End of Life Care - RCRMC Family Medicine Residency
advertisement

End of Life Care
Which of the following
is not documented in the Physician
Orders for Life-Sustaining Treatment
Paradigm (POLST) form?
A) Instructions for resuscitation
B) Types of medical interventions
desired
C) Designation of durable power of
attorney for health care
D) Use of artificial nutrition and
hydration
Answer
• C) Designation of durable power of
attorney for health care
Choose the correct criteria for eligibility for
hospice care in a patient with dementia.
Lack of meaningful verbal communication (6 or
fewer words)
Hospitalization for pneumonia, pyelonephritis,
sepsis, or other serious complications in previous
6 mo
Presence of stage 3 or 4 pressure ulcers
Weight loss of ≥5% in previous 6 mo
Total dependence for activities of daily living
A)
B)
C)
D)
1,2,3,4
1,3,4,5
2,3,4,5
1,2,3,5
Answer
1. Lack of meaningful verbal
communication (6 or fewer words)
2. Hospitalization for pneumonia,
pyelonephritis, sepsis, or other serious
complications in previous 6 mo
3. Presence of stage 3 or 4 pressure
ulcers
5. Total dependence for activities of daily
living
•
D) 1,2,3,5
Appetite stimulants may
increase ________ in
patients undergoing
palliative care.
A) Enjoyment of eating
B) Lean body mass
C) Longevity
D) A, B, and C
Answer
• A) Enjoyment of eating
Choose the correct statement about
the benefits of artificial hydration
and nutrition (AHN).
A) AHN can relieve dry mouth
B) Percutaneous endoscopic
gastrostomy (PEG) tubes and total
parenteral nutrition increase patient
comfort
C) AHN may cause dyspnea from
pulmonary edema
D) PEG tubes help prevent
pneumonia from aspiration
Answer
• C) AHN may cause dyspnea from
pulmonary edema
Constipation is the only
side effect of treatment
with opioids for which the
patient does not develop
tolerance.
A) True
B) False
Answer
• A) True
Which of the following
is notuseful for the treatment
of nausea and vomiting
induced by administration of
opioids in the absence of
motility and distention
problems?
A) Haloperidol
B) Diphenhydramine
C) Scopolamine
D) Metoclopramide
Answer
• D) Metoclopramide
Both glycopyrrolate and
scopolamine cross the
blood-brain barrier and
may cause changes in
mental status.
A) True
B) False
Answer
• B) False
Approximately ________
of patients at end of life
suffer from cough.
A) 10%
B) 25%
C) 40%
D) 60%
Answer
• C) 40%
Unlike ________ for
treatment of opioid
induced constipation,
________ does not cause
opioid withdrawal and
reversal of analgesia.
A) Oral naloxone;
methylnaltrexone
B) Methylnaltrexone; oral
naloxone
Answer
• A) Oral naloxone;
methylnaltrexone
Which of the following
statements about
methylphenidate for the
treatment of depression in
patients with terminal illness
is(are) correct?
A) It is the fastest acting
antidepressant
B) It is well tolerated in
geriatric population
C) A and B
D) None of the above
Answer
• C) A and B
An 80-year-old patient is on high
doses of morphine to control pain
and dyspnea at the end of life. Which
one of the following medications is
appropriate for constipation caused
by opioids?
A. Corticosteroids.
B. Naloxone (formerly Narcan).
C. Ketamine (Ketalar).
D. Polyethylene glycol solution
(Miralax).
Answer
• D. Polyethylene glycol solution (Miralax).
A 78-year-old woman with terminal
breast cancer has been vomiting. She
complains of feeling anxious and
fearful about her rapid decline in
function. Which of the following
antiemetic medications is/are most
appropriate?
A. Benzodiazepines.
B. Cannabinoids.
C. Antihistamines.
D. Dexamethasone.
Answer
• A. Benzodiazepines.
B. Cannabinoids.
An 85-year-old man with severe
pneumonia is rapidly declining and
is not responding to antibiotics.
Which of the following actions can
help prevent delirium?
A. Keeping familiar persons at the
bedside.
B. Limiting medication changes.
C. Limiting unnecessary
catheterization.
D. Using wrist restraints.
Answer
• A. Keeping familiar persons at the bedside.
B. Limiting medication changes.
C. Limiting unnecessary catheterization.
What should the dose of
the pain medication be for
breakthrough pain? What
% of the 24 hour dose q 1
hour?
Answer
• 10 to 20%
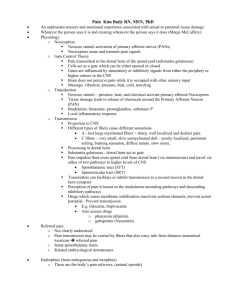
PALLIATIVE AND END-OFLIFE CARE
• Approach to discussion: study of
interaction between hope and desire for
prognostic information among 55 patients
with terminal disease;
• 4 patterns—feelings swing between totally
hopeful and completely discouraged (amount
of information desired depended on stage)
• scales and balance (hopeful but realistic
• wanted information but not too much)
• yin-yang (hope and bad news coexisted)
• Redirected hope (from hope for cure to other
things, eg, survive to certain date)
• ask all patients how much information they
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Advance
directive
Five Wishes form—includes designation of durable
power of attorney (DPOA) for health care
Type of medical treatment desired
degree of comfort desired
desired treatment
level of information shared with loved ones
does not direct paramedics about wishes regarding
code
Physician Orders for Life-Sustaining Treatment
Paradigm (POLST) form
provides instructions for resuscitation
types of medical interventions
use of antibiotics
artificial nutrition and hydration
does not designate DPOA
living will registry—available in Washington
patient sends copy of documents to central database
•
The Five Wishes
Wishes 1 and 2 are both legal documents. Once signed, they meet the legal
requirements for an advance directive in the states listed below. Wishes 3, 4 and
5 are unique to Five Wishes, in that they address matters of comfort care,
spirituality, forgiveness, and final wishes.
Wish 1: The Person I Want to Make Care Decisions for Me When I Can't
This section is an assignment of a health care agent (also called proxy, surrogate,
representative or health care power of attorney). This person makes medical
decisions on your behalf if you are unable to speak for yourself.
Wish 2: The Kind of Medical Treatment I Want or Don't Want
This section is a living will--a definition of what life support treatment means to you,
and when you would and would not want it.
Wish 3: How Comfortable I Want to Be
This section addresses matters of comfort care--what type of pain management you
would like, personal grooming and bathing instructions, and whether you would
like to know about options for hospice care, among others.
Wish 4: How I Want People to Treat Me
This section speaks to personal matters, such as whether you would like to be at
home, whether you would like someone to pray at your bedside, among others.
Wish 5: What I Want My Loved Ones to Know
This section deals with matters of forgiveness, how you wish to be remembered and
final wishes regarding funeral or memorial plans.
Signing and Witnessing Requirements
The last portion of the document contains a section for signing the document and
having it witnessed. Some states require notarization, and are so indicated in
the document.
