PERSIST-1 Phase III Oral Abstract slides
advertisement

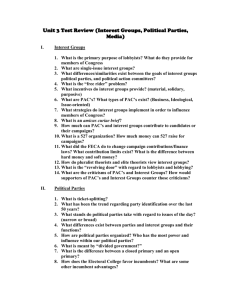
Results of the PERSIST-1 phase III study of pacritinib (PAC) versus best available therapy (BAT) in primary myelofibrosis (PMF), post-polycythemia vera myelofibrosis (PPV-MF), or post-essential thrombocythemia-myelofibrosis (PET-MF) Ruben A. Mesa,1 Miklos Egyed,2 Anita Szoke,3 Aleksandr Suvorov,4 Andrew Perkins,5 Jiri Mayer,6 Peter Ganly,7 Eric Jourdan,8 Harry C. Schouten,9 Patrizia Tosi,10 Charles Michael Farber,11 Pierre Zachee,12 Christof Scheid,13 James P. Dean,14 Paul Cernohous,14 Jyoti Nangalia,15 Jean-Jacques Kiladjian,16 Alessandro M. Vannucchi,17 Adam Mead,18 Claire N. Harrison19 1Mayo Clinic, Scottsdale, AZ; 2Kaposi Mor Teaching Hospital, Kaposvar, Hungary; 3lbert Szent-Györgyi Clinical Center, Universisty of Szeged, Szeged, Hungary; 4First Republican Clinical Hospital of Udmurtia, Izhevsk, Russia; 5ICON Cancer Care, Brisbane, Australia; 6University Hospital Brno, Brno, Czech Republic; 7Christchurch Hospital, Christchurch, New Zealand; 8Centre Hospitalier Universitaire de Nîmes, Nîmes, France; 9University Hosp Maastricht, Maastricht, Netherlands; 10Ospedale "Infermi", Rimini, Rimini, Italy; 11Morristown Memorial Hospital, Carol G. Simon Cancer Center, Morristown, NJ; 12ZNA Stuivenberg, Antwerp, Belgium; 13University of Cologne, Cologne, Germany; 14CTI BioPharma Corp., Seattle, WA; 15Cambridge Institute for Medical Research, Cambridge, United Kingdom; 16Hôpital Saint-Louis and Paris Diderot University, Paris, France; 17University of Florence, Florence, Italy; 18Oxford University Hospitals, Oxford, United Kingdom; 19Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom Disclosures • Employment – No relationships to disclose • Leadership – No relationships to disclose • Stock and other ownership interests – No relationships to disclose • Honoraria – Novartis Healthcare A/S • Consulting or advisory role – No relationships to disclose • Speakers’ bureau – No relationships to disclose • Research funding – CTI, Incyte, Gilead, Promedior, Genentech, Pharmessentia, Pfizer • Patents, royalties, and other intellectual property – No relationships to disclose • Expert testimony – No relationships to disclose • Travel, accommodations and expenses – No relationships to disclose • Other relationship – No relationships to disclose Background • Myelofibrosis is a rare hematologic malignancy, the symptoms of which have a substantial negative impact on both patient quality of life and overall survival1-3 • As early as 1 year from the time of diagnosis, the incidence of diseaserelated thrombocytopenia, anemia, and RBC transfusion requirements increase dramatically4 • Thrombocytopenia is a prognostic factor for shorter overall survival and risk of leukemic transformation5 • Current treatments have not demonstrated the ability to simultaneously improve splenomegaly, symptoms, and cytopenias in myelofibrosis patients RBC, red blood cell. 1. Tefferi A, et al. Blood. 2013;122:1395-1398. 