Functional Abdominal Pain In Childhood and Adolescence
advertisement

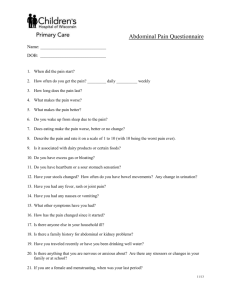
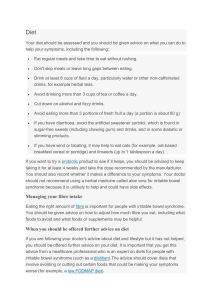
Recurrent Abdominal Pain In Childhood and Adolescence Cheryl A. Little, MD clitt002@stvincent.org St. Vincent Pediatric Gastroenterology 8402 Harcourt Rd. Suite #402 Indianapolis, IN 46260 (317) 338-9450 IMPORTANT POINTS • Recurrent Abdominal Pain (RAP) represents a description of symptoms, not a diagnosis • The most common cause of RAP is a functional gastrointestinal disorder (FGID) • There are 4 major pediatric disorders associated with recurrent abdominal pain • Functional abdominal pain syndrome • Functional dyspepsia • Irritable Bowel Syndrome (IBS) • Abdominal Migraine • A FGID is a positive diagnosis • Therapy of a FGID is directed at environmental modification Introduction • RAP is not a diagnosis • Clinical manifestation of an organic disorder (23.6%) (Indian Pediatrics; 46: 389-399, 2009) • Due to a FGID • Diagnosis of a FGID meets specific criteria (Rome III criteria) • Red flag symptoms concerning for an organic disorder Pain that awakens the child Significant vomiting, constipation, diarrhea, bloating, or gas Blood in the stool Unintentional weight loss or slowed growth Changes in bowel or bladder function Pain or bleeding with urination Abdominal tenderness Epidemiology • FGID occurs in 10-12% of school-aged children • 21% severe enough to affect activity (J Pediatr 129:220-226, 1996) • Female-to-male ratio equal up to 9 yrs of age • Female-to-male ratio 1.5:1 btw 9-12 yrs of age • Onset of pain <4 yrs • More in-depth organic evaluation Pathophysiology of FGIDs • Different presentations • Heterogeneous group of disorders • Variable expressions of the same disorder • Prevailing viewpoint • Pain is visceral in origin • Involves disordered GI motility • Involves visceral hypersensitivity/hyperalgesia • Genetic vulnerability • Abnormalities in the enteric nervous system • Dysfunction of the autonomic nervous system • Altered awareness of discomfort (emotions, cognitive processes, CNS influences) General Approach to RAP • History • Complete history is the MOST important component of the evaluation (Attempt to obtain directly from patient) • Focus on • Timing, frequency, location, quality of pain • Associated GI symptoms (nausea, vomiting, diarrhea, constipation, blood in stool or emesis) • Precipitating/relieving factors • Systemic symptoms ( fever, wt loss, joint pain, skin rash) • Family History of IBD or PUD • Travel History • Medication and nutritional interventions • Interference with school, play, peer relations, and family dynamics General Approach to RAP • Physical Examination • Complete and not only directed toward the abdomen • Growth data • ?Fall off in height or weight velocity • Delay in pubertal development • Abdominal examination • General appearance, auscultation, palpation of liver and spleen, for masses and tenderness • Rectal examination • Perianal and digital • Clubbing, rashes, arthritis • Pelvic examination (if indicated by history) Rome Criteria III • Functional Abdominal Pain Syndrome • At least 8 weeks of episodic or continuous abdominal pain in a school-aged child or adolescent occurring at least once/wk with one or more of the following: • some loss of daily functioning • additional somatic symptoms such as headache, limb pain, or difficulty sleeping • The patient has insufficient criteria for other functional GI disorders that can explain the pain • No evidence of an inflammatory, anatomic, metabolic or neoplastic process that is likely to explain the symptoms Gastroenterology 2006;130:1527-1537 Functional Abdominal Pain Syndrome • Periumbilical location • Variable in severity • Pain episodes tend to cluster alternating with pain-free periods of variable length • Associated GI symptoms are denied by the patient Functional Abdominal Pain Syndrome • Pain episodes begin gradually • Last less than 1 hr in 50% • Last less than 3 hrs in 40% • Continuous pain in < 10% • Child is unable to describe the pain • Radiation of pain is rare • Temporal relationship to meals, activity, bowel habits is unusual Functional Abdominal Pain Syndrome • Pain rarely awakens the child from sleep • Parents describe the patient as “miserable” and “listless” during pain episodes • During severe attacks the child may exhibit a variety of motor behaviors (“doubling over in pain”) • Common associated “autonomic” symptoms • Headache, pallor, nausea, dizziness, fatigue • At least one is observed in 50-70% of cases Functional Abdominal Pain Syndrome • Differential Diagnosis • Infectious • UTI, Giardia • Carbohydrate intolerance- Lactose, fructose, sorbitol, sucrase-isomaltase • Inflammatory • Crohn disease, ulcerative colitis, eosinophilic gastroenteritis, celiac disease, pancreatitis • IBS • Constipation with or without fecal impaction • Psychogenic Functional Abdominal Pain Syndrome • Diagnosis • There is no dependable biological marker for functional abdominal pain syndrome • Most reliable diagnostic features are the symptoms • Should NOT require a series of diagnostic tests to rule out organic causes of pain • Reasonable to obtain CBC, ESR or CRP, UA and culture, KUB, CMP, O+P, fecal leukocytes, lactose tolerance testing/lactose elimination • US and CT are low yield • Excessive testing may increase parental anxiety and put the child through unnecessary stress • Parental anxiety/uncertainty increases the stressful environment that provokes and reinforces the pain behavior Functional Abdominal Pain Syndrome • Treatment • Begins at initial office visit • Important to introduce the concept of functional pain during the initial evaluation • Review the differential diagnosis to reassure parents and child that specific organic disorders have been considered and “red flags” are absent Functional Abdominal Pain Syndrome • Treatment • Focus of treatment is not “cure” but management of symptoms and adaptation to illness to provide a satisfactory quality of life through support and education • Accomodative or secondary engagement coping (distraction, acceptance, positive thinking, cognitive restructuring) is related to less pain • Passive or disengagement coping (denial, cognitive avoidance, behavioral avoidance, wishful thinking) is associated with increased levels of pain Functional Abdominal Pain Syndrome • Treatment • Directed toward environmental modification • Identify, clarify, and reverse stresses that may provoke or increase the perception of pain • Reverse environmental reinforcement of the pain behavior • Lifestyle MUST be normalized regardless of the continued presence of pain • Parents should direct less social attention toward the symptoms Functional Abdominal Pain Syndrome • Supportive counseling • Target at illness behavior • Can be delivered by primary care physician • Listening, empathy, encouragement • Do not allow ongoing pain-induced disability • Patient-centered participatory arrangement • Instruct parents how to respond to symptoms • Encourage school officials to participate in treatment Functional Abdominal Pain Syndrome • Treatment • Pharmacologic therapy directed at reasonable physical triggers of pain • Constipation • Altered motility • Low-dose tricyclic antidepressants • Act as “central analgesics” • Raise the perception threshold for abdominal pain • Down regulate pain receptors in the intestine • Generally reserved for patients with anxiety/depression or maladaptive illness behavior Functional Abdominal Pain Syndrome • Treatment • Hospitalization • Reinforces pain behavior • Consultation • Reserved for patients with depression/anxiety, PTSD, abuse, severe disability, maladaptive illness behavior, chronic refractory pain • Child Psychiatrist • Child Psychologist • Behavioral modification therapy Rome Criteria III • Functional Dyspepsia • At least 