Management of Chronic Endophthalmitis
advertisement

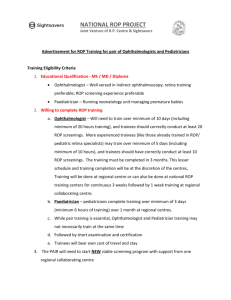
Retinopathy of Prematurity: Laser, Anti-VEGF,Surgery & Others Dr. Mangat R. Dogra Professor of Ophthalmology Advanced Eye Centre PGIMER, Chandigarh No financial disclosure Introduction Retinopathy of prematurity (ROP) is the leading cause of childhood blindness worldwide. Becoming a major public health concern in developing countries like India. (New and emerging cause of blindness) Blindness due to ROP is potentially preventable. A large number of babies in our country are presenting late with bilateral, irreversible blindness due to absence or delayed screening. Predicting ROP blindness according to Infant mortality rates. Gilbert C. Early Hum Dev 2008;84 (2):77-82. ROP in India Incidence of ROP: 38% – 47. 3 % in low birth weight infants. – – Charan R, Dogra MR, Gupta A, Narang A. Indian J Ophthalmol 1995; 43:123-26. Gopal L et al. Indian J Ophthalmol 1995; 43:50-61. Live births: 26 million /year Incidence of Low birth weight (< 2000g)- 8.7% 2 million newborns are at risk for developing ROP. National Neonatalogy Forum of India. National Neonatal Perinatal Database. Report New Delhi 2005 Indian scenario of ROP 1995 : Charan R ,Dogra MR et al IJO 43:123-126;1995 first prospective study (<1700g) incidence of 47.27% 1995 : Gopal etal ; (<2000g) 38% 1996 : Rekha etal ; (<1500g) 47.3% 1996 : Maheshwari etal; (<1500g) 20% 2001 : Varughese etal; (<1500g) 51.89% 2009 : Chaudhari etal; (<1500g) 22.30% 2012 : Hungi B etal; (<2000g) 41.5% Implications for screening The American screening guidelines Babies ≤ 1500 g birth weight or ≤ 30 weeks gestational age Selected infants with a birth weight 1500 -2000 g or gestational age > 30 weeks be screened at the discretion of the attending neonatologist. Pediatrics 2013;131(2) Indian Screening guidelines Infants weighing < 1750 grams or < 34 weeks of gestation. Heavier (1750-2000g) or older babies (34-36 weeks) may be screened depending upon the attending risk factors like mechanical ventilation, prolonged oxygen therapy, hemodynamic instability or adverse respiratory or cardiac disease profile. National neonatology forum. Clinical practice guidelines 2010. Why screen for ROP Premature child is not born with ROP Screening aims to identify treatable stage Narrow window for screening and treatment Delay cause blindness or visual impairment Medico-legal implications Economic and social burden of childhood blindness is immense Aggressive Posterior ROP The keys to diagnosis: Identification of plus disease Location in zone 1 or posterior zone 2 Subtle neovascular findings at the junction without any stages of ROP These cases progress rapidly and directly to retinal detachment . ICROP revisited: Arch Ophthalmol.2005;1239:991-99 Sanghi G, Dogra MR et al .Aggressive posterior retinopathy of prematurity in Asian Indian babies:Spectrum of Disease and Outcome After Laser Treatment. Retina 2009:29;1335-39 Jalali S, Kesarwani S, Hussain A. Outcomes of a protocol-based management for zone 1 retinopathy of prematurity: the Indian Twin Cities ROP Screening Program report number 2. Am J Ophthalmol. 2011 Apr;151(4):719-724 Shah PK, Narendran V, Kalpana N Aggressive posterior retinopathy of prematurity in large preterm babies in South India. Arch Dis Child Fetal Neonatal Ed. 2012 Sep;97(5):F371-5. The mean birth weight and gestational age in APROP Author year Country Mean Birth weight (g) Mean gestational age (wk) Jalali et al 2011 India 1228 29.63 Drenser et al 2010 USA 627 24.3 Sanghi et al 2009 India 1259 29.75 Azuma et al 2006 Japan 773 25 Shah et al 2012 India 1572 31.7 Current treatments of ROP Peripheral retinal ablation with laser delivered through laser indirect ophthalmoscope (LIO) is a gold standard in ROP treatment Anti-VEGF is emerging therapy for selective cases of ROP Vitreoretinal surgery is required in stage 4 and 5 ROP Rationale for laser treatment VEGF is stimulus for abnormal vessels which comes from avascular retina Ablate the avascular retina between ora and ridge to reduce VEGF Laser Treatment of ROP Laser treatment earlier than threshold ROP has shown better results & outcome after ETROP Study Arch Ophthalmol.121:1684-1696; 2003 ETROP Recommendations Arch Ophthalmol. 