2. Mesa RA, et al. Cancer. 2007;109:68-76. 3. Geyer HL, et al. Blood. 2014;124:3529-3537. 4. Tefferi A, et al. Mayo Clin Proc. 2012;87:25-33. 5. Gangat N, et al. J Clin Oncol. 2010;29:392-397. Pacritinib A Selective JAK2/FLT3 Inhibitor Not associated with clinically significant treatment-emergent anemia or thrombocytopenia in clinical studies1 Kinase JAK1 IC50 (nM) 1280 JAK2wt 6.0 JAK2V617F 9.4 JAK3 18.3 TYK2 27.0 FLT3-ITD 13.4 FLT3D835Y 4.7 CSF1R 39.5 IRAK1 13.6 CSF1R, colony stimulating factor 1 receptor; FLT, FMS-like tyrosine kinase; IC50, half-maximal inhibitory concentration; IRAK1, interleukin-1 receptor–associated kinase; ITD, internal tandem duplication; JAK, Janus kinase; TYK, tyrosine kinase. 1. William AD, et al. J Med Chem. 2011;54:4638-465. 2. Hart S, et al. Leukemia. 2011;25:1751-1759. PERSIST-1 Study Design Key Eligibility Criteria PMF, PET-MF, or PPV-MF Pacritinib 400 mg qd Intermediate- or high-risk disease Palpable spleen ≥5 cm No exclusion for baseline platelet levels; stratified for platelet counts <100,000/µL and <50,000/µL R (2:1) N=327 Best Available Therapy (BAT)a No exclusion for baseline Hgb levels No prior treatment with JAK2 inhibitors excluding ruxolitinib a Cross-over from BAT allowed after progression or after Week 24 assessment • Stratification at randomization: platelet count, risk category, and region • Study endpoints • Primary: proportion of patients achieving a ≥35% reduction in spleen volume • (by MRI/CT) from baseline to Week 24 Secondary: proportion of patients with ≥50% reduction in TSS from baseline to Week 24 on the Myeloproliferative Neoplasm Symptom Assessment Form CT, computed tomography; Hgb, hemoglobin JAK, Janus kinase; MRI, magnetic resonance imaging; PET-MF, post-essential thrombocythemia myelofibrosis; PMF, primary myelofibrosis; PPV-MF, post-polycythemia vera myelofibrosis; R, randomized; TSS, total symptom score. Patient Dispositiona Median Follow-up: 8.4 months (Range, 0.1-22.2) Randomized 2:1 PAC (ITT) n=220 BAT (ITT) n=107 PAC (Safety) n=220 BAT (Safety) n=106 Discontinued: n=96 (44%) Adverse event: n=32 (15%) Patient withdrawal: n=28 (13%) Investigator decision: n=16 (7%) Progressive disease: n=10 (5%) Death: n=3 (1%) Other: n=7 (3%) Ongoing n=124 (56%) a As of data cut off: Jan 17, 2015. BAT, best available therapy; ITT, intent-to-treat; PAC, pacritinib. Discontinued: n=98 (92%) Adverse event: n=3 (3%) Patient withdrawal: n=3 (3%) Investigator decision: n=78 (73%) Progressive disease: n=12 (11%) Death: n=1 (1%) Non-compliance: n=1 (1%) Crossed over to PAC n=85 (79%) Ongoing n=9 (8%) Baseline Characteristics Characteristic Median age, years (range) ≥65 years, n (%) Male, n (%) ECOG PS, n (%) 0-1 2-3 MF diagnosis, n (%) Primary MF Post-polycythemia vera MF Post-essential thrombocythemia MF IPSS score, n (%)a Int-1 Int-2 High Median spleen length by physical exam, cm (range)b Median spleen volume by MRI/CT, cm3 (range)c JAK2V617F positive, n (%) a Derived PAC (n=220) 67 (23-87) 135 (61) 125 (57) BAT (n=107) 65 (37-84) 