NUR 430 Gero Group Project
advertisement

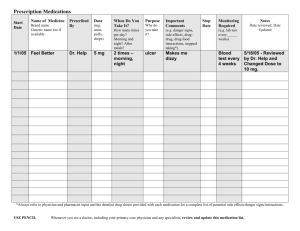
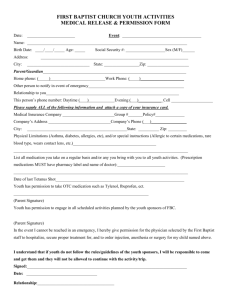
Living At Home Safely Home Sweet Home Case Study Mr. Harms is a 84 year old man that still lives in his own home. He has children and grandchildren that visit him regularly. His adult son calls him on a daily basis to check in. Mr. Harms takes medications to regulate his blood pressure. His medications consist of a betablocker, a daily aspirin, an occasional Aleve, a daily multivitamin, vitamin E and Vitamin C. Mr. Harms is independent with ambulation but on occasion has had some minor falls with only bumps and bruises. His falls have been related to tripping over his rug in the hallway and trying to get down the front stairs to go get the mail. He enjoys working in his flower garden and meeting the guys for coffee at the local café. Mr. Harms also attends church regularly when he is able to get a ride. He doesn’t drive anymore due to his macular degeneration. Patient and Family Teaching In relation to the above described case study, the following slides will discuss the possibilities of keeping Mr. Harms in his own home, the availability of alternative housing, and the teaching information for the patient and family. In addition, a home environment assessment should be done to include stairs, bathing and toileting, medications, predetermined wishes, nutrition and cooking, falls, smoke detectors, emergency numbers, temperature of home and water, neighborhood safety, and finances. (Tabloski, p.65). Additional Patient and Family Teaching Teach bleeding risks of combined medications Encourage patient to get all medications at the same pharmacy, preferably from one provider, and keep a list of medications in wallet at all times Teach blood pressure monitoring, recording, and symptom reporting as necessary Encourage patient to change positions slowly to avoid falls Provide chair or bench to do outdoor activities with flower garden Put flowers in reachable areas Arrange for transportation to church and other enjoyed activities outside of the home Causes of safety decline at home 1. Decline in overall health status 2. Polypharmacy 3. Lack of family or social support: Self isolation 4. Refusal to see primary care physician routinely 5. Low fixed incomes 6. Depression/Anxiety or other psychological disorder 7. Significant loss of spouse or loved one 8. Lack of resources or equipment needed to minimize safety risks 9. Fears of losing independence or moving to a facility 10. Impaired memory or judgment Considerations for living at home safely Legal aspects Finances Power of Attorney Advance Directives Ethical Cultural Respect cultural beliefs and customs of patient and family Professional Be respectful of patient and family at all times Spiritual Transportation to church or arrange visits from church officials Available television stations or radio stations to listen to services Lifeline Medical alert system that provides access to help 24/7/365 Necklace or bracelet worn with button to push for access to help Standard or advanced fall system that if unable to push button after a fall the system will be automatically alerted Cost is about $1/day and most companies have no equipment fee, no contracts, and no set up fee Volunteers age 55 and over who make a difference by providing assistance and friendships. They assist with grocery shopping, bill paying, and transportation to medical appointments, and they alert doctors and family members to potential problems. Senior Companions also provide short periods of relief to primary caregivers. Senior Companions Any housing arrangement designed exclusively for seniors, generally those aged 55 and over. Housing varies widely, from apartment-style living to freestanding homes. Housing is friendlier to older adults, often being more compact, with easier navigation and assistance in yard maintenance (if there is a yard). Also called retirement communities, retirement homes, senior housing, and senior apartments. Socialization with other elders. Transportation services to ease commutes for shopping, etc. Independent Living Types of Independent Living Subsidized senior housing. In the U.S., there are senior housing complexes, subsidized by the U.S. Department of Housing and Urban Development (HUD), for low-income seniors. Keep in mind that depending on the area, waiting lists can take years, so it’s a good idea to plan well in advance for this option. Senior apartments. Senior apartments are apartment complexes restricted by age, usually 55 and older. Rent may include community services such as recreational programs, transportation services, and meals served in a communal dining room. Retirement communities. Retirement communities are groups of housing units for those aged 55 and