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Discussing palliative care
with patients
Timing
at time of diagnosis of life-limiting disease
if physician expects patient’s death in next 6 to 12 mo
if patient has frequent hospital admissions
if chronic disease progresses
if patient with chronic untreatable disease presents with lifethreatening event
that could allow natural death
set safe context for discussion
open with questions about patient’s goals for their experience
questions—identify stakeholders
ask about patient’s understanding of situation
sources of strength,
Hopes
Fears
past experiences with serious illness
keys to successful discussion
allowing patient and family time to speak increases patient satisfaction and
helps reduce anxiety, posttraumatic stress disorder (PTSD), and depression
among family members
Try to aim for 66/34 with patient family 66% of talking
Hospice eligibility for
patients with dementia
• criteria include
• total dependency for activities of daily living
(ADLs)
• lack of meaningful verbal communication (6
or fewer words)
• hospitalization for pneumonia, pyelonephritis,
sepsis, or other serious complication in
previous 6 mo
• stage 3 or 4 pressure ulcers
• loss of 10% of body weight in previous 6 mo
• patient must have any 3
Benefits of hospice:
• nurse on-call 24 hr/day
• skilled hospice certified nursing
assistant (CNA)
• spiritual support
• Comprehensive emotional and grief
support, with special programs for
children
• hospice volunteers
Anorexia
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
obtain history and laboratory or radiographic data (if appropriate), and perform physical examination to seek
cause
if possible, treat underlying cause (eg, reflux, constipation)
appetite stimulants—options
alcohol,
Steroids
Megestrol
delta-9-tetrahydrocannabinol,
Androgens
do not increase lean body mass or longevity
may provide patients with enjoyment of eating
Artificial hydration and nutrition (AHN)
ask about patient’s goals
during nutritional deficiency
central nervous system endorphins may cause mild euphoria
intravenous (IV) fluids do not relieve dry mouth
Percutaneous endoscopic gastrostomy (PEG) tubes and total parenteral nutrition (TPN) do not prolong life
may increase suffering (eg, dyspnea from pulmonary edema or ascites
pneumonia from aspiration
discomfort from tube or IV
possible need for restraints in patients with dementia, loose stools)
appropriate for patients with malignancies of head and neck or upper gastrointestinal tract who are having
definitive surgery or receiving radiation or chemotherapy
selected ambulatory patients (eg,
patients with HIV)
patients with amyotrophic lateral sclerosis (ALS)
for patients with dementia, tube feeding does not prolong survival, prevent aspiration, Improve pressure
ulcers, improve function, or give comfort
Anorexia
• Study results
• not randomized
• median survival of 59 days among 23
patients who received PEG
• 60 days among 18 patients who did not
• Family concerns: encourage alternative
activities to show care for patient
• in case of conflicting wishes, perform
therapeutic trial of feeding tube for specific
time (eg, 3 days)
• Reassess
Questions and answers
•
•
•
•
•
•
•
•
•
•
•
•
•
Letter of condolence: difficult but appreciated by family
Questions and answers: why does POLST form have full
resuscitation option?
allows patient to specify wishes for other measures, eg, AHN
also, documentation of wish for resuscitation on POLST form indicates
that patient has discussed their wishes for this option
can duration of hospice exceed 6 mo?
yes; most groups follow Medicare guidelines, which require that
attending physician expects patient’s death within 6 mo
patient’s condition re-evaluated at 90 days after admission and every
60 days thereafter
patient may remain in hospice as long as expectation of death within 6
mo remains after these evaluations
some insurance companies pay only for specific period
many hospices provide charity care afterwards
do gastroenterologists believe that PEG tubes prevent aspiration?
literature does not support conclusion that PEG tubes that end in
stomach prevent aspiration
Tubes that terminate in jejunum may prevent aspiration
•
•
•
•
•
•
•
•
Letter of condolence
The benefit of writing a letter of condolence as twofold: to be a source
of comfort to the survivors and to help clinicians achieve a sense of
closure about the death of their patient. In the sidebar on the
previous page, Dr Mark Geliebter, Martinez, CA, describes how he
began writing letters of condolence to his patients and the value this
practice has had for him.
If you decide that writing a letter of condolence is a practice you
would like to begin incorporating into your medical practice, the
following guidelines, adapted from Wolfson and Menkin's "Writing a
condolence letter,"3 may be helpful.
Address the family member. Dear Mrs Wagner, ...
Acknowledge the loss and name the deceased. Dr Murphy and I were
deeply saddened today when we learned from your hospice nurse Lois
that your mother, Ruth Smith, had died.
Express your sympathy. We are thinking of you and send our heartfelt
condolences.
Note special qualities of the deceased. It seems like only yesterday
that Ruth talked about her love of card playing. I admired her energy
and quick wit.
Note special qualities of the family member. I was deeply moved by
the devotion you and your family showed during the period of Ruth's
final illness. Your concern was one indication of your love for her.
Although she was a fiercely independent woman, I know she
appreciated your involvement and help.
End with a word or phrase of sympathy. With affection and deep
sympathy, we hope that your fond memories of Ruth will give you
comfort.
Doctors and Sympathy Cards
By Mark Geliebter, MD
•
•
•
•
As soon as the Code Blue ends in the emergency department all of the housestaff scatter. During my training, I
was always struck by how quickly the doctors would leave the scene as soon as the patient was pronounced
dead. There was no lingering--as if no one wanted to stay in the room with the dead person. The strategy
seemed to be to create physical distance from any associated feelings of failure as a doctor. There was no ritual
to follow at the end of an unsuccessful resuscitation effort. There was never any discussion about the ritual of
death. We would spend weeks and weeks discussing the Krebs molecular "life cycle" in medical school.
However, discussions about the natural cycle of life and death were rare. After practicing internal medicine for
many years at Martinez, CA, I was struck by my own lack of closure when my patients died. I too would not
hover at the bedside when a patient of mine had died. I would not routinely connect with family members after
a death. Many years ago, I became involved in physician wellness efforts at my facility and regionally. I realized
that exploring our own relationship with death and dying was a key element in physician well-being.
One of the outcomes of that exploration was the decision to start a new practice for myself in 1995. I began to
list the name of every patient of mine who died. I generally would include a diagnosis, medical record number,
date and place of death. I started a folder labeled "Death and Dying." I also began to send a sympathy card to
each family (I later found these cards available as a KP stock item!).
Initially, I began with brief statements of sympathy. More recently, I've been writing more personal comments,
especially when I've had a longer relationship with the person or their family. I frequently mention that I felt
privileged to have been their physician. I also try to call the families that I feel connected to. I have received
frequent positive feedback from families for my personal note or call. They are most appreciative of my
thoughtful acknowledgments.
