system 4
advertisement

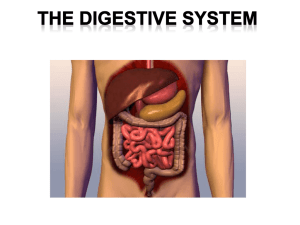
Human Digestive System Digestive System is divided to 1- Gastrointestinal tract and accessory organs A. Gastrointestinal Tract 1. Also known as "alimentary canal" 2. All organs through which food passes (mouth to anus) B. Accessory Structures 1. Assist in digestion 2. Includes teeth, tongue, salivary glands, liver, gall bladder, pancreas. 1 The gastrointestinal tract (GIT) consists of a hollow muscular tube starting from the oral cavity, where food enters the mouth, continuing through the pharynx, esophagus, stomach and intestines to the rectum and anus, where feaces is expelled. 2 Accessory organs : assist the tract mechanically or by secreting enzymes to help break down food into its component nutrients. Food is never found within the accessory organs, only within the tract itself. 3 A diet must supply chemical energy, organic molecules, and essential nutrients • A diet provides: – Chemical energy, which is converted into ATP to power cellular processes. – Organic building blocks, such as organic carbon and organic nitrogen, to synthesize a variety of organic molecules. – Essential nutrients (essential amino acids, essential fatty acids, vitamins & minerals), which are required by cells and must be obtained from dietary sources. •Ingestion Taking food into the mouth. •Mastication: •Peristalsis •Deglutition Functions of the GI Tract 1-Motility: – Movement of food through the GI tract. • Ingestion: – Taking food into the mouth. • Mastication: – Chewing the food and mixing it with saliva. • Deglutition: – Swallowing the food. • Peristalsis: – Rhythmic wave-like contractions that move food through GI tract. – Valves called sphincters regulate the movement of material between compartments Functions of the GI Tract (continued) • 2-Secretion: – Includes both exocrine and endocrine secretions. • Exocrine: – Hydrochloric acid (HCl), Water, (H2O), bicarbonate (HCO3-) , bile, Digestive Enzymes (lipase, pepsin, amylase, trypsin, and elastase), are secreted into the lumen of the GI tract. • Endocrine: – Stomach and small intestine secrete hormones to help regulate the GI system. » Gastrin, secretin, CCK (cholecystokinin), GIP (gastric inhibitory peptide), GLP-1 (glycogen-like peptide-1), guanylin, VIP (vasoactive intestinal peptides), and somatostatin. Functions of the GI Tract (continued) • 3-Digestion is the process of breaking food down into molecules small enough to be absorbed. digestion is an extracellular process that occurs mainly in the stomach and small intestine where proteins, fats and carbohydrates are chemically broken down into their basic building blocks. It is of 2 types: • A-Mechanical digestion, including chewing, which increases the surface area of food • B-Chemical digestion splits food into small molecules that can pass through membranes; these are used to build larger molecules • In chemical digestion, the process of enzymatic hydrolysis splits bonds in molecules with the addition of water • 4-Absorption: – Process of the passage of digested end products (chemical subunits) into the blood or lymph. – Smaller molecules are absorbed across the epithelium of the small intestine and subsequently enter the circulation. – The large intestine plays a key role in reabsorbing excess water. • 5-Storage and elimination: – Temporary storage and elimination of indigestible material out of the digestive system. – undigested material and secreted waste products, bacteria, unabsorbed digested material, cells sloughed from the GI tract are excreted from the body via defecation (passing of faeces). •Esophagus Layers of the GI 1- Mucosa • Lines the lumen of GI tract. – Depending on its function, the epithelium may be simple columnar epithelium or stratified (multiple layers). • Lamina propria: – Thin layer of connective tissue containing lymph nodules. • Muscularis mucosae: – Thin layer of smooth muscle responsible for the folds. – Folds increase surface area for absorption. • Goblet cells: – Secrete mucus. Mucosa’s functions are 1- Secrets mucus, digestive enzyme, and hormones. 2-Absorption of the end products of digestion into the blood 3- Protection against infectious diseases (lymph nodes 2-Submucosa • Thick, highly vascular layer of connective tissue. • Absorbed molecules enter the blood and lymphatic vessels. • Submucosal plexus (Meissner’s plexus): – Provide autonomic nerve supply to the muscularis mucosae. 