55 (51) 60 (56) 191 29 (87) (13) 96 11 (90) (10) 144 48 27 (65) (22) (12) 59 33 15 (55) (31) (14) 30 76 106 12 2223 154 (14) (35) (48) (4-33) (472-7948) (70) 18 35 51 12 2367 92 (17) (33) (48) (4-30) (436-5404) (86) from central laboratory data; b n=219 for PAC, n=106 for BAT; c n=218 for PAC, n=107 for BAT. BAT, best available therapy; CT, computed tomography; ECOG PS, Eastern Cooperative Oncology Group performance status; Int, intermediate; IPSS, International Prognostic Scoring System; JAK, Janus kinase; MF, myelofibrosis; MRI, magnetic resonance imaging; PAC, pacritinib. Baseline Characteristics Hematology Characteristic BM biopsy completed, n (%) Reticulin and collagen fibrosis staging MF 0-1 MF 2-3 Missing Peripheral blasts, n (%) <1% ≥1% <5% ≥5% Missing White blood cell count, n (%) ≤25 ×109/L >25 ×109/L Hemoglobin, n (%) <10 g/dL ≥10 g/dL Platelet count, n (%) <50,000/μL ≥50,000 to <100,000/μL ≥100,000/μL BAT, best available therapy; BM, bone marrow; Hgb, hemoglobin; MF, myelofibrosis; PAC, pacritinib. PAC (n=220) 219 (100) BAT (n=107) 107 (100) 32 180 7 (15) (82) (3) 18 83 6 (17) (78) (6) 78 94 (35) (43) 44 38 (41) (36) 159 13 48 (72) (6) (22) 74 8 25 (69) (7) (23) 177 43 (80) (20) 80 26 (75) (24) 84 136 (38) (62) 47 59 (44) (55) 35 37 148 (16) (17) (67) 16 18 73 (15) (17) (68) BAT Treatment WHO Drug Term, n (%) BAT (n=107) Watch and wait (no active Tx) 27 (25.5) Hydroxycarbamide Prednisone Interferon alfa Thalidomide Danazol Prednisolone Busulfan Cytarabine Peginterferon alfa-2a 59 (55.7) 7 (6.6) 6 (5.7) 6 (5.7) 4 (3.8) 4 (3.8) 2 (1.9) 2 (1.9) 2 (1.9) BAT, best available therapy; Tx, treatment. WHO Drug Term, n (%) Anagrelide Azacitidine Epoetin alfa Epoetin theta Everolimus Lenalidomide Mercaptopurine Methotrexate Vincristine BAT (n=107) 1 1 1 1 1 1 1 1 1 (0.9) (0.9) (0.9) (0.9) (0.9) (0.9) (0.9) (0.9) (0.9) Spleen Volume Reduction ≥35% At Week 24 as Assessed by MRI/CT Change From Baseline, % • ITT population: 19.1% vs 4.7%, PAC vs BAT (p=0.0003) • Evaluablea population: 25.0% vs 5.9%, PAC vs BAT (p=0.0001) a 60 50 40 30 20 10 0 -10 -20 -30 -40 -50 -60 -70 -80 -90 -100 PAC (n=168) BAT (n=85) 35% decrease Patientsa Evaluable Population: patients had both baseline and Week 24 spleen assessment by MRI or CT; n=168 for PAC and n=85 for BAT. BAT, best available therapy; CT, computed tomography; ITT, intent to treat; MRI, magnetic resonance imaging; PAC, pacritinib. Spleen Volume Reduction ≥35% Patients With Baseline Thrombocytopenia ITT PAC Evaluablea BAT p=0.0370 40% 33.3% Patients p=0.0451 30% p=0.0072 p=0.0086 22.9% 20% 23.5% 16.7% 10% 0% 0% <50,000/μL a 0% 0% <100,000/μL <50,000/μL Patients had both baseline and Week 24 spleen assessment by MRI or CT; n=168 for PAC and n=85 for BAT. BAT, best available therapy; CT, computed tomography; ITT, intent to treat; MRI, magnetic resonance imaging; PAC, pacritinib. 