This has created a ritual practice for myself at the time of a patient's death. It also gives me a way to remember
my patients. When I review my list, I can usually remember something about them, their faces, their
personalities, or some ethical or medical issues that may have been challenging. Even after many years, the list
elicits those memories. I would have totally forgotten many patients that had died if it weren't for my list. At
times, it reminds me of memorial plaques on some synagogue or other walls that list names of members or
their families who have died. Sending the sympathy card and making the follow-up phone calls have become
part of my own sense of responsibility as a physician. It helps obviate the need to run out of the room after an
unsuccessful Code Blue, as I did when a medical student. Integrating the reality of death; embracing it as a
natural process; developing coping strategies; not labeling death as failure; finding rituals; doing outreach
during and after the dying process are all part of our role as physicians. All of these insights and rituals will add
to our own personal wisdom of dealing with the inevitability of our patients' and our own deaths.
Example Condolence Letter
•
•
•
•
•
•
•
•
•
•
•
Below is an example of a condolence letter using the seven components above:
Dear_____________,1. Acknowledge the loss, refer to deceased by name.
I was deeply saddened to hear about the death of _____________.
2. Express your sympathy.
I know how difficult this must be for you. You are in my thoughts and prayers.
3. Note special qualities of the deceased.
____________was such a kind, gentle soul. She would do anything to help
someone in need.
4. Include your favorite memory.
I remember one time_________________.
5. Remind the bereaved of their personal strengths and qualities.
I know how much you will miss_______________. I encourage you to draw on
your strength and the strength of your family. You could use your special talent
of scrapbooking to make a lasting memory book of _________________.
6. Offer specific help.
I can come over on Tuesday evenings to help you make your scrapbook. I have
some lovely pictures of _______________ I’d love to share.
7. End the letter with a thoughtful closing.
May God bless you and your family during this time and always,
Sign your name_____________________
Keep in mind that this is only an example. Write from your heart and whatever
elements you include will be the right ones.
The next page includes information on writing a shorter version of the
condolence letter: The Condolence Note.
Condolence note
• You may decide to write a shorter version of a condolence
letter on note card or on a small piece of stationary tucked
inside a commercial card. If I am close enough to the
deceased to have photos of them, I especially like to print one
of my favorite photos on a card. That can be done from your
computer or from a picture program in your local photo
developing shop.
• When writing a condolence note, pick just a few elements
from the example on the first page of this article. Using
components #1, 2, 3, and 7 is a good guide.
1. Acknowledge the loss and refer to the deceased by name.
2. Express your sympathy.
3. Note any special qualities of the deceased that come to mind.
4. End the letter with a thoughtful word, a hope, a wish, or
expression of sympathy e.g. "You are in my thoughts" or
“Wishing you God’s peace.” Closing such as "Sincerely," "love,"
or "fondly," aren’t quite as personal.
• Remember that this is just a guide. You can use any of the
components of a condolence letter in your note or none at all.
The most important thing is to write from your heart
A letter by Abraham Lincoln
• Archival communications abound with
outstanding examples of fine letters of
condolence. A letter by Abraham Lincoln to a
girl whose father had died in the Civil War
showed several of the qualities outlined
above8:It is with deep grief that I learn of the
death of your kind and brave Father; and
especially that it is affecting your young heart
beyond what is common in such cases. In this
sad world of ours, sorrow comes to all; and,
to the young it comes with bitterest agony,
because it takes them unawares. The older
have learned ever to expect it.
• Note that Lincoln uses the word death directly
and describes her father as kind and brave.
Years later, one can only imagine how this
A Dying Art?
The Doctor’s Letter of Condolence
Gregory C. Kane, MD, FCCP
•
•
•
In their commentary on writing letters of condolence, Bedell et al5 outlined why
doctors do not regularly write letters of condolence. Potential explanations
included a lack of time, a loss for the appropriate expression of sympathy, a
feeling that they did not know the patient well enough, lack of a specific team
member responsible for writing the letter, or a sense of failure over the death.
No doubt, this has been fostered by a lack of role modeling or broader
discussion of such practices.
In a personal and memorable patient encounter, I sat and listened while a tearful
patient cried at having received no contact from the physician who treated her
husband for metastatic lung cancer for a treatment duration of 9 months. As I
struggled to comprehend her sense of pain and abandonment, I considered
offering as possible explanation that the physician may not have been “on call”
at the time of the death and may have mistakenly believed that his partner had
offered such a gesture verbally. Before I could respond, however, my patient
added that her veterinarian had sent a card when the family dog died. I was
speechless.
Other physicians have shared similar experiences, sometimes involving family
members, friends, or mutual patients. In his convocation speech on becoming
President of the American College of Chest Physicians in 2003, Dr. Richard
Irwin described a vision for patient-centered care. His vision was comprehensive
but also included a discussion of sympathy cards after the death of a patient. He
noted, “when physicians do not acknowledge the deaths of their patients, it is
perceived that physicians are silently saying that the deceased patient was not
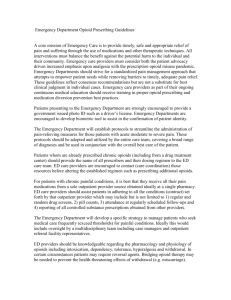
Nausea and vomiting (NV)
• consider possible causes
• Opioids: act on chemotactic trigger zone (rich in dopaminergic
receptors) and on vestibular system (may manifest after
changing position)
• data unclear whether NV side effects similar for all opioids
• patients eventually become tolerant
• constipation only side effect of opioids for which no tolerance
develops
• if NV mild, continue drug until tolerance develops
• if NV severe, rotate to other opioids
• Antiemetics haloperidol, scopolamine (anticholinergic) or
promethazine (Phenergan); antihistamine diphenhydramine
(Benadryl) also works well
• 5HT3 antagonists (eg, ondansetron) not generally helpful for
managing opioid-mediated NV
• Haloperidol most potent antidopaminergic, followed by
prochlorperazine
• promethazine has minimal antidopaminergic properties
• metoclopramide (Reglan) binds few receptors relevant to NV
• useful only for problems with motility and distention
Bowel obstruction
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
most often associated with pelvic cancer, especially ovarian and colon
symptoms include NV and cramping abdominal pain
treatments surgical, interventional, and medical
usually possible to avoid IV and nasogastric tube
Surgical treatment: includes venting gastrostomy tubes for small bowel
obstructions but not for colonic obstructions
Drug therapy: cocktail of opioids, anticholinergic agent, and somatostatin
(octreotide)
