Electronic Health Record
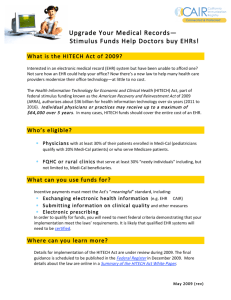
advertisement

ELECTRONIC HEALTH RECORDS Week 6 WHAT IS A PATIENT RECORD? A historical record of patient care Account of a patient’s health and disease following medical consultation. Typically contains findings, considerations, test results and treatment information related to an ailment / disease process. A communication tool among care providers A research and knowledge-gaining tool A teaching tool An operational tool (e.g., order entry) An administration record (e.g., to manage resources) A legal record with considerable longevity EVOLUTION OF PATIENT RECORDS (1) In the late 19th century every clinician kept patient medical details in a leather bound ledger. Contained a chronological account of all patient consultations. Known as a ‘Time-Oriented Medical Record’ Notes pertaining to a particular patient could be pages apart depending on the dates of subsequent consultations. This scattered nature made it difficult to assess disease progression. Furthermore, a patient could be treated by more than more clinician, therefore some notes would be contained in other clinicians ledgers. In early 20th century a separate file for each patient was adopted. Origin of patient-centered medical records No fixed criteria for data entry therefore different clinicians recorded differed pieces of data. EVOLUTION OF PATIENT RECORDS (2) In 1920, a minimal set of data that all clinicians should record was agreed upon. This early ‘standard’ became the foundation framework from which current medical record data is recorded. In 1960 the ‘Problem-Oriented Medical Record’ was established. Each patient assigned one or more problems. Notes recorded using the ‘SOAP’ structure S: subjective – complaints reported by the patient O: objective – the findings of the clinical staff A: assessment – test results, diagnosis P: plan – the suggested treatment etc. ISSUE: required a lot of effort to record information for a patient reporting several problems in parallel. EVOLUTION OF PATIENT RECORDS (3) ‘Source-Oriented Medical Records’ are the most commonly used system today. Record ordered according to the method by which they were obtained. Notes of the visit X-ray reports Lab reports, blood tests etc. Within each section, records are stored in chronological order. The SOAP method is still used for the clinical notes. How well is this paper based method suited for its clinical purpose? COMMON USES FOR PATIENT RECORDS Support Patient Care A source of evaluation and decision making A source for information that is shared among care providers. A legal report of medical actions Supporting research Clinical research, epidemiological studies, assessing quality of care, and post marketing surveillance of drugs. Educating clinicians Healthcare management and services SHORTCOMINGS OF PAPER BASED PATIENT RECORD (1) Increasing number of medical specialties Likely that patient treated by a number of these specialists for a single condition. One record /patient causes too many logistically issues Result: as many patient records for a single patient as there are specialists managing their care. Patient data becomes scattered among different specialists / centers. Clinician must request this data from a number of specialists to gain an overall picture Paper based records can only be in one place at a time – often it become misplaced in transit. Handwriting Illegible, data missing, notes too ambiguous. Space requirements. Large warehouses exist to house patient records PAPER BASED PATIENT RECORDS SHORTCOMINGS OF PAPER BASED PATIENT RECORD (2) Limited access to complementary medical information. X-ray, MRI results or other lab test feedback. Data backup issues http://www.youtube.com/watch?v=VzY12fTbNt8&feature=rela ted http://www.youtube.com/watch?v=DV5jod3INHY&feature=rel ated Perhaps the most fundamental limitation of paper-based records is that they can only contribute ‘passively’ to the decision making of the clinician. Paper-based records cannot give rise to active reminders, warnings or advice. Record cannot actively draw the attention of a clinician to: Abnormal lab results, Errors in data / medication entry. For scientific analysis, the contents need to be transcribed, with the potential for errors. PAPER FREE MEDICAL RECORDS http://www.youtube.com/watch?v=9jAH9hdF0xk &feature=related WHAT IS AN ELECTRONIC HEALTH RECORDS (EHR)? A repository of electronically maintained information about an individuals lifetime health status and health care, stored such that multiple persons can gain authorized access to it. Also known as: Electronic Patient Records (EPR) Electronic Medical Record (EMR) Patient Health Record (PHR) Computerised Patient Record (CPR) Computer Based Patient Record (CBPR) Electronic Clinical Information Systems (ECIS) Centerpiece of Health Informatics Potential to improve upon: Patient safety Staff Productivity Information Storage and Retrieval http://www.youtube.com/watch?v=t-aiKlIc6uk EPR: 5 FUNCTIONAL COMPONENTS Integrated View of Data Integrated Communic ations Support Clinical Decision Support Electronic Health Record Access to Knowledge Resources Clinical Order Entry EHR COMPONENTS (1) Clinical decision support Secure Messaging for communication support between clinicians, patients and support staff. Appointment scheduling and patient portal access. Referral Management Retrieval of lab and X-ray reports electronically Access to previous consultation notes and medication history. Support for paperless order entry services Provide alerts, reminders and clinical practice guidelines. Electronic ordering for prescriptions, x-ray, consults and other diagnostic tests. Support for multimodal data input Text, image, voice, dictation. EHR COMPONENTS (2) Interfacing with PDAs and portable computers Remote access from home or office Ambulatory access E-prescribing Knowledge resources