3-Muscularis • Responsible for segmental contractions and peristaltic movement through the GI tract. –Inner circular layer and outer longitudinal layer of smooth muscle. • Contractions of these layers move food through the tract; mix the food. • Myenteric plexus (Auerbach’s) located between the 2 muscle layers. –Major nerve supply to GI tract. •Fibers and ganglia from both sympathetic and parasympathetic nervous systems. 4-Serosa / or Adventitia • Binding and protective outer layer. • Consists of areolar connective tissue covered with simple squamous epithelium. Layers of the gastrointestinal tract Copyright 2009, John Wiley & Sons, Inc. Neural innervation • Enteric nervous system (ENS) – Intrinsic set of nerves - “brain of gut” – Intrinsic sensory neurons which form network within the walls of the gut from esophagus to anus – 2 plexuses • Myenteric plexus – GI tract motility • Submucosal plexus – controlling secretions • Autonomic nervous system – Extrinsic set of nerves – Parasympathetic stimulation: Vagus and sacral spinal nerves increase GI secretions and activity by stimulating ENS – Sympathetic stimulation decreases secretions and activity by inhibiting ENS From Mouth to Stomach The first stage of digestion is mechanical that takes place in the oral cavity. It includes: • Mastication (chewing): – Mixes food with saliva which contains salivary amylase. • Salivary glands deliver saliva to lubricate food • Teeth chew food into smaller particles that are exposed to salivary amylase, an enzyme that can catalyze the partial digestion of starch. • Saliva also contains mucus, a viscous mixture of water, salts, cells, Antimicrobial agents and glycoproteins. • • • • • The tongue shapes food into a bolus and provides help with swallowing The throat, or pharynx, is the junction that opens to both the esophagus and the trachea The esophagus conducts food from the pharynx down to the stomach by peristalsis Swallowing causes the epiglottis to block entry to the trachea Coughing occurs when the swallowing reflex fails and food or liquids reach the windpipe. From Mouth to Stomach • Deglutition (swallowing): – Begins as a voluntary activity. – Involves 3 phases: • Oral phase is voluntary. • Pharyngeal and esophageal phases are involuntary (autonomic) and controlled by the swallowing center in the medulla. So, it cannot be stopped. – – – – • (continued) During swallowing Soft palate lifts to close off the nasopharynx Larynx is raised and vocal cords close off the opening to the larynx. Epiglottis covers the entrance to respiratory tract. The upper esophageal sphincter relaxes. Esophagus: – Connects pharynx to the stomach. • Upper third contains skeletal muscle. • Middle third contains a mixture of skeletal and smooth muscle. • Terminal portion contains only smooth muscle. Esophagus • Peristalsis: Wave-like muscular contractions: – Circular smooth muscles contract behind, relaxe in front of the bolus. – Followed by longitudinal contraction (shortening passage way ahead of the bolus) of smooth muscle. • Rate of 2-4 cm/sec. – After food passes into stomach, lower esophageal sphincter constricts. Insert 18.4a Figure 41.10-3 Tongue Bolus of food Pharynx Epiglottis up Glottis Larynx Trachea Esophageal sphincter contracted Esophagus To lungs To stomach Relaxed muscles Contracted muscles Sphincter relaxed Stomach Stomach • Most distensible part of GI tract. – Empties into the duodenum. • Functions of the stomach: – Stores food. – Initiates digestion of proteins. – Kills bacteria. – Moves food (chyme) into intestine. • Contractions of the stomach churn chyme. – Mix chyme with gastric secretions. – Push food into intestine. • Gastric mucosa has gastric pits in the folds. Figure 41.11 Esophagus Sphincter Stomach 10 m Sphincter Gastric pits on interior surface of stomach Small intestine Folds of epithelial tissue Epithelium 3 Pepsinogen Pepsin 2 Gastric gland Mucous cell Chief cell Parietal cell HCl Chief cell 1 Cl H Parietal cell gastric pits contain four major secretory cells: a. chief cells Secret pepsinogen : 1. pepsinogen is activated by low pH to form pepsin 2. pepsin is a protease for