opioids—help relieve pain; evidence suggests they do not increase risk for
paralytic ileus
dopamine antagonist—eg, haloperidol; much lower dose (ie, 0.5 to 2 mg every
4-6 hr) of haloperidol required than for psychosis (5 to 10 mg)
spasms; agents include glycopyrrolate or scopolamine
glycopyrrolate administered IV or PO) and does not cross blood-brain barrier or
cause changes in mental status
scopolamine administered by patch and crosses blood-brain barrier
consider prokinetic drugs for partial small bowel obstruction and discontinue if
pain increases
octreotide—inhibits splanchnic blood flow and decreases secretions from
intestinal mucosa to diminish distention
administered IV or subcutaneously
Effective dose usually <400 g/day
Cough
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
highly debilitating; 40% of patients suffer from cough at end of life
drugs associated with cough include
angiotensin-converting enzyme (ACE) inhibitors, nonsteroidal anti-inflammatory
agents (NSAIDs), and propellants in inhaled medications
Treatment: American College of Chest Physicians (ACCP) recommends against
use of prescription and over-thecounter cough syrups
sweet syrups (eg, honey) possibly effective for relief of cough
Opioids first-line therapy for cough in patients with cancer
all opioids have similar effect
for patients already taking an opioid, study suggested low dose of oxycodone
effective a 5 mg po bid
Expectorants consider for wet cough
guaifenesin or inhaled acetylcysteine
avoid in patients with reactive airway disease because of bronchospasm
consider nebulized 3% to 10% hypertonic saline instead
use caution in patients with impaired cough reflex because of risk for aspiration
benzonate—local anesthetic second-line in addition to opioids
anticholinergics—play role if upper airway secretions contribute to cough (eg,
scopolamine and glycopyrrolate);
inhaled lidocaine—(used off-label)
bupivacaine block upper airway stretch receptors
Patients must not eat or drink for 1 hr after inhalation as precaution against
aspiration
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Constipation
experienced by 90% of patients in advanced phases of illness
mostly due to opioids
prevention critical, and all patients on opioids need bowel regimen
Constipation can cause fecal impaction and diarrhea
Digital rectal examination and history important
preventive regimen includes stool softener, eg, docusate (Colace), and stimulant
laxative, eg, senna or bisacodyl (Dulcolax)
add osmotic laxative if necessary
Induced by opioids
tolerance rarely develops
not centrally mediated, limited to gut
previously used oral naloxone (opioid antagonist with poor bioavailability)
However high doses needed cause opioid withdrawal and reversal of analgesia
methylnaltrexone—mu receptor antagonist that works only in gut
given as subcutaneous injection
lower dose works better
in studies, 60% of patients have bowel movement (BM) within 4 hr and 70%
within
first 24 hr
in clinical use, 54% have BM
no tolerance observed
average dose 8 mg (based on weight)
Comes in prefilled syringe
side effects include abdominal cramping, gas, and diarrhea
Metastatic bone pain
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
almost 500,000 new patients per year
often associated with cancers of lung, breast, and prostate and multiple myeloma
goals of treatment include
control of pain and prevention of fractures
Medical therapy: consider calcitonin because of low risk, although often not efficacious, and
effect short-lived when present
opioids—effective only 50% of time
NSAIDs—treat inflammation in bone
avoid indomethacin in elderly patients because of associated CNS toxicity and mental status
changes
ibuprofen (eg, Motrin) at anti-inflammatory doses (ie, 600 to 800 mg/day)
corticosteroids—mechanism similar to that of NSAIDs
dose not standardized
prednisone and dexamethasone (eg, Decadron) most commonly prescribed
Dexamethasone used at 16 to 32 mg/day for bone pain
start at 2 to 4 mg twice daily because of dose-limiting toxicity
Discontinue if not effective after 7 days at 16 to 24 mg
prednisone used at 30 to 40 mg/day
dexamethasone has lower mineralocorticoid activity than prednisone
bisphosphonates—(eg, zoledronic acid and pamidronate) decrease bone pain
most effective in breast and prostate cancer
inhibit bone resorption by osteoclasts
reduce number of fractures and skeletal events by 30%
reduce pain by 30% to 40% in 30% to 50% of patients
effects last 3 to 4 wk
if first infusion not effective, try second infusion, but if still ineffective, discontinue for pain
(may continue for fractures)
Metastatic bone pain
• Radiation therapy: effects on pain seen in 2 days to 2
weeks
• limited by number of areas affected by metastasis
• Radiopharmaceuticals: Strontium, best evidence for
efficacy in breast and prostate cancer; helpful with
multiple foci of metastasis
• improve pain in 30% of patients
• patient must have >12 wk of life remaining
• analgesia occurs as soon as 3 days, usually 2 wk
• worsened pain (flare) within first week because of
inflammatory effect (actually good prognostic sign)
• myelosuppression can occur (cancer patients who
already have myelosuppression from tumor not
candidates)
• Neuropathic bone pain: component of bone pain
• early data show benefit of gabapentin (Neurontin) or
Psychiatric symptoms
•
•
•
•
•
•
•
•
•
•
•
•
•
•
depression not part of dying but manageable symptom
antidepressants can help achieve better pain control
anxious depression often misdiagnosed as anxiety disorder
methylphenidate—fastest acting antidepressant
appropriate for patients with life expectancy of weeks
response observed within 1 or 2 doses
well tolerated in geriatric population
begin dose at 2 to 5 mg once daily and add 2.5 mg if no effect
ultimately may need only 5 mg twice daily
duloxetine (Cymbalta) and venlafaxine (Effexor) appropriate for patients
with depression and neuropathic pain
fluoxetine and venlafaxine appropriate to activate patients with
psychomotor retardation
Mirtazapine (Remeron) useful for depression with insomnia
Also stimulates appetite in patients without severe depression when
given at 7.5 mg at night
citalopram, escitalopram, and paroxetine helpful for depression with
anxiety
Suggested Reading
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Abernethy AP et al: Detailing of gastrointestinal symptoms in cancer
patients with advanced disease: new methodologies, new insights,
and a proposed approach. Curr Opin Support Palliat Care 3:41,
2009; Al-Khafaji A, Min Cho S: Making palliative care more “palatable.”
Crit Care Med 37:2492, 2009; Biermann JS et al: Metastatic
bone disease: diagnosis, evaluation, and treatment. J Bone Joint
Surg Am 91:1503, 2009; Dalal S et al: Is there a role for hydration at
the end of life? Curr Opin Support Palliat Care 3:72, 2009; Desandre
PL, Quest TE: Management of cancer-related pain. Emerg Med
Clin North Am 27:179, 2009; Di Giulio P et al: Dying with advanced
dementia in long-term care geriatric institutions: a retrospective
study. J Palliat Med 11:1023, 2008; Guay DR: Methylnaltrexone
methobromide: the first peripherally active, centrally inactive opioid
receptor-antagonist. Consult Pharm 24:210, 2009; Innes S, Payne S:
Advanced cancer patients’ prognostic information preferences: a review.
Palliat Med 23:29, 2009; Jacobsen J, Jackson VA: A communication
approach for oncologists: understanding patient coping and
communicating about bad news, palliative care, and hospice. J Natl
Compr Canc Netw 7:475, 2009; Kierner KA et al: Attitudes of patients
with malignancies towards completion of advance directives.