older. These housing units can be single-family homes, duplexes, mobile homes, townhouses, or condominiums. If you decide to buy a unit, additional monthly fees may cover services such as outside maintenance, recreation centers, or clubhouses. Continuing Care Retirement Communities (CCRCs). CCRCs offer service and housing packages that allow access to independent living, assisted living, and skilled nursing facilities in one community. If residents begin to need help with activities of daily living, for example, they can transfer to an assisted living or skilled nursing facility on the same site. Sited from http://www.helpguide.org/elder/independent_living_seniors_retirement.htm What is Assisted Living? Assisted Living Communities provide: 1. Comfortable apartments with home like amenities such as personal bathrooms, kitchens, and dining areas 2. Access to meals and medications, group activities, and social events 3. Professional assistance if needed and for emergencies 4. Are not federally regulated but do have their own individual services and regulations Benefits to Assisted Living Facilities: 1. Increased independence and freedom to continue life as desired with minimal assistance and supervision. 2. Peer and professional support 3. Decreased stress on family members 4. Care that fits you! Assisted Living Resources: Eldercare.gov Assisted Living Federation of America: alfa.org AARP.org Assisted Living Nebraska: www.assistedlivingnebra ska.com Home Health Care Historically home health care primarily consisted of private duty nurses or family members. Over the last 20 years the complexity and scope of home health care has grown relating to the rising cost of health care, the aging population, growing emphasis on managing chronic illness and stress, preventing illness and enhancing quality of life. For a time Home Health Care was viewed as end of life care. People were discharged from an acute care facility and sent home to die. Now people are able to stay home and avoid being admitted to acute care. A Home Health Nurse must be able to work independently, provide direct care, manage the care (including therapies and other members of the interdisciplinary team). They must be able to educate their patient and be willing to research and consult to provide the best care possible. The relationships between the nurse and client is generally more intimate and the nurse needs to be aware of inadequate care or limited support. The nurse is more likely to pick up on abuse or caregiver burn out of family members. Having a family member that lives at home can cause more stress on family members because of the increased and complex duties they may be expected to perform. The nurse needs to advocate for both the client and the family. Families tend to question care more often when it is in their loved ones home. They ignore advice more frequently and may do things their own way and set their own priorities and schedules. The nurse should attempt to have a close relationship with the family of their client. Medicare costs for home health increase 10 % each year. 3rd party payees favor home health because it’s more cost effective than acute care. There is increasing ability to provide high technological services in the home. Consumers want to stay home instead of going into an institution. Paying For Home Health Care Private Pay 3rd party reimbursement Combination of sources There must be a physicians order and physician approved plan before Medicare or Medicaid will cover any part of care. The nurse should ensure they also have a DME (durable medical equipment) benefit with their insurance or that they’re able to pay privately. Oasis (the Outcome and Assessment Information Set) is required as part of the Medicare condition of participations (http://www.cms.hhs.gov/oasis/) In Nebraska an agency must be licensed and certified. Certification is necessary in order to receive and pay from Medicare. Non-Medical Private Pay Homecare Non-Medical Private Pay Homecare agencies provide caregivers to assist the older adult in their own home from 3 hours a day to 24 hours a day. Services are out of pocket and not covered by Medicaid, Medicare or insurance. Some are now starting to work towards being able to accept respite waivers for caregiver relief, this is difficult as they are private pay/non-medical agencies, and would have to become Medicaid/Medicare certified to accept the waivers. Services provided are primarily Non-Medical. Cost of these programs in this area is around 20 dollars an hour for a minimum of 3 hours. Service agencies can provide Laundry, Linen changes Meal planning, preparation, feeding assistance Bathing assistance, personal hygiene, incontinence cares Standby assistance with morning and evening routines Transfer assistance