protein digestion 24 b. Parietal cells involved in 1-HCl secretion: HCl secretion is enhanced by histamine, gastrin, HCl a-Kills microbes; b-denatures proteins (hydrolyzes peptide bonds) ; c-breakdown of cell wall d- reduce pH = 2 activates pepsinogen pepsin (partial protein digestion) E-activates pepsin 2- Intrinsic factor secretion It is a polypeptide that binds to and allows B12 absorption in the intestine 25 c. G-cell secretes gastrin hormone Gastrin : 1-activates gastric juice secretion 2-stimulates parietal cells to secrete HCl 3- stimulates chief cell secrete to pepsinogen; 4- stimulates Enterochromafin like cells (ECL) to secret histamine 5- stimulate stomach wall contraction d. D-cell secrets Somatostatin Reduce gastrin release inhibits acid E-Enterochromafin like cells (ECL) secrets histamine (stimulates acid) F. Goblet cell secretes mucus ( contains HCO3-) which has a protective role against acids and digestive enzymes 26 Gastric Glands Summery Secrete gastric juice: – Goblet cells: mucus. – Parietal cells: HCl and intrinsic factor needed for the absorption of vitamin B12. – Chief cells: pepsinogen. – Enterochromaffin-like cells (ECL): histamine and serotonin which act as paracrine regulators of the GI tract. – G cells: gastrin hormone. – D cells: somatostatin hormone. – Stomach: ghrelin hormone that regulates hunger. HCl Functions Insert fig. 18.9 Digestion and Absorption in the Stomach • • • Proteins are partially digested by pepsin. Carbohydrate digestion by salivary amylase is inactivated by acidity. Alcohol and aspirin are the only commonly ingested substances absorbed. Protective Mechanisms of Stomach Q2-Why pepsin and HCL can not damage the stomach lining? • • • • • • Parietal and chief cells impermeable to HCl. Alkaline mucus contains HCO3-. Tight junctions between adjacent epithelial cells. Rapid rate of cell division (entire epithelium is replaced in 3 days). Prostaglandins inhibit gastric secretions. Pepsin is secreted in an inactive form. • Gastric ulcers: lesions in the lining, are caused mainly by the bacterium 1-excessive gastric acid secretion in respose to high levels of gastrin which is secreted by pancreatic tumer 2-infection by Helicobacter pylori bacteria. 3- inadequate HCO3- secretion in doudenum • • •Propulsion in the Stomach - Food must first be well mixed. - Rippling peristalsis occurs in the lower stomach. - The pylorus meters out chyme into the small intestine (30 ml at a time). - The stomach empties in four to six hours. Small Intestine • In SI the partially digested food coming from the stomach is mixed with three other liquids here: 1. Bile, a substance that is released by the gallbladder to help in the digestion of fat. 2. Pancreatic juice and enzymes (released into the intestine by the pancreas). 3. Other alkaline intestinal enzymes, such as maltase, lactase and sucrose, which help to further break down different types of sugars (this is why some people have reactions to dairy products – they lack, or have very low levels of lactase, so can’t break down lactose, the main sugar in dairy products). • The major functions of small intestine are: • 1- Segmentation: major contraction activity that results in mixing chyme with Bile & pancreatic juices and other digestive enzymes. • 2-Completes digestion of carbohydrates and proteins. lipid digestion Begins then fats are broken down to glycerol and fatty acids • 3-Absorption of 90% of all nutrients: Glucose, Amino Acids, Fatty Acids, Vitamin B12, Vitamin K, Water, Na+ Ca++ Fe++ K+ Cl32 Intestinal Contractions and Motility • 2 major types of contractions occur in the small intestine: (a) Peristalsis – Alternating waves of contraction (occurs throughout digestive system). Moving bolus then chyme forward. (b) Segmentation – Moving materials back and forth to aid in mixing chyme (mostly in small intestine and colon) Special structural features increase surface area for digestion and absorption – Circular folds • • Permanent ridges of mucosa and submucosa Cause chyme to coil – Villi • • • Fingerlike projections of mucosa Contains arteriole, venule, blood capillary, and lacteal Each villus is covered with columnar epithelial cells interspersed with goblet cells. – Microvilli • • Projects of apical membrane of absorptive cells Brush border with brush border enzymes Vein carrying blood to liver Villi Microvilli (brush border) at apical (lumenal) surface Epithelial cells Blood capillaries Muscle layers Villi • Intestinal wall Epithelial cells plicae circularis Large circular folds Basal surface Lacteal Key Nutrient absorption Lymph vessel Lumen Plicae circularis folds increase the surface area and speeds up absorption process. 