Support Care Cancer May 31, 2009 [Epub ahead of print]; MessingerRappaport BJ et al: Advance care planning: Beyond the living
will. Cleve Clin J Med 76:276, 2009; Monturo C: The artificial
nutrition debate: still an issue … after all these years. Nutr Clin Pract
24:206, 2009; Phelps AC et al: Religious coping and use of intensive
life-prolonging care near death in patients with advanced cancer.
JAMA 18:301, 2009; Price A, Hotopf M: The treatment of depression
in patients with advanced cancer undergoing palliative care.
Curr Opin Support Palliat Care 3:61, 2009; Rondeau DF, Schmidt
TA: Treating cancer patients who are near the end of life in the emergency
department. Emerg Med Clin North Am 29:341, 2009; Sanft
TB, Von Roenn JH: Palliative care across the continuum of cancer
care. J Natl Compr Canc Netw 7:481, 2009; Wee B: Chronic cough.
Curr Opin Support Palliat Care 2:105, 2008; Wright AA et al: Associations
between end-of-life discussions, patient mental health,
medical care near death, and caregiver bereavement adjustment.
JAMA 300:1665, 2008; Zaider T, Kissane D: The assessment and
management of family distress during palliative care. Curr Opin Support
Palliat Care 3:67, 2009.
dyspnoea
• Breathlessness or dyspnoea is the
unpleasant awareness of difficulty
in breathing
• dyspnoea, like pain, is subjective and
involves both the perception of
breathlessness and the reaction of the
patient to it
• dyspnoea is always associated with
some degree of anxiety, which in turn
will make the breathlessness worse
Treatment
• treatment directed at the specific
cause, where possible and appropriate
• general measures
• calm, reassuring attitude
• nurse patient in position of least
discomfort
• physiotherapy
• improve air circulation
• distraction therapy
• relaxation exercises
• breathing control techniques
• counselling
Is O2 saturation is a good
measure of dyspnea?
• True
• False
Answer
• False
• Dyspmea is a subjective symptom
Treatment
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
oxygen
if hypoxic
if it improves symptoms (terminal care situation)
Patients often feel better but it may be just do to movement of air on the face
A fan or open window may help just as much in certain situations
bronchodilators if there is a reversible element to the bronchial obstruction
corticosteroids
effective bronchodilators
for dyspnoea due to multiple metastases, lymphangitis carcinomatosis and
pneumonitis
opioids—the most useful agents in the treatment of dyspnoea
nebulised morphine
effective for some patients, although controlled studies do not support its use
risk of bronchospasm
aid expectoration
steam, nebulised saline
mucolytic agents
expectorants
Physiotherapy
reduce excess secretions
anticholinergics
antitussives if dyspnoea exacerbated by coughing
anxiolytics
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Examples of drug therapy
bronchodilators
salbutamol by metered aerosol or 2.5-5 mg by nebuliser, q4-6h
ipratropium by metered aerosol or 250-500 µg by nebuliser, q6h
aminophylline, theophylline PO
corticosteroids
prednisolone 40-60 mg/d PO or dexamethasone 8-12 mg/d PO
wean to the minimum effective dose after a few days
opioids
morphine 5-10 mg PO, q4h or 4-hourly PRN and titrate
50% increase in dose for patients on morphine for pain
nebulised morphine not recommended
anxiolytics
diazepam 2 mg PO q8h ± 5-10 mg nocte
alprazolam 0.25-0.5 mg SL, q1-2h
lorazepam 0.5-1 mg SL, q4-6h
mucolytics (for sputum retention)
humidified air (steam, nebulised saline)
acetylcysteine 10%, 6-10 ml by nebuliser, q6-8h
anticholinergics (for excessive secretions)
glycopyrrolate 0.2-0.4mg SC q2-4h or 0.6-1.2mg/24h CSCI
hyoscine hydrobromide 0.2-0.4mg SC q2-4h or 0.6-1.2mg/24h CSCI
Terminal Care
treatment should be purely symptomatic in the last week or days of life
investigations should be avoided
antibiotic therapy is usually not warranted
if of benefit, bronchodilator therapy can be continued by mask.
unconscious patients who still appear dyspnoeic should be treated with
morphine SC
TERMINAL RESPIRATORY
CONGESTION
('DEATH RATTLE')
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Terminal respiratory congestion is the rattling, noisy or gurgling respiration of
some patients who are dying
Cause
accumulation of pharyngeal and pulmonary secretions in patients who are unconscious or
semi-conscious and too weak to expectorate
Treatment
therapy is often more for the comfort of the relatives and other patients, as most
of the patients are no longer aware of their surroundings
position the patient on their side
oropharyngeal suction should be reserved for unconscious patients
anticholinergic drugs to suppress the production of secretions
hyoscine hydrobromide
0.4mg SC, ± repeat at 30min, then q2-4h or 0.6-1.2mg/24h CSCI
antiemetic; sedative; occasional agitated delirium
glycopyrollate
0.2-0.4mg SC, ± repeat at 30min, then q4-6h or 0.6-1.2mg/24h CSCI
less central and cardiac effects
atropine
0.4-0.8mg SC q2-4h
may cause tachycardia after repeated injections
transdermal scopolamine patches
hyoscine hydrobromide 1.5mg patch q72h
onset of action is delayed for several hours during which other anticholinergic treatment
needs to be given
reassure relatives that the noisy breathing is not causing any added suffering for
the patient
•
Pharmacologic Pearls for
End-of-Life Care
As death approaches, a gradual shift in emphasis from curative and life
prolonging therapies toward palliative therapies can relieve significant
medical burdens and maintain a patient's dignity and comfort.
• Pain and dyspnea are treated based on severity, with stepped
interventions, primarily opioids.
• Common adverse effects of opioids, such as constipation, must be treated
proactively; other adverse effects, such as nausea and mental status
changes, usually dissipate with time.
• Parenteral methylnaltrexone can be considered for intractable cases of
opioid bowel dysfunction.
• Tumor-related bowel obstruction can be managed with corticosteroids and
octreotide.
• Therapy for nausea and vomiting should be targeted to the underlying
cause; low-dose haloperidol is often effective.
• Delirium should be prevented with normalization of environment or
managed medically. Excessive respiratory secretions can be treated with
reassurance and, if necessary, drying of secretions to prevent the
phenomenon called the "death rattle."
• There is always something more that can be done for comfort, no matter
how dire a situation appears to be.
• Good management of physical symptoms allows patients and loved ones
the space to work out unfinished emotional, psychological, and spiritual
issues, and, thereby, the opportunity to find affirmation at life's end.
Clinical recommendation
•
Opioids should be used for dyspnea at the end of life.
• A
• Multiple studies have shown that nebulized opioids have no benefit over
systemic administration in terms of effect or adverse effects.
• Opioids should be used for pain at the end of life.
• C
• The ethical limitations of withholding opioids have limited the study of
opioids versus placebo, except in neuropathic pain.
• Stimulant laxatives are effective for prevention and treatment of
constipation in persons on opioids.
• C
• There is no clear benefit of one regimen over another.