Medication reminders Errands Incidental transportation Light housekeeping and organization (dishes, vacuuming, dusting) Clutter prevention Kitchen and bathroom cleaning Companionship Light exercise-walks Friendly and supportive conversation Plan and encourage social activities Service agencies Remaining in the home 24 hours a day if family member is not able, this is especially helpful in those with Alzheimer’s or those needing 24 hour care and is not safe alone. Services can be used temporarily or long term; the benefits outweigh the costs if it is affordable to the older adult. Beneficial to someone just out of the hospital who may need a little extra help until regaining strength. These services can also provide regular respite relief to caregivers to avoid caregiver burnout, allowing caregivers to attend to own needs or social outings. Often time’s Medical home care is used in conjunction with private pay services, and agencies will communicate on the patients needs. Home Adaptations Presence of grab bars around bath tubs and toilets, along with non slip surfaces in the shower and bath tub. A hand held shower head should be installed if it doesn’t exist. A raised toilet seat and a shower chair if necessary for safety. There should be some sort of safety lighting for at night. The walk ways need to be clear from clutter and throw rugs should be removed. In some situations a hospital bed may be warranted. Lifts are available depending on therapy evaluations and recommendations. The ease of access to shelves should be assessed and modifications made if necessary. Water temps should be set below 120 at least. Accessibility to light switches should be assessed. As well as accessibility to toileting- including bed pans or urinals. The availability and access of help should be assessed. Medications should be monitored and a system should be implemented that works best for the client. Ensure that needles are being disposed of properly. Medication Management The ability for an older person to manage medications can difficult especially when multiple medications are involved. This poses a safety risk and can increase the number of hospitalizations. There are many steps we can take to help. Non-adherence-medication non-adherence happens for many reasons; the older adult is not able to afford the medication, poor teaching on purpose of medication. Many People tend to stop taking a medication when they feel better, not attributing to the fact that the medication is the reason they feel better. The older adult may simply forget frequently to take them. Cost-We all know that medication costs can be outrageous, especially when a generic is not available or the older person does not have access to supplemental RX insurance. Some of the medications are not covered by insurance. Some older persons have to choose between eating a good meal and buying medication. Contacting the manufacture of the medication often results in discounts. Some physicians office’s will offer samples Old prescriptions- clean out that medicine cabinet! Expired prescription and over the counter medications can be one of 2 things, Non effective or TOXIC! Throw away all medications past the expiration date, or discontinued medications. A person is less likely to become confused with fewer medication bottles lying around; also this can help to reduce accidently taking the wrong medications. Check local pharmacy for disposal instructions of certain medications, such as narcotics and antibiotics. Medications should be reduced to only those necessary any ineffective meds or duplicate meds should be discontinued Herbal supplements should be evaluated these can interact with other medications and effect lab results such as PT INR Medication Consistency All of the older person’s physicians and pharmacist need to be on the same page with the patients currently prescribed meds and over the counter meds they are taking. Medication teaching should be done with the patient and family/caregivers on all medications, side effects, purpose, dose and frequency. This teaching can be given by the physician’s office, pharmacist, or homecare nurse. Using a weekly med sorter for multiple medications can decrease confusion, avoid overdosing or missing a medication, the patient or a family member can generally be taught how to set this up. The Patient should have a medication list they can follow to assist with set up, on this list should be the medication name (generic and brand), purpose, dose, frequency and time medication is taken. Pay close attention to a pill needing broke in half to make the correct dose. It may be helpful to actually tape the pill or a picture of it to the list. There are websites available to help with this. Update any changes immediately. A med minder or med machine