New Anticoagulants
advertisement

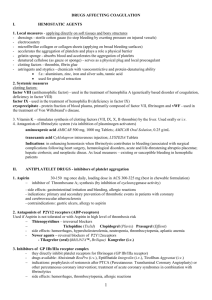
New Anticoagulants: Beyond Warfarin and Heparin Rachel LaCount Resident in Pathology August 4, 2005 Overview • Older anticoagulants: Warfarin & Heparin, LMWH • Why we need new drugs • Newer drugs – Direct Thrombin Inhibitors – Xa inhibitors – Heparinoids – The future Brief Review: Warfarin MOA • Blocks vitamin Kdependent glutamate carboxylation of precursor factors II, VII, IX, X • Vit K = cofactor • Warfarin blocks the reduction of Vit K • Oral administration Review: Heparin MOA • • • • Indirect thrombin inhibitor: IV only Called UFH (unfractionated heparin) Complexes with AT (heparin co-factor I) AT by itself inactivates SLOWLY! – Thrombin – Factor Xa – XIIa, XIa, IXa (lesser extent) • AT + Heparin: conformational change in AT = 1000-4000 fold acceleration in inactivation • At high concentrations: Also binds to platelets and heparin co-factor II—which inhibits thrombin • Heparin made of polysaccharide chains of varying lengths • Unique pentasaccharide sequence binds to AT – Sequence is randomly distributed along heparin chains • Inactivation of Xa—Heparin doesn’t have to bind to it • Inactivation of Thrombin--Requires heparin to bind to both AT and itself – Heparin must be >18 monosaccharides long to do this – Virtually all heparin molecules are > 18 Limitations of Warfarin and Heparin: • Both have narrow therapeutic windows • Highly variable dose responses: requires laboratory monitoring (PT, APTT) – Heparin can bind to other plasma proteins making bioavailability variable – Warfarin has numerous food, drug interactions • Limited ability to stop a clot from propagating: – Heparin does not inactivate thrombin bound to fibrin or Xa bound to platelets very well LMWHs • Molecular wt: Heparin: 15,000 vs LMWH: 4000-5000 • LMWHs inactivate Xa but have less effect on thrombin (some molecules not long enough) – ratio of anti-Xa to anti-thrombin activity of 3:1 – Do not prolong PTT unless dose high • Advantages over heparin: – Easier to administer: sq, BID dosing – Dosage and anticoagulant effect easier to predict; dose based on body weight – Lab monitoring not necessary in all patients – Less chance of inducing immune-mediated thrombocytopenia Names of LMWHs • Enoxaparin (Lovenox) • Dalteparin (Fragmin) • Tinzaparin (Innohep) – Differ chemically and pharmacokenetically but unsure if these differences are clinically significant • Other products not yet approved here: – Fraxiparin, reviparin, nadroparin, bemiparin, certoparin LMWH Rx monitoring • Uncomplicated patients do not require monitoring • Who may need to be? – Newborns, children, pregnant women – Conditions: obesity, renal insufficiency, malignancy, myeloproliferative disorders – People with hemorrhagic complications or with initial therapy to confirm appropriate levels LMWH Rx monitoring • Levels measured by chromogenic-based anti-factor Xa assays • Clot based APTT only sensitive to very high levels of LMWHs • Calibration is done with the same brand of LMWH that the patient is using—and not with Heparin! Anti Xa Assay • Pt plasma + known amount of excess Factor Xa and antithrombin • UFH/LMWH binds antithrombin & inhibits Factor Xa • Residual Factor Xa is measured – Factor Xa cleaves a chromogenic substrate similar to its natural substrate, releasing color detected by a spectrophotometer • Residual Xa is inversely proportional to the amount of LMWH (or UFH) Why new drugs? • UFH and LMWHs are inconvenient for the outpatient setting (IV or sq only) • UFH and LMWHs can cause HIT: – Risk 0.2% with LMWH vs. 2.6 % with UFH – Pts with HIT still need to be anticoagulated Why new drugs? • Warfarin is underused in pts who need it most: – Only 47% of patients with afib are taking warfarin – This is often due to