8 weeks (which need not be consecutive) in the preceding 12 months of persistent or recurrent pain occurring at least once/week centered in the upper abdomen AND • No evidence of an inflammatory, anatomic, metabolic or neoplastic process that is likely to explain the symptoms AND • No evidence that dyspepsia is exclusively relieved by defecation or associated with a change in stool frequency or form Gastroenterology 2006;130:1527-1537 Clinical Presentation • Functional Dyspepsia • • • • Pain localized to the epigastrium, RUQ, or LUQ Episodic vomiting Temporal relationship with meal ingestion Presence of anorexia, nausea, oral regurgitation, early satiety, post-prandial bloating, indigestion, and belching Functional Dyspepsia • No symptoms or signs that reliably distinguish functional dyspepsia from upper GI organic disorders • More extensive diagnostic evaluation than functional abdominal pain syndrome • Usually associated with the same signs of environmental reinforcement of pain behavior Functional Dyspepsia • Two groups • Ulcer-like dyspepsia • Pain most common symptom • Dysmotility-like dyspepsia • Often report nausea, fullness, and early satiety Functional Dyspepsia • Differential Diagnosis • Acid-related disease • Gastritis, duodenitis, esophagitis, peptic ulcer • Infection • Helicobacter pylori • Allergic/Inflammatory • Eosinophilic esophagitis, eosinophilic gastroenteritis, gastoduodenal Crohn disease, celiac disease • Gastroparesis • Chronic cholecystitis • Chronic fibrosing pancreatitis Functional Dyspepsia • Diagnosis • Physical exam- findings usually normal • Lab evaluation- CBC,ESR or CRP,amylase, lipase, hepatic panel, H. pylori serology or stool antigen • UGI +/- SBFT • Abdominal US • Nuclear medicine scintigraphy (HIDA scan) • Upper Endoscopy- patients with dysphagia, persistent symptoms despite the use of acid-reducing medications, or to confirm H. pylori infection. • ERCP Functional Dyspepsia • Treatment • Positive diagnosis, education, establishment of realistic expectations of treatment • Environmental and dietary modification • Avoid cigarette smoking, advise smoke-free home • Avoid alcohol, non-steroidal analgesics • Avoid caffeinated beverages, high-fat foods, and large meals • Address psychological comorbidity Functional Dyspepsia • Treatment • Drug therapy • 70% improvement rate by 1 year following diagnosis (JPGHAN 30: 413-418, 2000) • Ulcer-like dyspepsia • 4-6 week course with H2-receptor antagonist or PPI • Dysmotility-like dyspepsia • 4-6 week course with a prokinetic agent (metoclopramide or erythromycin) • Anti-emetics or low-dose tricyclic antidepressants • Serotonic agents- Buspirone (Buspar), Paroxetine (Paxil) Rome Criteria III • Irritable Bowel Syndrome • At least 8 weeks in the previous 12 months of abdominal discomfort or pain occurring at least once/wk with at least 2 of the following: • relief w/defecation • onset associated w/change in frequency of stool • onset associated w/ change in form of stool • No evidence of an inflammatory, anatomic, metabolic or neoplastic process that is likely to explain the symptoms Gastroenterology 2006;130:1527-1537 Irritable Bowel Syndrome • More common in adolescence • Pain is typically localized to the lower abdomen • Association of pain with altered bowel pattern • Diarrhea (4 or more stools per day) • Constipation (2 or less stools per week) • Sense of incomplete evacuation • Straining • Urgency • Passage of mucus • Feeling of bloating or abdominal distention • Pain is often relieved by defecation Irritable Bowel Syndrome • Differential Diagnosis • Infection • Giardia • Chronic Clostridium difficile colitis • UTI • Carbohydrate intolerance • Lactose, fructose, sorbitol, sucrase-isomaltase deficiency • Inflammatory • Crohn disease, ulcerative colitis, eosinophilic gastrenteritis, celiac disease • “Microscopic” colitis Irritable Bowel Syndrome • Diagnosis • Careful, sympathetic history