What types of pain can occur and which treatments are most suitable
advertisement

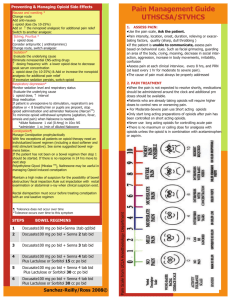
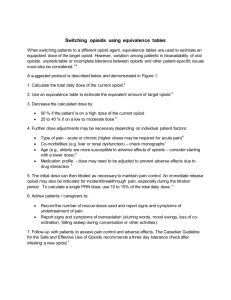
What types of pain can occur and which treatments are most suitable? Drugs Nociceptive pain Neuropathic pain pain may be mixed nociceptive/neuropathic paracetamol effective; most useful when taken regularly at maximal recommended doses (negligible anti-inflammatory effect) less effective opioids effective may be effective (depends on choice and dose) NSAIDs effective (useful anti-inflammatory effects) less effective TCAs, parenteral local anaesthetics, antiepileptics, clonidine rarely used may be effective (TCAs and antiepileptics are the treatments of choice) What long term issues may occur with chronic opioid use? Most specialists in pain medicine agree that patients on opioids will always develop physical dependence, will sometimes develop tolerance, but will rarely develop addictive disorders. The actual risk is unknown, and will vary depending on many factors including genetic factors, personality and psychiatric disorders, and the pharmacological and physicochemical properties of the drug prescribed. Patients need clarification and reassurance about what these terms mean and what to expect when taking opioids long term. Physical dependence is an ‘adaptation’ process, where the body becomes reliant on the externally provided opioid. The patient will develop a ‘drug class–specific withdrawal syndrome’ if they cease the opioid medication suddenly, or reduce the dose rapidly, or are administered an antagonist. The time to onset will depend on the half-life of the opioid ceased. For methadone, withdrawal symptoms can present from three days after cessation, and last as long as 21 days. Features of withdrawal syndrome are shown in Box 1.3. Ceasing the opioids slowly over several weeks to months (depending on the drug and the dose) can prevent withdrawal symptoms. Safe reduction rates are about 10% of the dose, weekly. Patients and their doctors often consider withdrawal symptoms as an indication of addiction, but withdrawal is purely a physiological response to lack of drug (see Drug addiction below). Tolerance is an adaptation process, in which exposure to the drug induces changes that diminish the drug’s effects. Over time the patient will require increasing doses of the drug, or the same dose more frequently, to have the same effect. These increases need to be carefully considered and discussed. High doses of opioids can cause their own problems, so most chronic pain specialists have maximum doses with which they feel comfortable based on clinical experience—morphine 180 mg/day, oxycodone 120 mg/day, and methadone 60 mg/day are considered reasonable maximum daily doses. Tolerance is felt to be less likely with long-acting opioid preparations. An adaptation occurs to all opioid therapeutic and adverse effects, but at different rates—and adaptation to constipation occurs last (see Table 1.5). Drug addiction is a chronic neuropsychobiological disorder, with genetic, psychosocial and environmental factors influencing its development and manifestation. It is characterised by aberrant drug-seeking and drug-taking behaviours that can include cravings, compulsive use, impaired control over drug use, and continued use despite harm. What was the total daily dose of Michael’s documented opioid consumption? Drug Endone 15mg Codeine 12.8 Codeine 30 Frequency 5 4 2 Opioid dose 75 mg 51.2 mg 60 mg 186 mg Equianalgesic When changing opioid, start at 50% of the approximate equianalgesic dose; then titrate according to response (see alsoEquianalgesic dosing). Approximate dose equivalent to 10 mg IM/SC morphine1 Approximate duration of action (hours)2 Comments codeine3 (analgesic only) 120–130 mg SC/IM; 200 mg oral 3–4 mild-to-moderate pain dextropropoxyphene3 unknown 4–6 mild-to-moderate pain; not recommended fentanyl 100–150 mcg SC 0.5–1 moderate-to-severe acute or chronic pain; preferred in renal impairment hydromorphone3 1.5–2 mg SC/IM; 6–7.5 mg oral 2–4; 24 (controlled release) moderate-to-severe acute or chronic pain methadone (analgesic only) 10 mg SC/IM; 20 mg oral4 8–24 (chronic dosing) severe chronic pain morphine3 30 mg oral 2–3; 12–24 (controlled release) moderate-to-severe acute or chronic pain Drug Agonists Drug Approximate dose equivalent to 10 mg IM/SC morphine1 Approximate duration of action (hours)2 Comments oxycodone 15–20 mg oral 3–4; 12–24 (controlled release) moderate-to-severe acute or chronic pain pethidine3 75–100 mg IM 2–3 not recommended tramadol3 100–120 mg IM/IV; 150 mg oral 3–6; 12–24 (controlled release) moderate-to-severe pain 0.4 mg IM; 0.8 mg sublingual 6–8 not first line for analgesia Partial agonists buprenorphine(analgesic only) Compare and contrast the opioid pain patches marketed in Australia Norspan (buprenorphine) Partial agonist High affinity for opiod receptors Prolonged onset and duration of action Takes 3 days to reach ss Not first line for analgesia 20 ug/hr is patch is approximately equivalrent to 100-150 mg/day of oral tramadol OR 36 mg/day of oral morphine 20 ug/hr patch is LESS potent than the LOWEST strength fentanyl patch (12 ug/hr) Adapted from AMH 2011 Durogesic (Fentanyl) Patch is efctive for 72 hoursf Takes 24-72 hrs to reach maximum effect, ss may not be reached until the second patch is applied. Moderate to severe acute pain or chronic pain 12 ug/hr patch is approxiametely equivalent to 45 mg/day oral morphine