hemorrhagic contraindications – Convenience issues due to the need for frequent monitoring – Difficulty in maintaining optimal anticoagulation The ideal anticoagulant • • • • • • • • • Effective Minimal complications/side effects Convenient administration (ie: oral for outpatients) Rapid absorption Fast on and offset action Predictable pharmacokinetics No interactions with food or drugs No HIT No coagulation monitoring Categories of new drugs – Direct Thrombin Inhibitors: • hirudin, lepirudin, desirudin, bivalirudin, argatroban, ximelagatran – Xa inhibitors: • fondaparinux, idraparinux – Heparinoids: • Danaparoid (discontinued) Objectives for each drug • • • • Mechanism of Action Current uses Limitations Monitoring in the lab Direct Thrombin Inhibitors Direct Thrombin Inhibitors • 3D structure of thrombin: 100s of thrombin inhibitors in last 15 yrs • Most are peptidomimetic compounds – Mimic the fibrinogen sequence which interacts with the thrombin active site – Peptidomimetic: A compound that mimics binding and biological activity of the natural peptide Thrombin 3 important areas: 1. Active site: fibrinogen binding 2. Exosite I: major docking site--interaction with fibrinogen and other receptors; fibrinogen recognition site 3. Exosite II: interacts with heparin Hirudin • Medicinal leeches: – Used since ancient times to relieve body of “bad humors” • Egyptians, Greeks – Reached peak popularity in mid-19th century Hirudo medicinalis • 1884: John Haycraft in Birmingham demonstrated that medicinal leeches, Hirudo medicinalis, secrete a substance that prevents blood from clotting • 1904: Substance named hirudin • 1957: Markwardt isolated the active anticoagulant substance, determined it to be a polypeptide 65 AAs long which inhibited thrombin • Estimated to require 50,000 leeches annually for diagnostics and treatment • 1986: DNA isolated and cloned • Today recombinant hirudin is made in yeast cells – Lepirudin, desirudin, bivalirudin R-Hirudins • • • • All bind in active site and exosite I Irreversible: Lepirudin, Desirudin Reversible: Bivalirudin Minor differences in structure between them – ie: Lepirudin has one extra oxygen molecule than desirudin and one AA difference • Lepirudin (Refludan) – Approved for use in HIT • No binding to platelet factor IV • 89% of patients with rapid increase in plt count – Monitored with APTT daily • • • • Measure 4 hr after dose Target: Pt’s APTT to be 1.5-2.5 x the lab’s median APTT Caution in pts with renal insufficiency Dose dependent relationship – Antihirudin antibodies develop in 40-70% • Drug is made of non-human proteins • Can cause irritation to skin • Not neutralizing; may enhance drug potency by delaying clearance • These patients need to be monitored with APTT • Desirudin (Iprivask) – Studied in DVT prophylaxis for total hip • Lower rate of DVT than LMWH and no increase in bleeding complications – Also used in HIT – Also monitored with APTT • Monitor especially in pts with renal insufficiency • APTT twice upper limit of normal = stop and restart at reduced dose • Dose dependent relationship – Antihirudin antibodies can also develop • Bivalirudin (Angiomax) – Previously called hirulog – Binds reversibly to thrombin • Thrombin slowly cleaves the drug from its active site • Short half-life 20-30 min – Less immunogenic (is only 20 AAs long) – FDA approved in 2002 for use in angioplasty for patients with unstable angina • Bivalirudin, cont… – REPLACE-2 (2004) • Randomized Evaluation in PCI Linking Angiomax to Reduced Clinical Events • Pts randomized to receive either bivalirudin or heparin + GP IIb/IIIa inhibitor during PCI • Significant reduction in in-hospital bleeding • Endpoints about equal: MI, urgent repeat revascularization • Trend towards decreased mortality – Undergoing study for