• Methylnaltrexone (Relistor) can be used for treatment of opioid bowel
dysfunction.
• B
• Methylnaltrexone has recently been added as a treatment option.
• Corticosteroids can be used for malignant bowel obstruction.
• B
• Haloperidol (formerly Haldol) is effective for nausea and vomiting.
• B
• 34, 35
• Hyoscyamine (Levsin) should be used for the "death rattle" (excessive
respiratory secretions).
• C
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
•
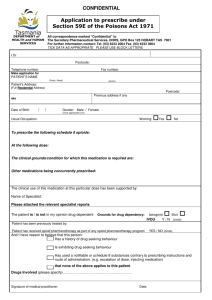
Methylnaltrexone (Relistor)
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use
RELISTOR safely and effectively. See full prescribing information for
RELISTOR.
RELISTOR (methylnaltrexone bromide) Subcutaneous Injection
Initial U.S. Approval: 2008
————————— INDICATIONS AND USAGE —————————
RELISTOR is indicated for the treatment of opioid-induced constipation in
patients with advanced illness who are receiving palliative care, when
response to laxative therapy has not been sufficient. Use of RELISTOR
beyond four months has not been studied. (1)
——————— DOSAGE AND ADMINISTRATION ———————
RELISTOR is administered as a subcutaneous injection. The usual schedule is
one dose every other day, as needed, but no more frequently than one dose in
a 24-hour period. (2.2)
The recommended dose of RELISTOR is 8 mg for patients weighing 38 to
less than 62 kg (84 to less than 136 lb) or 12 mg for patients weighing 62 to
114 kg (136 to 251 lb). Patients whose weights fall outside of these ranges
should be dosed at 0.15 mg/kg. See the table below to determine the correct
injection volume. (2.2)
Patient Weight
Pounds Kilograms
Injection
Volume Dose
Less than 84 Less than 38 See below* 0.15 mg/kg
84 to less than
136
38 to less than 62 0.4 mL 8 mg
136 to 251 62 to 114 0.6 mL 12 mg
More than 251 More than 114 See below* 0.15 mg/kg
*The injection volume for these patients should be calculated using one of
the following (2.2):
Multiply the patient weight in pounds by 0.0034 and round up the
volume to the nearest 0.1 mL.
Multiply the patient weight in kilograms by 0.0075 and round up
the volume to the nearest 0.1 mL.
In patients with severe renal impairment (creatinine clearance less than
30 mL/min), dose reduction of RELISTOR by one-half is recommended. (8.6)
——————— DOSAGE FORMS AND STRENGTHS ———————
12 mg/0.6 mL solution for subcutaneous injection in a single-use vial. (3)
—————————— CONTRAINDICATIONS —————————
RELISTOR is contraindicated in patients with known or suspected
mechanical gastrointestinal obstruction. (4)
——————— WARNINGS AND PRECAUTIONS ————————
If severe or persistent diarrhea occurs during treatment, advise patients to
discontinue therapy with RELISTOR and consult their physician. ( 5.1)
—————————— ADVERSE REACTIONS ——————————
The most common (> 5%) adverse reactions reported with RELISTOR are
PAIN AND DYSPNEA
•
Pain and dyspnea are treated based on severity, with stepped
interventions, primarily opioids.
• Dyspnea that persists despite optimal respiratory treatment is
sensed in the same central nervous system structures as pain and
should be considered as if it were "lung pain."
• Moderate to severe dyspnea and pain may be treated with oral or
parenteral opioids.1,6,7
• Proven nonpharmacologic strategies should be optimized.8
• Using one of many validated scales, physicians can support
patients' efforts to set realistic goals for function and pain or
dyspnea levels.
• Recommended scales should include assessment of intensity and
quality of pain, as well as function.
• Scales that include a nonverbal 0 to 10 line, faces scales, and
intensity descriptive scales have proven reliable in persons with
Mini-Mental State Examination scores averaging as low as 15.3
out of 30.9
• For nonverbal patients, other scales, such as the Pain
Assessment in Advanced Dementia scale, are necessary
•
Pain Control
Nonopioid pain therapies should be optimized; nonsteroidal antiinflammatory drugs, steroids, and bisphosphonates are particularly
effective for bone pain.1,4,6
• A variety of medications are also available for neuropathic pain, a subject
beyond the scope of this article.
• The fear that opioids will hasten death is an inappropriate barrier to their
use, assuming proper dose initiation and escalation are used.11
• Opioids are a central part of pain treatment in palliative care, including
treatment of nonmalignant and neuropathic pain.12
• Titration for effective pain management should be rapid and consistent,
using parenteral or oral short-acting medications, with dosing intervals set
according to peak effects rather than duration of action.13
• Breakthrough dosing must be proportionate to the total 24-hour dose of
opioids.
• It should be 10 to 20 percent of the 24-hour oral morphine equivalent (or 50
to 150 percent of the hourly intravenous rate).
• A common error is the administration of 5 to 10 mg of oxycodone
(Roxicodone) for breakthrough pain when a patient is tolerating high longacting doses.
• For example, if a patient requires 1,000 mg of oral morphine equivalent
every 24 hours, the appropriate breakthrough dose would be 60 to 120 mg
of oxycodone.
• Breakthrough doses should treat unpredictable spikes in pain and prevent
breakthrough pain when predictable, such as before necessary turning or
transfers. Increases in the basal dose should be 25 to 50 percent for mild
to moderate pain and 50 to 100 percent for severe pain.
Pain Control
•
To control symptoms, breakthrough doses should be administered each time an increase in a basal
dose is initiated.
•
Preparations that combine an opioid with acetaminophen, aspirin, or ibuprofen should be avoided
because of the risk of toxicity above established dose ceilings of the nonopioid.14
•
Many patients with terminal illnesses and their families are reluctant to begin opioid therapy
because of the stigma associated with addiction.
•
Preparatory reassurance, education of the patient and family, and use of the term "opioids" instead
of "narcotics" helps.
•
If a persistent objection is raised to initiating one opioid, another can be substituted.
•
Failure of one opioid at the highest tolerated dose may be treated by rotation to another opioid.
•
Reduce dose equivalents by 50 to 75 percent when rotating opioids in the context of well-controlled
pain to compensate for incomplete cross-tolerance.
•
Dose ceilings of opioids are variable and often high.
•
Methadone is among the most difficult and dangerous to use, but has advantages in cost and
effectiveness. Physicians should consider consultation with a palliative care specialist before using
methadone, unless they are familiar with its interactions, variable duration of effect, adverse
effects, unique comparative potency with morphine, and risk of toxicity, including QT interval
prolongation.
•
The New Hampshire Hospice and Palliative Care Organization's opioid use guidelines
(http://www.nhhpco.org/opioid.htm) provide a quick reference card that reviews opioid
management and includes equianalgesic tables, opioid rotation guidelines, and a methadone and
morphine nomogram.13
•
Common causes of a partial response or lack of response to opioids include: neuropathic pain;
social, psychological, or spiritual pain; substance use disorders; and misinterpretation of
symptoms for pain, particularly in persons who are cognitively impaired.