taking • Appropriate, thorough PE ( to include rectal exam) • Negative routine diagnostic studies • Empiric lactose elimination • Full assessment of psychological and social factors as well as physical symptoms Irritable Bowel Syndrome • Diagnosis • Colonoscopy is indicated in pts in whom the history or PE suggest the possibility of IBD Evidence of GI bleeding Profuse diarrhea Involuntary wt loss or growth deceleration Fe deficiency anemia Elevated ESR or CRP Extra-intestinal symptoms (fever, recurrent mouth sores, rash, joint pain) Irritable Bowel Syndrome • Management • Symptomatic and supportive care • Development of a positive relationship between doctor and patient/parents • Validate the symptoms that they are experiencing • Address the patient’s agenda by asking directly about their concerns and fears • Initial Management • Positive, confident diagnosis communicated with clarity and honesty • Educate about the pathophysiology of FGIDs and bring focus to the multifactorial nature of IBS Irritable Bowel Syndrome • Dietary Management • Constipation predominant • Insoluable fiber diet ( root vegetables, skinned fruits, bran, whole-wheat products) • Diarrhea predominant • Eat slowly, avoid chewing gum, avoid excessive intake of alcohol, carbonated and caffeinated beverages, high-fat foods, legumes, and foods or beverages with fructose or sorbitol • Soluable fiber diet (dried beans and fruits, peas, oats, barley, carrots, flesh of fruits such as apples and organges) • Response rates of 70% (Lancet 2: 1115-1117, 1982) Irritable Bowel Syndrome • Drug Therapy • Antispasmodics • Anticholinergics • Used in diarrhea predominant or variable stool IBS • Dicyclomine-Bentyl • Hyoscyamine-Levsin,Levbid • Enteric-coated Peppermint Oil • Amitiza- chloride channel activator • Indicated for constipation predominant IBS in adults • Antibiotics/Probiotics- to treat bacterial overgrowth • Tricyclic Antidepressants • Serotonic drugs- Buspar, Celexa Summary • FGIDs can occur as a well defined clinical entity (e.g. IBS) or a less defined clinical syndrome (e.g. functional abdominal pain syndrome) • Essential for physicians to take a biopsychosocial approach to diagnosis and treatment • Appreciate the close interaction of the gut and brain • Allows the child, parent and physician to address the pain on many levels • Further understanding of brain-gut axis and the role of serotonin in neural sensorimotor functions is needed Irritable Bowel Syndrome • Probiotics • Replace deficiencies of “normal” colonic bacteria and reduce fermentation • Randomized double-blind controlled trial • Lactobacillus plantarum • Reduction in the degree of flatulence • Improved overall GI function at 12 months (Am J Gastroenterol 95:1231-1238, 2000) Irritable Bowel Syndrome • Tricyclic Antidepressants • Effect significant on primary outcome measures and on global response and pain • 89% improvement in adult pts 61% remission of symptoms (Gut 2005;54:1332-1341) • Effectiveness in clinical practice limited by side effects (sleepiness) • Reserved for patients with severe symptoms or symptoms resistant to common first-line approaches Irritable Bowel Syndrome • Serotonic Agents • 5-HT1 agonists • Buspirone (Buspar) • Reduce gastric acid and colonic responses to volume distention • Anxiolytic activity • SSRIs • Citalopram (Celexa) • Reduce colonic sensation to volume distention in healthy subjects Irritable Bowel Syndrome • Psychological Treatment • Stress management • Psychotherapy • Introduce early in the discussion of pathophysiology and management of IBS • Do not leave as “last-ditch” treatment after medical therapy has proved less than optimal • Therapy often combination of parent training, altering reinforcement of various behaviors and stress management • Statistically significant improvement of pain with adjunctive cognitive-behavioral therapy (J Consult Clin Psychol 57: 294-300, 1989, and 62: 306314, 1994)