use in cardiac surgery for use both “on pump” and “off pump” – Monitored with APTT or ACT Direct Thrombin Inhibitors, cont… • Argatroban (Novastan) – Binds at active site reversibly – Does not bind at exosites – First introduced in Japan in 1990 for treatment of peripheral vascular disorders • Argatroban, cont… – FDA approved in 2000: Anticoagulant for pts with HIT needing prophylaxis or treatment for thrombosis – 2002 approved for pts with or at risk for HIT undergoing PCI – Small, without immunogenicity – Monitoring with APTT or ACT recommended • Desired APTT: 1.5 to 3 times the initial baseline value (not to exceed 100 seconds) • Ximelagatran (Exanta) – ORAL !!!!! BID dosing – Only binds to active site; reversible – Prodrug for melagatran – Numerous Phase III trials (10): • 6 for prophylaxis of venous thromboembolism [VTE] due to orthopedic surgery • 1 for initial treatment of VTE • 1 for long-term prevention of VTE recurrence • 2 for stroke prophylaxis due to atrial fibrillation – The good news: Some studies have shown benefit over warfarin or LMWH Ximelagatran, cont… The bad news: • Studies have shown increase in bilirubin, ALT • FDA: Estimates rate of liver injury 1 in 200 • 10% could progress to liver failure, need liver transplantation, or death – 1 in 2000 patients tx’d long-term could have overt liver failure • 3 of 6948 patients did die under circumstances that FDA felt could reasonably be related to ximelagatran – Consistent with the 1-in-2000 rate DTIs…a bit more on lab testing • Interference with APTT: – Other drugs: warfarin, abx – Pts with LA – High factor VIII levels leading to falsely low APTT • Why not do a Factor IIa assay to measure drug activity? – For example, chromogenic anti-factor IIa assay – Limited reproducibility, linearity, and sensitivity DTIs… • Why not use PT/INR? – Little to no sensitivity to some Rx and less than optimal to others – INR can be markedly different depending on reagent used – One recent study of lepirudin, argatroban, & bivalirudin observed a dose dependent effect on the INR • PT/INR most affected by argatroban at therapeutic concentrations • Lepirudin had the least overall effect on PT/INR DTIs & Lab tests, cont… • TCT (thrombin clotting time) – Seems logical, but is overly sensitive to these drugs and doesn’t provide useful clinical info • ACT (activated clotting time) – Has been used successfully in the OR • ECT (ecarin clotting time) – Not standardized for clinical use, but shows promise – Venom from snake Echis carinatus: • Converts prothrombin to a meizothrombin that is sensitive to thrombin inhibitors Factor Xa inhibitors Factor Xa inhibitors • Fondaparinux (Arixtra) – Synthetic polysaccharide: – The drug is the unique pentasaccharide sequence that UFH and LMWH use to bind to AT – Reacts with strong affinity to AT (reversible) → Induces conformational change in AT → Increased ability to inactivate Xa Fondaparinux: Too short to inactivate thrombin (much like LMWH); need >18 saccharide units to inactivate thrombin • Fondaparinux, cont… – Does not interact with plasma proteins, platelets, or platelet factor IV = useful in HIT (although not yet formally approved) – FDA approved in 2001 • Prevention of post op VTE (DVT and PE) in orthopedic surgery – Hip fracture, hip replacement, knee replacement – Fondaparinux vs. enoxaparin in one study decreased VTE in knee replacement from 12.5 to 27.8% • 2004/5 approval: – VTE treatment if administered with warfarin – Anticoagulation in abdominal surgery • Potential uses being studied: MI, PCI, UA • Fondaparinux, cont… – Drug monitoring: • APTT and PT are insensitive • PT/INR may or may not be proportional to the clinical safety or efficacy—more studies needed • Anti-factor Xa assay –must be calibrated with fondaparinux – Long half-life (17 