for both patients and clinical staff Ability to scan in text, images Ability to create graphs, charts Ability to generate patient lists or disease registries. Data Warehouse –backup system Public health tracking and reporting Support for Client – Server or web based Application Service Providers (ASPs) RATIONALE FOR EHR SYSTEMS (1) EHR systems have the potential to bring huge benefits to patients and are being implemented in health systems across the developed world. EHRs aim to provide easy navigation through the entire medical history of a patient. Storing and sharing health information electronically can: speed up clinical communication Records available 24/7 reduce the number of entry errors assist doctors in diagnosis and treatment patients can have more control of their own healthcare. electronic data also have vast potential to improve the quality of healthcare audit and research. RATIONALE FOR EHR SYSTEMS (2) record can be used by multiple personnel at the same time record is accessible from anywhere (even from home) clear, well-organized, legible documentation data can be reused for other purposes data can be integrated from multiple sources transparently data can be validated automatically provide reminders that tests / examination are overdue. enables multiple automated research and decision-support functions (analysis, machine learning and data mining, automated diagnosis, reminders, guideline-based care) decision support can be integrated with use of the patient record increasing access to data through EHR systems also brings new risks to the privacy and security of health records. RATIONALE FOR EHR SYSTEMS (3) EHR have the potential to provide many large volumes of data! Many of the major players are offering free services to healthcare facilities in return for access to anonymous patient data. http://www.youtube.com/watch?v=V35Kv6ZNGA&feature=related POSITIVE EHR Patients Perspective http://www.youtube.com/watch?v=n1L4nKdYr6E&fea ture=related Doctors Perspective http://www.youtube.com/watch?v=mtLi6vmJ4fo&feat ure=fvw http://www.youtube.com/watch?v=fjnyDNZE3RY&fea ture=related DIFFERENT USES OF EHRS (1) Inpatient Research Department Outpatient Nursing Home Primary Care EHR Disease Specific Hospital Emergency Department Intensive Care DIFFERENT USES OF EHRS (2) General practitioners highest level of computerisation with the vast majority of surgeries using IT systems both for administrative and clinical purposes. most practices store some patient information electronically dispensed with paper systems altogether after scanning old paper notes into new electronic systems. Hospitals Level of computerisation varied widely but consistently lower than in general practice. Most hospitals use basic Patient Administration Systems (PAS) for scheduling, recording admissions and discharges, and storing patient demographic and basic diagnosis information. In some clinical areas, such as theatres and pathology, more sophisticated systems have often been used for both administrative and clinical purposes. The overwhelming majority of patient records are still stored in often voluminous paper form. Lack of unifying standards means that IT systems in different departments within a single hospital are often unable to communicate. Community and mental health care providers Levels of IT use have been the lowest of all. Disease Specific Complex systems have been developed across clinical networks with responsibility for a particular patient group. INTEGRATION OF EHR AND DECISION SUPPORT MODULES Decision support is most effective when integrated with an EHR The most likely opportunity for providing decision support is when the physician is assessing the patient record or entering an order All or most relevant patient data can be accessible to the DSS and do not require separate entry Physician should always be able to override the recommendation and, if relevant, provide feedback ORDER ENTRY A major function of an EHR system is allowing care providers to enter clear, legible orders for patient care anytime, anywhere Supports validation of order, issuing of alerts, suggestion of relevant information and knowledge, and even actions Quick effect on physician ordering behavior EHR AND KNOWLEDGE SOURCES The most effective time to provide access to knowledge is when the care provider is browsing the patient record A query can be formulated in a contextsensitive manner with respect to the patient record, thus anticipating the physician’s needs Note: Queries often have relatively expected structure and content (e.g., which drug is useful for condition X in context Y; What are side effects of drug Z when used in manner W; What clinical guidelines are most relevant for disease D in patients of type P) EHR ISSUES: COSTS Large initial set-up investments Hardware, software, training, support, maintenance Significant workflow changes Significant organisational changes Difficult data entry relative to handwriting Potential catastrophic failure – system crash, hack, loss of data. Paper records also have “down” times Notes unavailable 30% of the time, natural disasters EHRS: MAJOR ISSUES Data Entry Data capture: the scope of the data that is or can be represented in the EHR Data input: coded data are difficult to input by physicians; text is less useful for processing Errors can be reduced by multiple validity checks VALIDITY CHECKS DURING DATA ENTRY IN AN EHR Range checks (Hemoglobin in [0..30] Gr/Dl) Pattern checks (a telephone number pattern) Numeric and other inter-data constraint checks (total of WBC differential is 100%) Consistency checks (pregnant male??) Temporal-abstraction checks (weight cannot change by 50 Kgs in 2 days) Spelling checks PHYSICIAN-ENTERED DATA The main challenge to EHR developers! Patient histories, physical findings, interpretations, diagnostic and treatment plans Several very different entry methods Transcription