121:1684-96;2003 Z o n e No Plus 1 Plus Z o n e No Plus 2 Plus Stage 1 Follow Stage 2 Follow Stage 3 Treat Stage 1 Treat Stage 2 Treat Stage 3 Treat Stage 1 Follow Stage 2 Follow Stage 3 Follow Stage 1 Follow Stage 2 Treat Stage 3 Treat Plus disease If pupil does not dilate suspect tunica vasculosa lentils and plus disease. Plus disease Plus disease means at least 2 quadrants of dilation and tortuosity of the posterior retinal blood vessels Preplus & Plus disease Laser treatment Delivered in confluent pattern (less than half burn width apart) Around 90% attain favourable outcome Laser treatment for ROP: evolution in treatment technique over 15years Hurley et al. Retina 26: S16-7; 2006 Laser treatment Possible inside the incubator through the slopping transparent wall in extremely unstable premature infants Dogra etal Ophthalmic Surg Lasers Imaging 39:350-352;2008 Frequency doubled Nd: YAG (532 nm green) versus diode laser (810 nm) in treatment of ROP Favorable outcome in 97% with 532 nm laser versus 96.9% in diode laser group. Treatment possible in eyes with TVL, vitreous or preretinal hemorrhage and without inducing any cataract, anterior segment ischemia or hyphema . Sanghi G, Dogra MR, Vinekar A,Gupta A. Frequency doubled Nd: YAG (532 nm green) vs diode laser(810 nm ) in treatment of retinopathy of prematurity Br J Ophthalmol 94;1265-1265 : 2010 Laser treatment of APROP Delivered through LIO in confluent pattern (less than half burn width apart) with in 24-48 hours of diagnosis Around 55% to 84% attain favourable outcome in reported series Sanghi G, Dogra M R et al. Aggressive posterior retinopathy of prematurity in Asian Indian babies:Spectrum of Disease and Outcome After Laser Treatment. Retina 2009:29;1335-39 APROP in posterior zone 1 with mat like proliferation Unfavourable outcome after laser Risk factors for RD after laser treatment of APROP Gestational age less than 29 weeks Posterior zone 1 APROP Pre-retinal hemorrhages Need for repeat laser treatment New onset fibrovascular proliferation after laser treatment Sanghi G, Dogra M R et al.Aggressive posterior retinopathy of prematurity: risk factors for RD despite confluent laser photocoagulation. Am J Ophthalmol. 2013: Jan;155(1):159-164 Indications for ROP surgery Progression despite laser treatment Delayed or no screening Stage 4A, 4b and stage 5 ROP Bilateral cases Current surgical approaches in ROP Scleral buckle is rarely performed Lens sparing vitrectomy Lensectomy & vitrectomy Management of stage 4A and 4B ROP ? Observation if < 4 clock hrs of elevation Lens sparing vitrectomy has shown reattachment in 60 % to 85% eyes Bende P, Gopal L et al. Indian J Ophthalmol 57:267-271;2009 Lakhanpal et al. Arch Ophthalmol 124: 675-679;2006 Capone A Jr, Trese MT. Ophthalmology 108:2068-2070;2001 Lens sparing vitrectomy (LSV) Most important recent innovation Ideal for stage 4A and 4B ROP Both 2 or 3 port LSV is possible 23G and 25G LSV are preferred at present ROP stage 5 : Total retinal detachment Management of stage 5 ROP Lensectomy and vitrectomy in these cases Reattachment in some eyes (< 1/3) Functional results extremly poor and dismal ETROP Study results: Arch Ophthalmol 124;24-30:2006 Arch Ophthalmol 129;1175-1179:2011 Shah et al. Eye 23;176-180:2009 Gopal et al. IJO 48:101-106; 2000 Bevacizumab monotherapy Avastin monotherapy showed a significant benefit for zone 1 but not for zone 2 ROP as compared to conventional laser therapy. Trial was too small to assess safety issue. Mintz-Hittner et al. N Engl J Med 2011; 364:603-15 Avastin in ROP Caution is warranted for routine use at this time due to safety issues. 