0% <100,000/μL Correlation of SVR With OS By Treatment Landmark Analysis at Week 24 Hazard Ratio (95% CI)a p-value ≥10% to <20% (n=37) 0.15 (0.02, 1.18) 0.071 ≥20% (n=98) 0.26 (0.09, 0.76) 0.014 2.31 (0.50, 10.81) 0.287 NA NA SVR Pacritinib BAT ≥10% to <20% (n=5) ≥20% (n=11) a Reference to < 10% SVR as assessed by MRI/CT. BAT, best available therapy; CT, computed tomography; MRI, magnetic resonance imaging; NA, not applicable; OS, overall survival; SVR, spleen volume reduction. Patients Achieving ≥50% Reduction in TSSa At Week 24 (ITT Populationb) PAC 30% Patients 25% BAT p<0.0001 24.5% p=0.4086 p=0.0677 p=0.0004 25.0% 24.3% 20.0% 20% 15% 10% 8.8% 6.5% 6.3% 5.5% 5% 0% All Patients a <50,000/μL TSS and TSS 2.0 combined; b n=220 for PAC and n=107 for BAT. BAT, best available therapy; ITT, intent to treat; PAC, pacritinib; TSS, total symptom score. <100,000/μL ≥100,000/μL Platelet Subgroup Patients Achieving ≥50% Reduction in TSSa At Week 24 (Evaluable Populationb) PAC 50% BAT p=0.0790 p<0.0001 41.9% 40.4% p<0.0001 40.9% p=0.3791 Patients 40% 31.8% 30% 16.7% 20% 10% 9.9% 11.1% 7.5% 0% All Patients <50,000/μL <100,000/μL ≥100,000/μL Platelet Subgroup a TSS and TSS 2.0 combined; b Patients had both baseline and Week 24 TSS value; n=132 for PAC and n=71 for BAT. BAT, best available therapy; PAC, pacritinib; TSS, total symptom score. Patients Achieving ≥50% Reduction in TSS Reduction Over Time (Evaluable Populationa) PAC BAT Patients with ≥50% Reduction in Total Symptom Score, % 50 45 40 35 30 25 20 15 10 5 0 1 a 4 8 Patients had both baseline and the corresponding post-baseline TSS value. BAT, best available therapy; ITT, intent to treat; TSS, total symptom score. 12 Weeks 16 20 24 Mean Change From Baseline, % Mean % Change in Body Weight Over Time 2.5 PAC 2 BAT 1.5 1 0.5 0 -0.5 Baseline BAT, best available therapy; PAC, pacritinib. 4 8 12 16 Weeks 20 24 36 Hemoglobin Over Time By Central Laboratory Mean % Change in Hgb (± SEM) Mean Hgb (g/dL) (± SEM) 10 PAC BAT 80 Mean Hgb (g/dL) (± SEM) Mean % Change in Hgb (± SEM) 100 60 40 20 0 PAC BAT 9.5 9 8.5 8 -20 BL 3 4 8 12 Weeks 16 20 24 BL Safety Population BAT, best available therapy; BL, baseline; Hgb, hemoglobin; SEM, standard error of the mean. 3 4 8 12 16 Weeks Patients With Baseline Hgb <10 g/dL 20 24 Platelets Over Time By Central Laboratory Mean Platelets×109/L (± SEM) Mean % Change Platelets (± SEM) 60 PAC BAT Mean Platelets×109/L (± SEM) Mean % Change Platelets (± SEM) 100 80 60 40 20 0 -20 50 p=0.0034a 40 30 20 p=0.1927a 10 0 BL 3 4 8 12 16 20 24 Weeks Safety Population a PAC BAT Based on linear regression using mixed model. BAT, best available therapy; BL, baseline; PAC, pacritinib; SEM, standard error of the mean. BL 3 4 8 12 16 Weeks Patients With Baseline Platelets <50,000/μL 20 24 RBC Transfusion Independence • At baseline, 15.9% PAC and 14.0% BAT patients were RBC transfusion dependent, per Gale criteriaa Patients Achieving Transfusion Independence p=0.043 30% 25.7% Patients 25% PAC BAT 20% 15% 10% 5% 0% ≥ 6units/90 days. BAT, best available therapy; PAC, pacritinib; RBC, red blood cell. a 0% Most Common Adverse Events Within 24 Weeks (by Investigator) All Grades