of dictated or written notes Structured encounter forms from which notes are transcribed and even encoded Direct entry of data by physician via computer Speech recognition might alleviate some of the difficulties SECURITY ISSUES IN EHRS Authorization Is my dentist allowed to see my gynecological record? Which fields of my record can my or another GP view? Who has asked to view my records last month? Authentication Is this user really my physician? Encryption Can an eavesdropper to my doctor? Eventually, understand the message sent security depends on people SUMMARY OF ADVANTAGES AND DISADVANTAGES ADVANTAGES OF EHR (1) The biggest advantage is that all data is stored in one place, and, can effectively be accessed anywhere. This is as opposed to paper based records where the records can only really be in one place at any time. This means that a nurse in a hospital can view the same records as a doctor in a remote surgery is viewing. To move a paper based record to another location requires faxing, posting etc. This is costly and slow. With paper records one part of the medical history may be stored in the hospital whilst another part may be located in the doctors surgery. ADVANTAGES OF EHR (2) The physical storage requirements of electronic records are also by far superior to their paper counterparts. Paper takes up much more physical space. A particular issue with medical records is that they may include different media, such as x-rays, notes, ECG recordings, perhaps even vide or audio tapes. It is often difficult to store different types of media in one place. Electronic records get a round this problem as most forms information can be stored and linked digitally on the same media (i.e. on the same disk). Information can also be archived and disk space can be recycled much more efficiently. ADVANTAGES OF EHR (3) Handwritten and paper based records are much more prone to error. Physicians are notorious for poor hand writing. Forcing them to type up notes gets around this problem. Some forms of paper based or hard media (such as micro films or images) may deteriorate over time. Digital information will not deteriorate. This is particularly an issue in prescribing. This potentially can reduce medical errors and in turn reduce costs that may result from incorrect diagnosis. These costs may arise from more expenditure in patient treatment and law suits. DISADVANTAGES OF EHR (1) Cost Initial costs. It is costly to install all the infrastructure necessary to effectively run such a system. Think of the expenditure of kitting out all health centres in NI with PCs and all hospitals. This would just represent a fraction of the start up cost. Other start up costs include training users, converting existing records. Cost to maintain system. Healthcare providers must provide all the support necessary to make sure the system is extremely robust and versatile. Cost of technical staff. Costs of training programmes to continually educate new medical staff. Who should pay for each part? DISADVANTAGES OF EHR (2) How do we treat old records. We already mentioned the cost of converting paper based records to electronic records. But is there even a practical way to enter all these records? Some systems opt for scanning the records in and storing them as images, or use ocr. DISADVANTAGES OF EHR (3) Security. Medical data is up there with bank details. Must be treated with utmost respect! If data is being transmitted around a large system there is much potential for loss of data or compromise of data. How do we ensure that only the right people have access to this data. People are very wary of this, both patients and practitioners. http://www.youtube.com/watch?v=JJjjLaw7PRM DISADVANTAGES OF EHR (MISC) Some more disadvantages: It is difficult to get people to accept change. Many vendors are now producing healthcare solutions and its hard to link all these systems together. Methods of input may be difficult for older users. TRENDS IN EHR The biggest challenge that this technology faces is it’s incorporation into current practices in healthcare delivery. This problem is not easy to resolve. There are other trends that advances in technology can address: These include Facilitating better data entry. Making data entry as easy as possible is essential if we want clinicians to use electronic means to enter and share accurate patient info on a national network. Typing may not be most suitable for all doctors. Perhaps a way to proceed is to allow doctors to dictate information. Later this information can be mined to store key words. Facilitating easier data access and interpretation. It is quicker to retrieve and assimilate information by reading and scanning than by listening to speech. Reading print is quicker than reading from a screen. Regardless the huge amounts of information stored in EHRs needs to be presented carefully. There is much more scope for effective presentation using computers. (i.e. computers can generate the output in any way). We need to think of the best ways to convey this information. EHR SUMMARY EHR systems also bring new risks, particularly to the privacy and safety of health information. Electronic systems allow access to data from many locations, increasing the likelihood of a security breach; they can also give individuals access to much more data than was previously possible, increasing the damage caused by system misuse. Personal health information is often highly sensitive, and it is therefore difficult to repair the damage caused by a breach of privacy. All these risks can be mitigated, but there is little doubt that EHR systems will create, as the European Data Protection Working Party acknowledged, “a new risk scenario” for personal health information. AMERICAN CASE STUDY Veterans Health Information Systems and Technology Architecture (VistA) VETERANS HEALTH INFORMATION SYSTEMS AND TECHNOLOGY ARCHITECTURE (VISTA) Source: http://upload.wikimedia.org/wikipedia/en/8/8f/VistA_ 19 YEAR HISTORY The Department of Veteran’s Affairs has had automated information systems for medical information since 1985. Formerly known as the Decentralized Hospital Computer Program (DHCP) it is now known as the Veterans Health Information Systems and Technology Architecture (VistA). HISTORY (2) In the late 1990’s the component of VistA known as the Computerized Patient Record System (CPRS) was introduced. This has been a highly successful venture that integrated for the health care provider most of the tools for patient centered healthcare. Patient Centric Viewpoint allowing multiple users to view information and work within the patient chart simultaneously in a “tab-like” Graphical User Interface (GUI) environment. Provided the order entry for Labs, Pharmacy, Imaging, Nutrition and Consults and Procedures in one place. Reduced the chances of transcription error since orders flow directly from the Clinician to ancillary service. Created tools for local modifications to create order sets, such as standing or admission orders, and templates, providing standard or required text in progress notes, consults and procedures. HISTORY (3) o o o Clinical Alerts for Critical Lab and Imaging results are sent electronically to the ordering provider for viewing and action. A backup system of alerts for clinical follow-up is also effective in making sure there is some responsible clinician in case the ordering provider does not act upon the alerts. Order Checks are in place to prevent medication contraindications based on previous patient orders, lab results (ex. Creatinine Clearance) or other physical information. Clinical Reminders provide information concerning needs for the patient based diagnosis, age, or other highly individualized factors. o o Imaging results available online at any workstation for reference. Remote Data allowing access to clinical information from any other sites that the patient might have had a visit. CPRS IS GOOD…. BUT DOES HAVE SOME DISCREPANCIES Lacks the ability to review across a patient group Does not easily allow information that would be tracked on a flow sheet Patient signatures are not available electronically, meaning that there continues to be some need of a paper record Does not include the identified patient with the ability to participate in their own care THE NEXT GENERATION CPRS-R (Computerized Patient Record System-Repackaging) is the next phase in the development of the clinical record. HealtheVet Desktop is one of the first releases of CPRS-R. This will provide a framework that can be reengineered with a wide range of clinical applications plus enabling seamless integration between independently developed applications. CPRS will only be one small part of CPRS-R, a great deal more functionality and flexibility will be available than currently exists. CARE MANAGEMENT One of the first products in current use in the HealtheVet Desktop is Care Management. Care Management is unique since it finally allows the clinician the ability to scan alerts, scan and sign multiple documents and create individual personalized electronic messages across a group or team list of patients. It also is one of the first tools that can provide by-role selection of information via the use of Perspectives, currently as Clinician and Nursing. Care Management has limitations to what activities, such as order entry, progress notes or access to complete linear patient data. For this reason, the HealtheVet Desktop provides the unique ability for linkage from Care Management, connecting through to the same patient, to CPRS where these tasks can be accomplished. PERSONAL EMPOWERMENT: MY HEALTHEVET My HealtheVet is a web-based application that creates a new, online environment where veterans, family and clinicians may come together to optimize veterans’ health care. My HealtheVet empowers the veteran by providing powerful heath education and assessment tools, online services, health record access, and messaging between the veteran and clinicians. Provide online prescription refills and co-payment balance review Use online calendar to set and track their own appointments Veterans will be able to view and maintain a copy of key portions of their own health care record The Veteran will be able to share all or part of the information in their account with health care providers, inside and outside the VA. GLOBAL COLLABORATION: HEALTHEPEOPLE (1) HealthePeople is a collaborative strategy, including making HealthePeople-VistA (the public version of VistA), that takes VistA outside the VA to support high quality, accessible and affordable health care that will substantially improve the health of veterans and, potentially, all people in the U.S and perhaps other countries. The title reflects the key thrust of the effort: a strong people focus, strong health focus and a heavy reliance on “e” the electronic means as a key enabler. Public and private sectors organizations are encouraged to join this effort to help adopt standards for architecture, data and communications to develop model, high performance health information systems. GLOBAL COLLABORATION: HEALTHEPEOPLE (2) Make high performance health information systems more affordable, available and interoperable and make electronic health information system information available to organizations that serve the poor and near poor at close to no cost as are possible. Will enable easier and more secure sharing of health information amongst people and their health care providers VA is already working closely with DoD (Department of Defense) and HHS (Human Health Services). Interest has also been expressed by other public and private sector health related organizations such as the Institute for Medicine, foundations, commercial technology companies, State and local agencies and other health care providers.