36 Small Intestine •Epithelial cells at the tips of villi are exfoliated and replaced by mitosis. •Paneth cells---lysozyme (anti-bacterial). •Lamina propria contain lymphocytes, capillaries, and central lacteal. The mucosa of the small intestine contains several specialized cells. Some are responsible for absorption, others secrete digestive enzymes and mucous to protect the intestinal lining from digestive actions. •Histology mucosa has intestinal glands for secretion of intestinal juice mucosa and submucosa has large folds called Plicae circularis. Each plicae has numerous villi (folds of mucosa) and each villus is covered by epithelium with projecting microvilli (brush border). This increases surface area and speeds up the absorption process. 39 “brush border” has many enzymes : i. Several carbohydrate-digestive enzymes such as maltase, sucrase, lactase i. Protein-digestive enzymes : Peptidases such as aminopetidase, dipeptidase ii. Nucleosidases and phosphatases. Nucleosidase an enzyme that catalyzes the splitting of a nucleoside to form a purine or pyrimidine base and a sugar alkaline phosphatase---removes phosphate group from organic compounds. 40 1. As chyme enters the duodenum, Peristalsis propels chyme through small intestine. 2-Chyme’s proteins and carbohydrates are partly digested but no fat digestion occurred yet. • 3. Additional digestion is aided by secretions from the liver (Bile) and the pancreas. • a. Bile is a secretion of the liver temporarily stored in the gallbladder before being sent to duodenum; bile emulsifies fat (allows fat droplets to disperse in water). 41 • Each villus contains blood vessels and a lymphatic capillary, called a lacteal. • a. A lacteal aids in the absorption of fats. • 6. Sugars and amino acids enter villi cells and are absorbed into bloodstream. • 7. Glycerol and fatty acids enter villi cells; reassembled into fat molecules, they move into lacteals. • 8. After nutrients are absorbed, the hepatic portal vein carries nutrient-rich blood from the capillaries of the villi to the liver, then to the heart. • The liver regulates nutrient distribution, interconverts many organic molecules, and detoxifies many organic molecules. • nutrients are eventually carried throughout the body by the bloodstream. 42 •Digestion and Absorption of Nutrients 43 Nutrient Absorption Summery 1. Carbohydrates a. enzymaticaly digested to form monosaccharides (glucose, fructose, galactose) b. absorbed in SI by active transport or facilitated diffusion c. enter blood capillary in villi, then directed to hepatic portal vein 44 2. Proteins a. enzymatically digested to amino acids or di- and tri-peptides b. absorbed in SI by active transport or facilitated diffusion. c. enter blood capillary in villi, then directed to hepatic portal vein 45 3. lipids a. enzymatically digested to short or long chain fatty acids b. suspended in SI in form of micelles جزيئة غرويّةwith bile salts c. micelle formation aids lipid diffusion into SI epithelial lining d. inside epithelial cells, lipids bound into chylomicrons for transport e. chylomicrons are transported to lacteal villi; then into lymphatics and then to venous blood 46 47 Carbohydrate digestion Oral cavity, Polysaccharides Disaccharides pharynx, esophagus Salivary amylase Smaller Maltose polysaccharides Stomach Protein digestion Proteins Pepsin Small polypeptides Small intestine (enzymes from pancreas) Pancreatic amylases Nucleic acid digestion Fat digestion DNA, RNA Fat (triglycerides) Pancreatic trypsin and chymotrypsin Pancreatic nucleases Disaccharides Smaller polypeptides Nucleotides Pancreatic lipase Pancreatic carboxypeptidase Glycerol, fatty acids, monoglycerides Small peptides Small intestine (enzymes from epithelium) Disaccharidases Nucleotidases Dipeptidases, carboxypeptidase, and aminopeptidase Nucleosides Nucleosidases and phosphatases Monosaccharides • Amino acids Nitrogenous