dispenser can be helpful, an alarm and verbal instruction to take medications can be set to the individual patient. The machine only dispenses the meds due at that time. Machines can be purchased privately or rented through programs such as Philips the same organization that provides life line. In some cases the machines are covered under Medicaid or Medicare. Caregiver Burnout Caregiver burnout is a state of physical, emotional, and mental exhaustion that may be accompanied by a change in attitude -- from positive and caring to negative and unconcerned. Burnout can occur when caregivers don't get the help they need, or if they try to do more than they are able -- either physically or financially. Caregivers who are "burned out" may experience fatigue, stress, anxiety, and depression. Many caregivers also feel guilty if they spend time on themselves rather than on their ill or elderly loved ones. This puts care givers at an increased risk for Depression, dependent adult abuse or neglect. Signs and Symptoms to watch for Withdrawal from friends, family, and other loved ones Loss of interest in activities previously enjoyed Feeling blue, irritable, hopeless, and helpless Changes in appetite, weight, or both Changes in sleep patterns Getting sick more often Feelings of wanting to hurt yourself or the person for whom you are caring for Emotional and physical exhaustion Irritability Prevention Find someone you trust -- such as a friend, co-worker, or neighbor -- to talk to about your feelings and frustrations. Set realistic goals, accept that you may need help with caregiving, and turn to others for help with some tasks. Be realistic about your loved one's disease, especially if it is a progressive disease such as Parkinson's or Alzheimer's. Don't forget about yourself because you're too busy caring for someone else. Set aside time for yourself, even if it's just an hour or two. Remember, taking care of yourself is not a luxury. It is an absolute necessity for caregivers. Talk to a professional. Most therapists, social workers, and clergy members are trained to counsel individuals dealing with a wide range of physical and emotional issues. Take advantage of respite care services. Respite care provides a temporary break for caregivers. This can range from a few hours of inhome care to a short stay in a nursing home or assisted living facility. Prevention Know your limits and stay within them Educate yourself. The more you know about the illness, the more effective you will be in caring for the person with the illness. Develop new tools for coping.. Stay healthy by eating right and getting plenty of exercise and sleep. Accept your feelings. Having negative feelings -- such as frustration or anger -- about your responsibilities or the person for whom you are caring is normal. It does not mean you are a bad person or a bad caregiver. Join a caregiver support group. Sharing your feelings and experiences with others in the same situation can help you manage stress, locate helpful resources, and reduce feelings of frustration and isolation. Who can help? Home health services -- These agencies provide home health aids and nurses for short-term care, if your loved one is acutely ill. Some agencies provide short-term respite care. Adult day care -- These programs offer a place for seniors to socialize, engage in a variety of activities, and receive needed medical care and other services. Nursing homes or assisted living facilities -- These institutions sometimes offer short-term respite stays to provide caregivers a break from their caregiving responsibilities. Private care aides -- These are professionals who specialize in assessing current needs and coordinating care and services. Caregiver support services -- These include support groups and other programs that can help caregivers recharge their batteries, meet others coping with similar issues, find more information, and locate additional resources. Community Resources Nebraska Department of Health and Human Services; dhhs.ne.gov EASTERN NE OFFICE ON AGING, Dennis Loose, Director, 4223 Center Street Omaha, NE 68105 402-444-6444 Fax: 402-444-6503 Out of State Toll Free: 888-554-2711 www.enoa.org AGING PARTNERS, June Pederson, Director,1005 O Street Lincoln, NE 68508-3628 , 402-441-7070 Fax: 402-441-7160 Toll Free within NE: 800-247-0938 aging.lincoln.ne.gov NORTHEAST NE AREA AGENCY ON AGING, Connie Cooper, Director,119 W Norfolk Ave, Norfolk, NE 68701, 402-370-3454 Fax: 402-370-3279 Toll Free: 800-672-8368 www.nenaaa.com Community Resources SOUTH CENTRAL NE AREA AGENCY ON AGING Rod Horsley, Director,Suttle Plaza, 4623 2nd Ave, Suite 4, Kearney, NE 68848-3009, 308-234-1851 Fax: 308-2341853 Toll Free: 800-658-4320, www.agingkearney.org MIDLAND AREA AGENCY ON AGING, Jerrell Gerdes, Director, 