hours) = qd dosing (LMWH = BID) • Idraparinux – Longer acting analogue (q week dosing) currently being developed Danaparoid (Orgaran) • A LWM heparinoid • Derived from porcine gut mucosa – (can’t use if have a pork allergy) • A mixture of heparan sulfate, dermatan sulfate, chondroitin sulfate • Does not have heparin or heparin fragments (heparan differs from heparin by sulfur groups on the sugar molecules) Danaparoid: MOA • Binds to AT and heparin cofactor II • More selective at inhibiting Xa than LMWH, not as selective as fondaparinux: Drug UFH LMWH Danaparoid Fondaparinux Anti-Xa/anti-IIa ratio 1:1 2-4:1 22:1 ∞ • Ability to prevent extension of thrombi • Minimal effect on platelet function and aggregability Danaparoid • FDA approved in 1996 – Proven effective in DVT prophylaxis in pts undergoing hip surgery • Used off label in patients with HIT • Discontinued manufacturing in USA 4/2002 due to problems obtaining raw material – Available in Germany Future possible drugs • Ticks Isolated from the saliva or blood of various species: – Thrombin inhibitors – Factor Xa inhibitors, – Tissue factor pathway inhibitor (TFPI) Future possible drugs • Razaxaban – Oral drug – Inhibitor of factor Xa without requiring AT – In phase II trials • DX-9065a – Xa inhibitor; also in phase II trials; IV • Potential targets being developed – TF/fVIIa • Recombinant tissue factor inhibitor (FTPI) • Other specific TF/fVIIa or fVIIa inhibitors being developed – Recombinant APC • In phase III trials—inactivates Va and VIIIa Future possible drugs • Aptamers: – From root word aptus (“fit”) – Single stranded nucleic acids that fold into specific 3D structures which bind and inhibit a protein target – Anti factor VIIa, IXa, and thrombin aptamers have been developed – Should be nonimmunogenic—small and similar to endogenous molecules – Possible use in HIT References • Angelli, G. Current issues in anticoagulation. Pathophysiology and Haemostasis and Thrombosis. 2005;34(suppl 1):2-9. • Bauer, K. Clinical uses of fondaparinux. Uptodate. • Davidson, B. Preparing for the new anticoagulants. J of Thrombosis and Thrombolysis. 2003;16 (1/2): 49-54. • DiNardo, J. Fondaparinux. Newsletter. Society of Cardiovascular Anesthesiologists. 2003 Dec. (http://www.scahq.org/sca3/newsletters/2003dec/drug4.shtml) • Gosselin, RC, et al. Effect of direct thrombin inhibitors, bivalirudin, lepirudin, and argatroban, on prothrombin time and INR values. Am J Clin Pathol. 2004;121:593-99. • Hirsh, J. et al. Heparin and low-molecular-weight heparin. Chest. 2004;126:188S-203S. • Kikelj, D. Peptiomimetic thrombin inhibitors. Pathophysiology of Haemostasis and Thrombosis. 2003/2004;33:487-491. • Lai, R. et al. A thrombin inhibitor from the ixodid tick, Amblyomma hebraeum. Gene. 2004 Nov 24; 342(2):243-9. • Lawrence, LK. New anticoagulants. Uptodate. References, cont… • Markwardt, F. Past, present and future of hirudin. Haemostasis. 1991;21 Suppl 1:11-26. • Martel, N. et al. Risk of heparin induced thrombocytopenia with unfractionated and low molecular weight heparin thromboprophylaxis: a meta-analysis. Blood. 2005 Jun 28 (Epub ahead of print). • Nimjee, S. et al. The potential of aptamers as anticoagulants. TCM. 2005; 15(1):41-45. • Starke, K. The beginnings of hirudin. Trends Pharmacol Sci. 1989 Mar; 10(3):99. • Walenga, J. et al. Monitoring the new antithrombotic drugs. Seminars in Thrombosis and Hemostasis. 2004; 30(6): 683-695. • Weitz, J. et al. Treatment of venous thromboembolism: New anticoagulants for treatment of venous thromboembolism. Circulation. 2004;110:I-19 – I-26. • White, CM. Thrombin-directed inhibitors: Pharmacology and clinical use. American Heart Journal. 2005 Jan;149(15):S54-60. • Valentine, K. et al. Clinical use of heparin and low molecular weight heparin. Uptodate