•
Sometimes, aggressive therapies for pain control, such as surgery, radiation, regional nerve blocks,
and intraspinal or epidural delivery devices, are appropriate and necessary when basic measures
fail and interventions are consistent with patient goals.
•
Throughout treatment, physicians must evaluate the "total pain syndrome" and align treatment with
the causes of pain as much as possible, optimizing psychological, social, and spiritual treatments
and avoiding inappropriate pharmacologic management of psychosocial or spiritual pain.
Opioids
•
•
•
•
•
Steps to Rotate or Change Opioids
1. Calculate 24 hr dose of current drug.
2. Translate that to equianalgesic 24 hr dose of oral morphine.
3. Calculate 24 hr equianalgesic dose of new drug and reduce dose to
50-75% of calculated dose if pain is well controlled; use 100%
otherwise.
4. Divide to attain appropriate interval and dose for new drug.
5. Always have breakthrough dosing available while making changes.
Breakthrough Dosing (immediate release (IR) / short acting meds
only)
50-150% of IV basal dose q15 minutes OR 10-20% of 24 hr oral
dose q1hr.
Changing Basal Rates (due to inadequate baseline pain control)
Increase rate by 50-100% of IV basal rate q15 minutes.
Give a breakthrough dose each time basal rate is increased.
Ceiling Effect = uncontrollable pain with appropriate increases in
dose OR side effects such as neuroexcitation, myoclonus, or
protracted central effects.
a) Rotate to another opioid as above.
b) Dose reduce opioid by 25-50% with addition of other treatment for
pain.
c) Treat side effect +/- dose reduce.
Partial Reversal with Naloxone: ONLY for overdose in rare cases:
à mix 0.4 mg amp with saline to make 10cc + administer 0.5 -1 ml
(0.02-0.04 mg) IV/SC q2-5 minutes until response; naloxone effect
shorter in duration than long acting opioids and close monitoring +/-
METHADONE
•
•
•
METHADONE
CAUTION: Use only with experience or training in pain mgt.
- Dosing interval is titrated for analgesic effect q4-12h; start
with q8h.
- Delayed side effects @ Day 4 after initiation: highly lipid
soluble with potential delayed and prolonged side effects that
outlast analgesic efficacy.
- Prolonged QT at high dose>200 mg/day; interactions at
CYP450 (esp 2D6, 3A4)
- Common drugs that increase methadone effect: SSRI’s
(fluoxetine), TCA’s (amitriptyline), macrolides, metronidazole,
grapefruit juice.
- Decrease methadone effect: antiretrovirals, carbamazepine,
rifampin, phenytoin.
Rotation to Methadone
Day 1: Calculate dose (above). Give 33% methadone dose +
66% of present drug.
Day 2: Give 66% methadone dose + 33% present drug.
Day 3: Give 100% methadone dose.
Rotation from Methadone
Caution: Ratios above do not necessarily apply – consult an
Transdermal Fentanyl
• Rotating to and from Transdermal
Fentanyl (TDF)
Shortcut: Transdermal Fentanyl
(mcg/hr) X 2 = approx 24 hr dose of
MS PO(mg).
From TDF: Start new drug at 50% dose
for 6-24 hrs after removal of TDF.
To TDF: Continue old drug at 50% dose
for 6-24 hrs after starting TDF.
Bowel Routine
• Bowel Routine
All patients on opioids should be on a baseline bowel
routine such as one or more of the following:
Senna + docusate (Senokot S) 1-2 tabs twice daily.
MOM 30-60 cc twice to three times daily.
Lactulose 30-60 cc twice to three times daily.
PEG solution: Miralax 1-4 T daily or 4-8 oz of
GoLytely titrated to effect.
• STEP UP: If symptoms of constipation, lack of BM for
specified period of time, or risk factors present such as
immobilization, hospitalization, significant increase in
opioids:
Double dose of regimen above OR add 2nd agent
such as Lactulose or Miralax.
RECTAL IMPACTION or significant rectal stool:
Empty rectum first with:
Bisacodyl 10 mg pr bid for 1-3 days or Fleet or other
enemas until clear. Then proceed with stepped up bowel
regimen as above.
Opioid Adverse Effects
•
Nausea and vomiting, sedation, and mental status changes are common with opioid initiation and
most often fade within a few days.
•
When initiating an opioid, prophylactic use of an antiemetic for three to five days can be effective
in the susceptible patient.15
•
Persistent nausea and vomiting is related to chemoreceptor trigger zone stimulation, and can be
treated with a combination of dose reduction, opioid rotation, and antiemetics.16
•
Undesirable sedation can be addressed with low-dose methylphenidate (Ritalin), which can be
rapidly tapered when no longer needed.17
•
Allergy to opioids usually amounts to nothing more than sedation or gastrointestinal adverse
effects, and can be managed expectantly.
•
Localized urticaria or erythema at the site of an injection of morphine is caused by local histamine
release and is not necessarily a sign of systemic allergy.
•
Constipation is one adverse effect of opioids that does not extinguish with time (Table 2).18 An
important principle of pain management is that, when writing opioid prescriptions, physicians also
need to write orders for the bowel preparation. Increasing fiber or adding detergents (e.g., forms of
docusate) is not sufficient.
•
Like pain, constipation is more easily prevented than treated. Start a conventional combination of a
stimulant laxative with a stool softener (e.g., senna with docusate) or osmotic agent (e.g.,
polyethylene glycol solution [Miralax]) at the same time as the opioid.19
•
There is no good evidence of superiority of any one regimen over another.20 Polyethylene glycol
solutions are easy to titrate, with no maximal dose; can be given once daily; and are particularly
effective with the addition of a stimulant, such as senna.
•
With increases in opioid dose, or with other risks of worsening constipation (e.g., change in
environment, declining performance status), the laxative dose should be doubled or therapy
stepped up by adding a stronger agent.
•
Dosing can be ordered with the notation "hold for diarrhea" or a stepped action plan can be
developed based on consistency and frequency of stool.
•
Overflow diarrhea can occur with fecal impaction. Patients nearing death decrease their intake of
solids, which is often expected to cause the cessation of bowel movements.
•
However, 70 percent of the dry weight of stool consists of bacteria, so bowel activity can and
should be maintained for comfort.21
Treatment of Constipation
• Treatment
• Dosage
• Lactulose
• 15 to 30 mL orally two or three times per day
• Magnesium hydroxide
• 30 to 60 mL orally at bedtime
• Polyethylene glycol (Miralax)
• One or more tablespoons dissolved in 4 to 8 oz of fluid
orally per day
• Senna with docusate
• One to two tablets orally two to four times per day
Opioid Side Effects
•
Opioid bowel dysfunction that is unresponsive to aggressive conventional
medications, removal of anticholinergic or other contributing medications, enemas,
opioid dose rotation, and opioid reduction may be carefully treated with
methylnaltrexone (Relistor).22
•
It reverses mu-opioid receptor-mediated bowel paralysis without crossing the bloodbrain barrier.
