
women in dispelling myths.
7. Determine preferences for involving
partners in the discussion
• Discuss involvement of the partner, and with whom ongoing
sexual assessment and intervention will be arranged .
• Not all women will wish to involve their partner in this process,
e.g.,
– If there is a history of violence, infidelity or sexual abuse in
the woman’s current or past relationships
– If there are cultural or religious taboos around discussing
matters of sexuality, the woman may feel more
comfortable discussing sexuality issues on her own.
Case Study: Anna
• Anna is a 48 year old woman, born in a non-English speaking
country. Migrated to Australia 25 years ago with husband,
Frank. Has two grown up children still living at home.
• Recent radical hysterectomy and PLND for stage 1a2 cervix
cancer. No adjuvant therapy required
• Seen by Clinical Psychologist for routine psychosexual
assessment.........
Case Study: Anna
• Anna identifies multiple concerns:
about her diagnosis
about her relationship with Frank
about her recovery from treatment
• Identify what these concerns may be
Anna’s story part 1
Case Study: Norma
• Norma is aged 78 and has been widowed for 15 years
• She lives alone and is independent in ADL’s; she enjoys a
close relationship with her 4 children and their families
• Active in her community; church, bowls, senior citizen’s
• Underwent wide local excision and bilateral groin node
dissection for a stage 1 SCC of vulva. No adjuvant therapy
required.
Norma’s story part 1
Case Study: Norma
Seen by Social Worker for routine psychosexual
assessment.........
• What potential barriers are there to communicating with
Norma about her sexuality?
• What communication skills does the social worker use to
facilitate discussion with Norma about her sexuality?
Norma’s story part 2
Undertaking a Psychosexual
Assessment
Undertaking a Psychosexual Assessment
• Comprehensive assessment of psychosexual concerns needs
to include an understanding of all intimate behaviours and
practices for giving and receiving sexual pleasure/satisfaction.
• Sexuality is multidimensional, encompassing concepts of
body image, self-esteem, intimacy, emotional adjustment,
interpersonal communication and a diverse range of sexual
behaviours.
Ex-PLISSIT Model for Assessment
• Permission: Give permission for the patient to have sexual
feelings / relationships and normalise this.
• “Many women diagnosed with cancer find that it has an
impact on their relationships and their interest in sex. Is it ok if
we discuss this issue?”
Ex-PLISSIT Model for Assessment
• Limited Information: Provide limited information to identify the
effect of the cancer / treatment on sexuality. Correct any
misconceptions, dispel myths, provide accurate information.
– “Treatment side effects often have a big impact on sexual
activities. You mentioned that you started having
intercourse again but it is still painful after treatment. How
is this pain affecting your sex life?”
Ex-PLISSIT Model for Assessment
• Specific Suggestions: Make specific suggestions to manage
the sexual side effects they have identified.
– “There are many ways that couples can adapt their sex
lives to adjust to the effect of the cancer and treatment. To
address the issue of pain, you could consider which
activities you can still enjoy when feeling sore from
treatment, and focus on these instead of intercourse until
you have recovered fully. How would you and your partner
feel about focusing on other types of sexual activity?”
Ex-PLISSIT Model for Assessment
• Intensive Therapy: Identify further support for the issues you
have discussed, and refer them if appropriate.
– “Some women find it helpful to get more support for the
issues we’ve discussed. You mentioned that you are
feeling pressure to keep your sex life the way it has always
been, and it is making you very distressed, but you can’t
talk to your partner about it. Would you like to see a
counsellor who is experienced in this area?”
Interventions to Manage Specific
Psychosexual Sequelae
Principles for intervention
• Normalise the incidence of post-treatment sexuality changes
and facilitate positive communication
• Treat the underlying cause where possible (physical,
psychological, social)
• Minimise effects of anatomical changes, e.g. use of vaginal
dilators
• Provide symptom relief
• Provide information and advice on alternative methods for
showing intimacy, and for giving and receiving sexual
pleasure; involve the partner if appropriate
• Refer to specialised services where required
Managing vaginal dryness
• The most effective solution for vaginal dryness is to use a
product that adds moisture to the vaginal tissue
• Evidence suggests vaginal moisturisers and lubricants can
increase vaginal moisture, vaginal fluid volume, vaginal
elasticity and a return to premenopausal pH.
• There are 3 types of products for improving vaginal moisture
Vaginal moisturisers
Vaginal lubricants
Vaginal oestrogens
• General suggestions include using unperfumed soaps and
wearing cotton underwear
Sexuality in Palliative Care (Lemieux et al 2004)
• Qualitative study to explore what ‘sexuality’ meant to 10
palliative patients and how their illness had affected their
sexuality
• Emotional connection to others was integral component of
sexuality and took precedence over physical expressions of
sexuality
• Sexuality continues to be important at the end of life, even in
the last weeks and days
• Lack of privacy, shared rooms, staff intrusion and single beds
were considered barriers
• All felt sexuality should be addressed as an integral
component of their care – only raised with one patient
Enhancing sexual intimacy at end of life
• Give couples private time
• Remove extraneous equipment & make environment less
clinical
• Reassure couple that kissing, stroking, massaging and
embracing won’t cause physical harm and may lead to
relaxation and decreased pain
• Fatigue can decrease a person’s ability to maintain personal
grooming
• Mouth care is paramount
• Maintaining personal dignity is essential when providing
intimate care
• Ensure symptoms are well managed
• Positioning
Case Study: Susan
• Susan had surgery and adjuvant chemotherapy for stage 3
ovarian cancer diagnosed 3 years ago.
• She has had multiple recurrences and has now been referred
to the community palliative care nursing service.....
Case Study: Reintroducing Susan
• Susan had surgery and adjuvant chemotherapy for stage 3 ovarian
cancer diagnosed 3 years ago.
• Susan has had multiple recurrences and has now been referred to
the community palliative care nursing service.....
Susan’s story part 4
Case Study: Reintroducing Susan
Susan’s story part 5
Find these topics in the PSGC online resource….
• What is sexuality?
Go to Module 1 and complete the module
• Principles for communicating with people affected by
cancer about sexuality
Go to Module 3 (section 3.1) and access the Psychosexual
communication principles
• Ex-PLISSIT Model for Assessment
Go to Module 3 (section 3.3.2) and access the assessment
tools
• Managing specific psychosexual sequelae
Go to Module 6 for specific treatments
Find palliative care in the PSGC resource….
• Enhancing sexual intimacy at end of life
Go to Module 6 (section 6.4.1) for ‘couples in palliative care’
• Women with special needs
Go to module 2 (section 2.1.6) for ‘understanding the
experience’ of palliative care advanced disease
• Overcoming barriers
Go to module 3 (section 3.5.2) for enquiring and responding in
the palliative care phase
Search function
• Use the search function for quick access to relevant topics
• Located top right hand corner all pages of the resource
Acknowledgements
Funded by:
Disciplines represented in Project
Working Group & module review :
Cancer Australia
Project team:
Professor Patsy Yates
Kath Nattress
Kim Hobbs
Ilona Juraskova
Kendra Sundquist
Project Officer:
Lynda Carnew
Project Working
Group:
Dr Margaret Davy
(Chairperson)
Consumer
Gynaecological Oncologist
General Practitioner
Radiation Oncologist
Gynaecological Clinical Nurse Specialist
Gynaecological Clinical Nurse Consultant
Psychologist
Research Psychologist
Social Worker
Education Services Manager
Patient Programs Officer
Sexual Health Educator
www.cancerlearning.gov.au