inner ear
advertisement

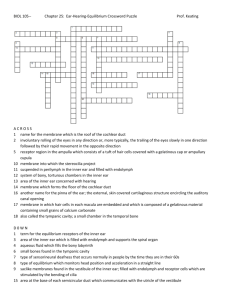
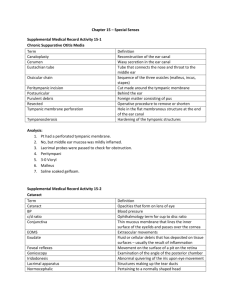
Chapter 17: The Special Senses BIO 210 Lab Instructor: Dr. Rebecca Clarke Smell (Olfaction) Olfactory Organs Provide sense of smell Located in nasal cavity on either side of nasal septum Made up of two layers Olfactory epithelium Lamina propria Figure 17–1a Smell (Olfaction) Layers of olfactory organs Olfactory epithelium contains Olfactory receptors Supporting cells Basal (stem) cells Lamina propria contains Areolar tissue Blood vessels Nerves Olfactory glands Figure 17–1a Smell (Olfaction) Smell (Olfaction) Olfactory Glands Secretions coat surfaces of olfactory organs Olfactory Receptors Highly modified neurons Olfactory reception Involves detecting dissolved chemicals as they interact with odorant-binding proteins Smell (Olfaction) Olfactory Pathways Axons leaving olfactory epithelium Collect into 20 or more bundles Penetrate cribriform plate of ethmoid Reach olfactory bulbs of cerebrum where first synapse occurs Axons leaving olfactory bulb: travel along olfactory tract to reach olfactory cortex, hypothalamus, and portions of limbic system Accessory Structures of the Eye Provide protection, lubrication, support Include: Palpebrae (eyelids) Conjunctiva (superficial epithelium) Lacrimal apparatus Accessory Structures of the Eye Figure 17–3 Palpebrae: Superior/Inferior Palpebra Continuation of skin Separated by palpebral fissure Blinking keeps surface of eye lubricated, free of dust, and debris Can close to protect delicate surface Palpebral Structures medial canthus and lateral canthus where eyelids are connected at corners of eye eyelashes Hairs that grow along margins of eyelids prevent foreign matter from reaching surface of eye (lacrimal) caruncle soft tissue mass at medial canthus contains glands thick secretions at night gritty deposits (“sand” in eyes) Tarsal (Meibomian) Glands large sebaceous glands associated with eyelashes oily product that keeps eyelids from sticking together chalazion – sty; painful, localized swelling associated with infection of tarsal gland Eyelid Muscles Orbicularis oculi – closes eyelids Levator palpebrae superioris – opens eyelids Eyelid Muscle: Levator Palpebrae Superioris Opens eyelid Eyelid Muscle: Orbicularis Oculi Closes eyelids Conjunctiva Epithelium covering: Inner surfaces of eyelids (palpebral conjunctiva) Anterior surface of eye (ocular conjunctiva) Cornea = corneal epithelium; continuous with ocular conjunctiva Figure 17–3b Fornix Pocket where palpebral conjunctiva joins ocular conjunctiva Figure 17–4a Conjunctivitis (Pinkeye) Results from damage to conjunctival surface Functions of Tears reduce friction remove debris prevent bacterial infection ( antibacterial lysozyme) provide nutrients and O2 to conjunctival epithelium + sebum (waxy secretion on hairs) “oil slick” that lubricates, slows evaporation Lacrimal Apparatus Structures that produce, distribute, and remove tears: Lacrimal gland, lake, puncta, canaliculi, sac and nasolacrimal duct Figure 17–3b Lacrimal Apparatus Tear gland: Located in: Lateral depression in frontal bone Produces tears (watery, slightly alkaline secretion, with antibacterial enzyme) Lacrimal lake: Where tears accumulate at the medial canthus Covers lacrimal caruncle Lacrimal puncta – 2 small pores that drain the lacrimal lake; empty into… Lacrimal canaliculi – small canals that lead to… Lacrimal sac – nestles in lacrimal sulcus of orbit Nasolacrimal duct – leads from lacrimal sac to nasal cavity Tears Large quantities of tears go into the nasal cavity runny nose If lacrimal puncta can’t provide enough drainage, lacrimal lake overflows and tears run down face Figure 17–3b Outer Eye: Contains 3 Layers Fibrous tunic (outer) Vascular tunic (middle) Neural tunic (inner) Figure 17–4b Outer Eye: Fibrous Tunic Structures: Sclera (white of eye) Cornea Figure 17–4b Outer Eye: Fibrous Tunic Figure 17–4c Fibrous Tunic Functions: Provides mechanical support and physical protection Serves as attachment site for extrinsic eye muscles Fibrous Tunic: Sclera dense fibrous CT that covers most of the ocular surface thinnest over anterior surface, thickest over posterior near where optic nerve exits surface contains nerves and small blood vessels ( thin red lines on opaque background) Fibrous Tunic: Cornea Transparent overlies iris and pupil structurally continuous with sclera no blood vessels; obtains nutrients and O2 from tears that wash surface numerous nerve endings so is most sensitive portion of eye Outer Eye: Vascular Tunic Structures: Choroid Ciliary body (of choroid) Iris Figure 17–4b Outer Eye: Vascular Tunic Figure 17–4c Outer Eye: Vascular Tunic Functions: Provides route for blood and lymphatic vessels that supply eye Regulates amount of light that enters eye Controls shape of lens, essential to focusing images on retina Secretes and reabsorbs aqueous humor Contains many blood vessels, lymphatic vessels and intrinsic eye muscles