0.625mg in 0.025ml of intravitreal avastin is usually given. Mostly used as rescue therapy in zone 1 ROP along with laser Increasing ROP blindness in India High rate of preterm birth Neonatal care not optimal ROP screening and treatment programs not in place Inadequate treatment and follow up Increasing numbers of NICUs and SNCUs SNCUs Sick Newborn Care Units District level Provide newborn care to decrease mortality Potential sources for ROP in the coming years ROP Stage 5 86.4% of infants presenting with stage 5 ROP were never screened 74.2% were picked up by the parents when they noticed that child is not seeing. Pediatricians referred none 25.8% referred by an ophthalmologist. – Sanghi G, Dogra MR, Katoch D, Gupta A. Demographic profile of infants with stage 5 retinopathy of prematurity in North India: implications for screening. Ophthalmic Epidemiol 2011;18(2):72-4. Prevailing clinical practices among pediatricians Only 14.5% were following the recommendations ROP referral. – for Patwardhan SD, Azad R, Gogia V, Chandra P, Gupta S. Prevailing clinical practices regarding screening for retinopathy of prematurity among pediatricians in India: a pilot survey. Indian J Ophthalmol 2011;59(6):427-30. Role of neonatologist and / or pediatrician Prevention of ROP ROP screening During ROP treatment / surgery Follow up of cases Prevention of ROP Prevention of prematurity Good antenatal and obstetrics care 1.Use of antenatal steroids 2.Trained personal in delivery room to avoid asphyxia Judicious use of oxygen therapy and ventilation Reduce morbidity of premature infants ROP screening Single nodal person to be identified Communicate with parents and ophthalmologist Identify babies and decide time for screening Combine ROP screening visit with follow up for neonatal problems Record keeping is most important During laser therapy Monitoring during therapy Counseling Resuscitation What should be done Wall chart regarding whom to screen, when to screen and how to dilate should be pasted in NICU and Nursery What should be done Any one weighing the new born infant should paste a bold sticker on card / file for ROP screening in babies < 1750gms at birth in 3 to 4 weeks. Responsibility is of Obstetrician / Pediatrician / nurses to get ROP screening done from Ophthalmologist at appropriate time A novel, low-cost method of enrolling infants at risk for Retinopathy of Prematurity in centers with no screening program: the REDROP study. Vinekar A, Avadhani K, Dogra M, Sharma P, Gilbert C, Braganza S, Shetty B. Ophthalmic Epidemiol. 2012 Oct;19(5):317-21 Goals of an ROP workshop Define criteria for identification of babies at risk with birth weight and gestational age Develop programs for prevention, detection and treatment of ROP Develop teams at NICUs with no program Prepare action plan for prevention of ROP Stimulate government participation Conclusions Lack of awareness about ROP in India Neonatal care and screening program are variable not optimal More mature and higher birth weight babies are developing ROP Delayed or no screening responsible for increasing rates of childhood blindness due to ROP in India Conclusions Treat ROP as per ETROP Study recommendations & with APROP promptly with confluent laser Use anti-VEGF as rescue therapy. Lens sparing vitrectomy is the most important recent exciting innovation for stage 4A and 4B. Lensectomy and vitrectomy in complex cases usually results in poor outcome. ROP prevention, screening and management is a team effort India THANK YOU