2727 W. 2nd Street, Suite 440 Hastings, NE 68901, 402-463-4565 Ext. 310 Fax: 402-463-1069, Toll Free: 800-955-9714 www.midlandareaagencyonaging.org BLUE RIVERS AREA AGENCY ON AGING, Larry Ossowski, Director 1901 Court Street, Beatrice, NE 68310, 402223-1376 Fax: 402-223-2143 Toll Free: 888-317-9417 www.braaa.org Community Resources WEST CENTRAL NE AREA AGENCY ON AGING, Linda Foreman, Director, 115 North Vine, North Platte, NE 69101, 308-535-8195 Administrative Fax: 308-535-8197 CHOICES Program Fax: 308-535-8190 Toll Free: 800662-2961, www.wcnaaa.org AGING OFFICE OF WESTERN NEBRASKA, Victor Walker, Director Bluffs Business Center, 1517 Broadway, Suite 122, Scottsbluff, NE 69361, 308-635-0851 Fax: 308-635-2321 Toll Free: 800-682-5140, www.aown.org Iowa Community Resources Many patients and families are not aware of state and local community resources. Generally some are listed in the phone book, or the patient can call the local hospital or their physician’s office also. American Association of Retired Persons (AARP) 888-687-2277 Offer not only discounts on auto and some health insurance plans, provides access to Advocacy in both Washington and individual states; on Medicare, Social security and consumer safety. They can offer some community resource info on local chapters and have a nationwide volunteer network. American Lung Association 800-568-487 American Cancer Society (Iowa) 712-233-1188 American Diabetes Association 800-342-2383 American Heart Association Iowa affiliate 712-255-4798 American Red Cross 712-2524081 Dependent Adult Abuse Iowa 712-255-2699 Iowa Department for the Blind 800-362-2587 Books, cassette tapes and records mailed to the home free of charge to legally blind, visually impaired, or physically disabled persons. Local resources for Siouxland Area Siouxland Aging-works with Adults 60 and over to assist with needs, to help seniors remain independent at home. This agency sets up meal programs such as MOM’s(premade frozen meals that can be reheated at home) Meals on wheels(sliding scale based on income), works with Medicaid waiver programs and provides agencies, to assist with chore services, and bathing services, transportation on transit system and wheelchair bus, and assistance with housing issues. Also provides respite services to caregivers. A social worker is assigned to the older adult and will become an advocate. Phone 712-2796900- www.siouxlandaging.org The Center-works with low income seniors can provide some financial assistance for basic utility bills, food and home repairs. Phone712-252-1861 Iowa Department of Human services- works with low income and disabled adults- waivers, Medicaid, food stamps. Phone 712-255-0833 Non-Medical Private Pay homecare programs-Synergy and Homeinstead. Synergy- www.synergyhomecare.com 712-605-242-6056 and Homeinsteadwww.homeinstead.com/381.Phone 712-258-4267. Lutheran Social Services- Local transportation to physician appointments, groceries. Phone 712-276-1075 References AARP. Retrieved from http://assets.aarp.org/www.aarp.org_/promotions/sem/m ember01.html?keycode=U6TPM1&packageid=&componenti d=&whocalled=promo_enroll&cmp=IVS-KNC-ACQ-PMD-ACQJOIN Aging Partners-City of Lincoln and Lancaster County. (2005-2009). Retrieved from http://lincoln.ne.gov/city/mayor/aging/info.htm#naaa CDC. Medication Safety Program. (2012). Retrieved from http://www.cdc.gov/medicationsafety/ Centers for Medicare and Medicaid Services. Outcome and Assessment Information Set. Retrieved from http://www.cms.hhs.gov/oasis/ Ellenbecker, C., Samia,L., Cushman, M., and Alster, K. (2008). Patient Safety and Quality in Home Health Care. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK2631/ Kozier, B. and Erb, G. (2008). Fundamentals of Nursing. Upper Saddle River, New Jersey: Pearson. Lifeline Medical Alert Service. (2013). Retrieved from http://www.lifelinesys.com/content/home Medical Guardian: Medical Alert Systems. (2013). Retrieved from http://www.medicalguardian.com/ppc-Nebraska-medical-alertsystem.html?gclid=CLOHs4C957gCFSho7Aod8kgA2A References Meiner,S. and Lueckenotte, A. (2006). Gerontologic Nursing 3rd edition. St. Louis, MO: Mosby Inc. NonMedical HomeCare. (2013). Retrieved from http://www.synergyhomecare.com/respite-for-family-caregivers/ Senior Corps. http://www.serve.nebraska.gov/pdf/americorps/nebraskasenior-corps-senior-companions.pdf Siouxland Aging Services. (2009). Retrieved from www.siouxlandaging.org Tabloski, Patricia. (2010). Gerontological Nursing. Upper Saddle River, New Jersey: Pearson. University of Rochester University. Medication Management (2013). Retrieved from http://www.urmc.rochester.edu/encyclopedia/content.aspx ?Conten tTypeID=56&ContentID=DM250 WebMD. Caregiver Burnout.(2005-2013). Retrieved from http://www.webmd.com/healthy-aging/caregiver-burnout Tips.