Vascular Tunic: Choroid covered by sclera supplies O2 and nutrients to retina Vascular Tunic: Ciliary Body Contains: Ciliary muscle - extends around outer edge of lens Ciliary processes: folds of ciliary body secrete aqueous humor Suspensory ligaments (of lens): Attach lens to ciliary processes Holds lens centered on pupil so light passing through pupil will also pass through lens Ciliary Body Figure 17–4c Ciliary Body Figure 17–8 Vascular Tunic: Iris Round, colored area visible through transparent cornea; pupil = central opening Contains: Pigment cells (melanocytes) In CT and epithelium Density and distribution determine eye color Blood vessels Pupillary muscles (smooth muscles) Pupillary Muscles Change pupil diameter (central opening of iris) when they contract and relax Controlled by ANS Pupillary Muscles Constrictor muscles (sphincter): Concentric; constrict pupil Dilator muscles: Radial; dilate/enlarge pupil Outer Eye: Neural Tunic (Retina) Consists of two layers: Pigmented part Neural part Figure 17–4b Outer Eye: Neural Tunic (Retina) Figure 17–4c Neural Tunic: Pigmented Part Thin outer layer Single layer of cells Absorbs light that passes through neural part Neural Tunic: Neural Part Thick inner layer with several layers of cells Lines posterior cavity Contains: Photoreceptors = visual (light) receptors Rods – light sensitive Cones – color sensitive Associated neurons (bipolar, horizontal, amacrine cells) Blood vessels (supply tissues that line posterior cavity) Retina Figure 17–6a Photoreceptors Not evenly distributed Optic disk: Has no photoreceptors origin of optic nerve (N II = cranial nerve II) blind spot; don’t notice because involuntary eye movements keep visual image moving (Fig 17-7 – find your blind spots) Macula lutea: concentration of cones, no rods fovea (fovea centralis) – middle of macula lutea, highest concentration of cones sharpest vision macular degeneration – age-related deterioration loss of visual field Optic Disc and Macula Lutea Figure 17–6b, c Central Retinal Artery and Vein pass through center of N II (optic nerve) emerge on surface of optic disc supply retina Optic Chiasma(a) where optic nerves crossover on way to visual cortex of occipital lobe of cerebrum (Fig 17-19) Note: brain devotes approx 35% of its power to vision! Inner Eye Eyeball is “hollow” filled with fluid or gelatinous material Divided into 2 cavities: Smaller anterior cavity Large posterior cavity Figure 17–4b Anterior Cavity Subdivided into: anterior chamber: extends from cornea to iris posterior chamber: between iris, ciliary body, and lens Filled with aqueous humor Aqueous Humor clear fluid; similar to CSF formed by epithelial cells of ciliary processes and secreted into posterior chamber passes between chambers through pupil Diffuses through anterior chamber walls into canal of Schlemm: passageway that encircles eye at level of limbus (where cornea meets sclera) delivers aqueous humor to veins of sclera Circulation of Aqueous Humor Ciliary processes posterior chamber pupil anterior chamber canal of Schlemm veins of sclera Figure 17–8 Aqueous Humor Functions: Circulation provides important route for nutrient and waste transport forms fluid cushion Intraocular Pressure fluid pressure in aqueous humor helps retain eye shape stabilizes position of retina, pressing neural part against pigmented part inadequate drainage of aqueous humor at canal of Schlemm: inc intraocular pressure = glaucoma can result in atrophy of optic nerve and blindness Posterior (Vitreous) Chamber Large chamber Filled with gelatinous mass (vitreous body/humor) Vitreous body: formed during development of eye; not replaced helps stabilize shape of eye gives additional physical support to retina Lens Lies posterior to cornea Forms anterior boundary of posterior cavity Held in place by suspensory ligaments that originate on ciliary body of choroid Primary function: to focus visual image on photoreceptors accomplished by changing shape Lens Structure Consists of concentric layers of precisely organized cells: Covered by fibrous capsule with elastic fibers Makes lens spherical when contracted Cells in center: Have no nuclei or other organelles Appear transparent Contain transparent proteins (crystallins) that clarity and focusing power of lens Cataract Abnormal, cloudy lens with reduced transparency Age-, disease-, drug-related Most common cause of blindness in adults Extrinsic Eye Muscles External muscles that rotate the eyeball Originate on surface of the eyeball 4 rectus muscles – attach straight behind the eyeball superior rectus inferior rectus medial rectus lateral rectus 2 oblique muscles – that attach from the side of the eyeball superior oblique – along medial wall, passes through trochlea (loop on medial wall of orbit) and turns laterally inferior oblique – from lateral wall of orbit, on inferior side of eyeball Extrinsic Eye Muscles Extrinsic Eye Muscles Summary: Extrinsic Eye Muscles Table 11–3 Ear Divided into 3 