•
In a recent industry-sponsored phase 3 trial, subcutaneous methylnaltrexone at 0.15
mg per kg led to a bowel movement within four hours in 48 percent of terminally ill
patients with opioid bowel dysfunction versus 15 percent with placebo, with a median
time of 45 minutes to first bowel movement versus 6.3 hours with placebo.23
•
A more recent study found a dose of 5 mg to be effective, but did not find a dose
response above 5 mg.24
•
Methylnaltrexone is approved by the U.S. Food and Drug Administration for this
indication.
•
Toxic effects of opioids at higher dose ranges or with rapidly escalating doses
include forms of neuroexcitation, such as hyperalgesia, delirium, and myoclonus.25
•
A common pitfall is to confuse these symptoms with worsening pain and further
escalate the dose, which may worsen neuroexcitation and increase hyperalgesia,
thereby exacerbating total pain.
•
Opioid reduction or rotation, with the addition of adjuncts for pain control, is
indicated instead.
•
Ketamine (Ketalar) can be an effective adjunct in severe cases, but requires
experience or consultation.26
•
Unintentional overdose of an opioid can usually be managed expectantly; however, if
partial reversal is necessary, very low-dose naloxone (formerly Narcan) can be
quickly administered by giving 0.01- to 0.04-mg (or 1.5 mcg per kg) intravenous or
intramuscular boluses every three to five minutes, titrated to respiratory rate or
mental status (mix one 0.4 mg per mL ampule of naloxone with saline to make 10 mL,
which equals 0.04 mg per mL).27
•
Continued close monitoring is necessary because duration of opioid effect may
outlast naloxone.
Bowel Obstruction Nausea
•
•
•
•
•
•
•
•
•
Mechanical bowel obstruction is commonly associated with ovarian28 and colon cancers.29
If this cause is known or suspected, it is acceptable to opt not to proceed to invasive intervention
urgently.30
•
Surgery or venting gastrostomy tube insertion should be undertaken only after careful
consideration, because of potential procedural complications, lack of evidence for life
prolongation, and recurrence rates up to 50 percent.31
Endoscopic bowel stenting can be a reasonable option for esophageal or duodenal obstruction.
•
Standard conservative therapies may include cessation of oral intake, transient nasogastric
suction, antiemetics, octreotide (Sandostatin), and corticosteroids.
•
Octreotide inhibits the accumulation of intraluminal intestinal fluid and can be administered
subcutaneously or intravenously at 50 to 100 mcg every six to eight hours and titrated rapidly to
effect.32
•
It is also available in an intramuscular depot form, but this form costs more.
Dexamethasone six to 16 mg intravenously daily may resolve a bowel obstruction caused by edema
from gastrointestinal or ovarian cancer.33
•
Although there is no change in mortality at one month, a review of 10 trials confirmed that
corticosteroids shrink swelling around the tumor and can allow resumption of oral intake with
reinstatement of normal bowel activity (number needed to treat = 6).33
Tapering off corticosteroids should not be undertaken in this circumstance unless indicated for
other reasons.
Persistent nausea and vomiting (without bowel obstruction) should be carefully investigated and
treatment directed to the underlying cause, most commonly in the central nervous system or the
gastrointestinal tract (Tables 3 and 4).34
If one medication fails, substitute another drug from a different class. Promethazine (Phenergan), a
sedating antihistamine, is relatively ineffective in palliative care and is overused.
As noted in a comprehensive review,34 off-label use of haloperidol (formerly Haldol), a low-cost
antiemetic, can be at least as effective as ondansetron (Zofran).35
It is best used at lower doses than for psychosis and can be combined with other interventions.
Choice of Antiemetic Based
on Cause of Nausea and
Vomiting
•
Cause of nausea and vomiting
• Antiemetic
• Anxiety, anticipatory, psychologic
• Benzodiazepines, canniboids
• Bowel obstruction
• Octreotide (Sandostatin; see text)
• Gastroparesis
• Metoclopramide (Reglan)
• Increased intracranial pressure, central nervous system pain
• Dexamethasone
• Inner ear dysfunction (rare in palliative care)
• Anticholinergics, antihistamines
• Medication (primarily chemotherapy)
• 5-HT3 and dopamine receptor blockers
• Metabolic (e.g., uremia, cirrhosis)
• 5-HT3 and dopamine receptor blockers, antihistamines, steroids
• Opioid bowel dysfunction
• Methylnaltrexone (Relistor)
DELIRIUM AND THE
"DEATH RATTLE"
•
Up to 85 percent of patients experience delirium in the last weeks of life, up 46 percent with
agitation.36
•
It manifests as a sudden onset of worsened mental status with agitation.
•
This distressing symptom often occurs in those with rapidly escalating opioid requirements and
can be challenging for all.
•
Prevention can be undertaken in all patients at risk by providing continuity of care; keeping familiar
persons at the bedside; limiting medication, room, and staff changes; limiting unnecessary
catheterization; and avoiding restraints.
•
Causes such as polypharmacy, opioid toxicity, urinary retention, constipation, and infection should
be ruled out.
•
For mild to moderate cases, add haloperidol.37
•
More severe terminal delirium can be managed with midazolam infusion or other forms of sedation.
•
These interventions, which in conjunction with high-dose opioids can induce "double effect" (the
outcome of hastening death when the intention is purely to relieve symptoms), require expertise
and can lead to ethical controversy.38,39
•
Consultation with a palliative care specialist is recommended when delirium, pain, or any other
symptoms appear to be intractable.
•
As mental status changes occur during the dying process, patients lose the capacity to clear upper
respiratory secretions ("death rattle").
•
Nonpharmacologic interventions, such as positioning to facilitate drainage and very gentle anterior
suctioning (not deep), are an appropriate initial response.
•
Pharmacologic interventions may include hyoscyamine (Levsin), glycopyrrolate (Robinul),
scopolamine, octreotide, and the oral use of atropine eyedrops (Table 5).40
•
Patients do not report experiencing these sounds to be as distressing as family members or
caregivers find them, and education regarding this issue may be as effective as positioning and
medication.41
•
A randomized trial is presently underway comparing the effectiveness of different strategies.
Treatment of Excessive
Respiratory Secretions
• Treatment
• Dosage
• Atropine eye drops 1%
• One to two drops orally or under the tongue;
titrate every eight hours
• Glycopyrrolate (Robunil)
• 1 mg orally or 0.2 mg subcutaneously or
intravenously every four to eight hours as needed
• Hyoscyamine (Levsin)
• 0.125 to 0.5 mg orally, under the tongue,
subcutaneously, or intravenously every four
hours as needed
• Scopolamine
• One to two patches applied topically and changed
every 48 to 72 hours