Adverse Event, n (%) PAC (n=220) BAT (n=106) Grade 3 PAC (n=220) Grade 4 BAT (n=106) PAC (n=220) BAT (n=106) Non-hematologic (>10%) Diarrhea 117 (53.2) 13 (12.3) 11 (5.0) 0 0 0 Nausea 59 (26.8) 7 (6.6) 2 (0.9) 0 0 0 Vomiting 35 (15.9) 6 (5.7) 2 (0.9) 0 0 0 Peripheral edema 16 (7.3) 12 (11.3) 1 (0.5) 1 (0.9) 0 0 Pyrexia 11 (5.0) 11 (10.4) 4 (1.8) 1 (0.9) 0 0 Anemia 49 (22.3) 21 (19.8) 32 (14.5) 13 (12.3) 5 (2.3) 3 (2.8) Thrombocytopenia 37 (16.8) 14 (13.2) 12 (5.5) 7 (6.6) 14 (6.4) 3 (2.8) 8 (3.6) 2 (1.9) 1 (0.5) 1 (0.9) 4 (1.8) 1 (0.9) Hematologic (>2%) Neutropenia • 10% of patients in the PAC arm had dose reductions due to AE (3% diarrhea; 2% anemia) AE, adverse event; BAT, best available therapy; PAC, pacritinib. Side Effects of Interest Gastrointestinal • Majority of cases occur within the first 2 weeks • Benefit (SVR, TSS) preserved irrespective of any gastrointestinal side effects • More frequent in patients aged >65 years and patients with platelets <100,000/μL • Diarrhea resolves in a little over 1 week irrespective of grade with antimotility agents • Diarrhea resulted in discontinuation or dose interruption (average 1 week) in only 3 and 13 patients, respectively SVR, spleen volume reduction; TSS, total symptom score. Conclusions • Significantly greater proportion of patients with ≥35% reduction of spleen volume, regardless of baseline platelet count (p=0.0003) • Significant treatment effect (p<0.05) in highest-risk subset (baseline platelets <50,000/μL) • Significant reduction in TSS (p<0.0001) • Significantly higher proportion of patients became RBC transfusion independent (p<0.05) • Patients with baseline platelets <50,000/μL had mean increase in platelet counts of 35% by Week 24 • Based on preliminary data, pacritinib may be disease modifying and warrants combination studies with other potentially disease-modifying agents in MPNs MPN, myeloproliferative neoplasm; RBC, red blood cell; TSS, total symptom score. PERSIST-2 Study Design Pacritinib 400 mg qd Eligibility Criteria Patients with platelet counts ≤ 100,000/µL, prior/current JAK2 therapy allowed 1:1:1 Randomizationa N=300 Pacritinib 200 mg bid Best available therapy (BAT)b Status: reached agreement with FDA on SPA October 2013 Sites: North America, Europe, Russia, and Oceania Anticipated patient accrual: ~ 300 Principal investigator: Srdan Verstovsek a Crossover b BAT from BAT allowed after progression or assessment of the primary endpoint. may include ruxolitinib at the approved dose for platelet count CT, computed tomography; JAK, Janus kinase; MRI, magnetic resonance imaging; TSS, total symptom score. Co-Primary Endpoints % of patients achieving ≥35% reduction in spleen volume from baseline to Week 24 (MRI/CT) Patients achieving ≥50% reduction in TSS from baseline to Week 24 Acknowledgments • We would like to thank all the patients, investigators, and personnel who contributed to this study • Medical editorial assistance funded by CTI Biopharma Corporation was provided by Nexus Global Group Science, LLC