anatomical regions: External/outer ear Middle ear Inner ear Figure 17–20 External/Outer Ear Visible portion of ear Collects and directs sound waves toward middle ear Structures: Auricle (pinna) External acoustic/auditory canal Tympanic membrane External Ear Figure 17–20 Auricle (Pinna) Fleshy, cartilaginous flap Surrounds/protects entrance to external acoustic canal Provides directional sensitivity Blocks sound waves from behind Collected from side/front and channeled into canal External Acoustic Canal Passageway from outside to tympanic membrane (eardrum) Tympanic Membrane Thin, delicate, semitransparent sheet Separates external ear from middle ear Ceruminous Glands Integumentary glands along external acoustic canal Secrete waxy material (cerumen): With hairs projecting from canal walls, traps foreign objects Slows growth of microorganisms in canal and reduces chance of infection Middle Ear Figure 17–20 Middle Ear Separated from external ear by tympanic membrane Collects sound waves and transmits to inner ear Air-filled chamber in petrous portion of temporal bone Communicates with nasopharynx via auditory (eustachian) tube Encloses and protects 3 auditory ossicles Auditory Tube Allows equalization of pressures inside/outside tympanic membrane Also allows microorganisms to invade middle ear middle ear infection (otitis media) Auditory Ossicles Connect tympanic membrane to receptor complexes of the inner ear Convert sound waves into mechanical movements 3 tiny bones: Malleus (hammer) – attaches at 3 places on tympanic membrane; Incus (anvil) – attaches outer ossicle (malleus) to inner (stapes) Stapes (stirrup) – edges of base are bound to edges of oval window = opening in bone surrounding inner ear Note: articulations between auditory ossicles are smallest synovial joints in body Middle Ear Figure 17–21 Muscles Protect tympanic membrane and ossicles from violent movements Tensor tympani muscle: Inserts on malleus Stiffens tympanic membrane Stapedius muscle: Inserts on stapes Reduces movement of stapes at oval window Inner Ear Figure 17–20 Inner Ear Also in petrous part of temporal bone Contains sensory organs for: hearing – enables us to detect and interpret sound waves equilibrium – establishes position of head by monitoring gravity, linear acceleration, rotation Receptor mechanism same for both senses Receptors = hair cells (simple mechanoreceptors) Structures: Bony labyrinth Membranous labyrinth Maculae of Hair Cells Figure 17–23 Inner Ear: 2 Labyrinths Labyrinth = network of canals Bony labyrinth: Surrounds and protects membranous labyrinth Inner contours follow contours of membranous labyrinth Contains perilymph (similar to CSF) that flows between two labyrinths Membranous labyrinth Fluid-filled ducts and chambers inside bony labyrinth Site of sensory receptors Contains endolymph = fluid with different electrolyte concentrations than those of body Inner Ear Figure 17–22 Inner Ear: Bony Labyrinth 3 regions: Vestibule Semicircular canals Cochlea Vestibule Bony structure that encloses 2 membranous sacs: Utricle – superior, larger, nearer semicircular canals Saccule – inferior, smaller, closer to cochlea Receptors (hair cells) clustered in oval structures (maculae) Provide sensations of gravity and linear acceleration Connected with endolymphatic duct which ends in endolymphatic sac Semicircular Canals Continuous with utricle of vestibule Enclose 3 semicircular ducts Each duct has an ampulla = expanded region that contains hair cells (sensory receptors) Receptors in ducts respond to rotation of head Vestibular Complex Combination of vestibule and semicircular canals Cochlea Spiral-shaped bony chamber (“snail shell”) Size of a split pea Contains 3 ducts (parts of membranous labyrinth): Cochlear duct: spiraling central duct within cochlea; contains endolymph; suspended between… Vestibular duct: superior to cochlear duct; starts at oval window, and Tympanic duct: inferior to cochlear duct; ends at round window Vestibular and tympanic ducts interconnect at tip of cochlear spiral one long perilymphatic chamber (contains perilymph) Organ of Corti: Inside cochlear duct Contains hearing receptors Hearing Process Figure 17–29 Organ of Corti Figure 17–27 Organ of Corti Inside cochlear duct Contains hearing receptors Consists of: Vestibular membrane – separates cochlear duct from vestibular duct Basilar membrane – separates cochlear duct from tympanic duct Hair cells – hearing receptors set in rows along basilar membrane Tectorial membrane – thick membrane above hairs of hair cells; attached to inner wall of cochlea Cochlear Windows Oval window: Collagen fibers connect to stapes Round window: Thin partition that separates air space of middle ear from perilymph of cochlea Figure 17–20 Vestibulocochlear Nerves (N VIII): Vestibular Branch Carries neural information on orientation and movement of head Figure 17–25 Vestibulocochlear Nerves (N VIII): Cochlear Branch Carries neural signals for hearing Figure 17–31