bases, sugars, phosphates The portion of a nucleotide without the phosphate group is called a nucleoside Large Intestine • • • Outer surface bulges outward to form pouches called haustra, does not contain villi. Appendix: immune function. Inflammation of appendix is called appendicitis. Little absorptive function. – Absorbs H2O, electrolytes, several vitamin B complexes, vitamin K, and folic acid. – The colon houses anaerobic bacteria (e.g., Escherichia coli) which live on unabsorbed organic material; some produce vitamins. So, they form mutualistic or commensal relationships with humans. • Bacteria ferment indigestible molecules to produce short-chain fatty acids. • Intestinal microbiota (microflora) produce significant amounts of folic acid and vitamin K and B vitamins. • Reduces the ability of pathogenic species to colonize the intestine. • Excessive use of antibiotics kills the normal flora. Fluid and Electrolyte Absorption • The small intestine receives 7-9L fluid from different secretions and diet and most of this fluid and electrolytes are absorbed by small intestine. • Absorption of H2O occurs passively as a result of the osmotic gradient created by active transport. • Aldosterone stimulates NaCl and H2O absorption in the ileum. • Large intestine: – Absorbs about 90% of the remaining volume. • Secretion of H2O occurs passively as a result of the osmotic gradient created by active transport of Na+ or Cl- to the intestinal lumen. • Diarrhea---excessive water secretion in feces. • Constibation---decreased water secretion in feces. •The rectum Last portion of the digestive tract Terminates at the anal canal Internal and external anal sphincters 51 52 Defecation • Feces, including undigested material and bacteria, become more solid as they move through the colon. • Feces is stored in the rectum until they can be eliminated through the anus • The anus has two sphincters: Internal anal sphincter External anal sphincter Internal anal sphincter is composed of smooth muscle (relaxation causes the urge feeling) External anal sphincter is composed of skeletal muscle (relaxation causes defecation) These sphincters are closed except during defecation • Defecation reflex: – Longitudinal rectal muscles contract to increase rectal pressure. _ Relaxation of internal anal sphincter. – Excretion is aided by contractions of abdominal and pelvic skeletal muscles that push feces from the rectum. • Defecation occurs when rectal pressure rises and external anal sphincter relaxes. Liver The liver is a large, reddish-brown organ situated in the right upper quadrant of the abdomen. It is surrounded by a strong capsule and divided into four lobes namely the right, left, caudate and quadrate lobes. The liver has several important functions. 55 Liver •liver is largest •gland in body 56 All nutrients absorbed by the intestines pass through the liver and are processed before traveling to the rest of the body. 1. Capillary in intestine 1. Liver receives nutrient-rich blood from SI via the hepatic portal vein 2. Capillary 3. Hepatic vein 4. Inferior vena cava 57 Capillaries of the digestive tract drain into the hepatic portal vein, which carries blood to liver. Portal system: capillaries---vein--- capillaries---vein. • The hepatic portal vein is not a true vein, because it does not conduct blood directly to the heart. • It is a vessel in the abdominal cavity that drains blood from the gastrointestinal tract and spleen to capillary beds in the liver. 58 Enterohepatic Circulation •Some compounds re-circulate between liver and intestine. So, they have enterohepatic circulation •e.g bile salts, cholesterol. Hepatic blood flow • Liver receives blood from • Hepatic artery carrying oxygenated blood • Hepatic portal vein carrying deoxygenated blood with newly absorbed nutrients and possibly drugs, microbes or toxins from GI tract •The Role Of Liver 1-It acts as a mechanical filter by filtering blood that travels from the intestinal system – 2-It detoxifies several metabolites including the breakdown of bilirubin, ETOH, detoxification and other dietary toxins. Chemical alteration of the molecules such as ammonia. Ammonia is produced by deamination of amino acids in the liver. It is very toxic. So, the liver converts it into urea that is excreted in urine. – other molecules that are cleared from blood are eliminated in the feces. 3-The liver has synthetic functions, producing albumin and blood clotting factors and cholesterol 4-Regulates carbohydrate metabolism a. glucose secretion into blood/absorption from blood into glycogen storage b. regulated by insulin & glucagon 61 •The Role Of Liver 5-However, its main roles in digestion are in the production of bile and metabolism of nutrients. The bile produced by cells of the liver, enters the intestines at the duodenum. Here, bile salts break down lipids into smaller particles so there is a greater surface area for digestive enzymes to act 62 Major Categories of Liver Function Functional category Actions Detoxification of blood Phagocytosis by kupffer cells Chemical alteration of biologically active molecules (hormones & drugs) Production of urea, uric acid & other molecules that are less toxic than parent compounds Excretion of molecules in bile Carbohydrate metabolism Conversion of blood glucose to glycogen & fat Production of glucose from liver glycogen & from other molecules (amino acids,…) by gluconeogenesis Secretion of glucose into blood Lipid metabolism Synthesis of triglycerides & cholesterol Excretion of cholesterol in bile Production of ketone bodies from fatty acids Protein synthesis Production of albumin, clotting factors and plasma transport proteins Secretion of bile Synthesis of bile salts Gallbladder • Sac-like organ attached to the inferior surface of the liver. • Functions to Stores and concentrates bile. • When gallbladder fills with bile, it expands. – Contraction of the muscularis layer of the gallbladder ejects bile into the common bile duct into duodenum. • When small intestine is empty, the sphincter of ampulla (sphincter of Oddi) closes. – Bile is forced up to the cystic duct to gallbladder. • Gallstones: small hard deposits that can produce painful symptoms by obstructing the cystic or common bile duct. Also, they contain cholesterol as their major component. •The sphincter of ampulla or sphincter of Oddi is a muscular valve that controls the flow of digestive juices (bile and pancreatic juice) through the ampulla of Vater (is formed by the union of the pancreatic duct and the common bile duct) into the duodenum. •Pancreas Pancreas Finally, the pancreas is a lobular, pinkish-grey organ that lies behind the stomach. Its head communicates with the duodenum and its tail extends to the spleen. The organ is approximately 15cm in length with a long, slender body connecting the head and tail segments. 67 The pancreas has both exocrine and endocrine functions. Endocrine refers to production of hormones which occurs in the Islets of Langerhans. The Islets produce insulin, glucagon and other substances and these are the areas damaged in diabetes mellitus. The exocrine (secretory) portion makes up 80-85% of the pancreas and is the area relevant to the gastrointestinal tract. 68 It is made up of numerous acini (small glands) that secrete contents into ducts which eventually lead to the duodenum. The pancreas secretes fluid rich in carbohydrates and inactive enzymes. Secretion is triggered by the hormones released by the duodenum in the presence of food. Pancreatic enzymes include carbohydrases, lipases, nuclease, and proteolytic enzymes that can break down different components of food. These are secreted in an inactive form zymogens (inactive enzyme) to prevent digestion of the pancreas itself. The enzymes become active once they reach the69 duodenum. E. Role Of The Pancreas In Digestion approx 1.5L/day pancreatic secretions are produced secretions enter duodenum via two pancreatic ducts many different components in these secretions a. NaHCO3 – buffers pH of chyme b. Pancreatic amylase 70 c. Trypsinogen: is activated by enterokinase to become trypsin trypsin acts on other proteases to activate them d. lipases e. ribonucleases (a type of nuclease that catalyzes the degradation of RNA into smaller components. ) 71 Fig. 18.29 EN: Enterokinase Pancreatic juice Summery – 1200-1500ml daily – Mostly water • Sodium bicarbonate – buffers acidic stomach chyme • Enzymes – Pancreatic amylase – Proteolytic enzymes – trypsin (secreted as trypsinogen), carboxypeptidase – Pancreatic lipase – Ribonuclease and deoxyribonuclease