Dr. Carl Davis presentation
advertisement
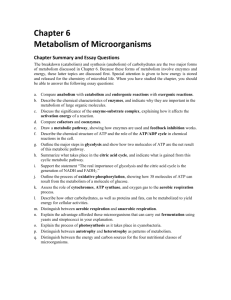
Predicting Human Drug Metabolism and Pharmacokinetics in Drug Discovery Carl D. Davis, Ph.D. April 17th 2007 Drug Metabolism and Pharmacokinetics Pharmaceutical Candidate Optimization Bristol-Myers Squibb Company carl.davis@bms.com Agenda • Introduction: the significance of drug metabolism in drug discovery • Overview of drug-metabolizing enzymes and associated concerns • Tools for predicting human drug metabolism and pharmacokinetics • Scaling preclinical data to predict human pharmacokinetics • Summary 2 Drug Metabolism • The metabolism and toxicity of phenacetin and acetaminophen are well studied and very illustrative examples of processes that can affect drugs in general 3 Drug Metabolism • The exposure of xenobiotics (e.g. drugs) and endogeneous substrates is regulated in animals and humans by clearance, either by direct elimination (biliary and/or renal) or by enzyme-mediated metabolism – Generally this is a detoxication process that prevents accumulation of bioactive compounds in the body • can also produce reactive metabolites and toxicity • The contribution of these processes to total clearance of a drug is evaluated in drug discovery and development to identify the safe efficacious dose of a compound and safe exposure of its metabolite(s) – In discovery, drug metabolism is typically an impediment when looking for an optimal dose • More highly cleared compounds require bigger and more frequent doses to achieve a therapeutic effect – Problems: formulation, inter-individual variability, drug-drug interactions and safety margins 4 The Significance of Drug Metabolism • The oral exposure profile of a drug depends on its Absorption, Distribution, Metabolism, and Excretion (ADME) – The rate of metabolism is a significant factor governing the oral bioavailability of a drug 5 Metabolic Clearance and Systemic Exposure • Target exposure lie in the therapeutic window with safety vs risk defined by the unmet medical need, the severity of disease and the quality of options available 6 Drug Metabolism in a Drug Discovery Setting • Large number of structurally diverse compounds – Methods optimized for throughput and economy • More sophisticated methods used for lead compounds – Most sophisticated methods used in Development (GLP) • Limited data available on compound properties – Matrix teams encounter matrix problems: • Solubility, Absorption, Active-Efflux, Metabolism, Toxicity, Efficacy – Define issues for development • New PK/PD models – Limited/no validation data available • Species differences in pharmacology • Species differences in drug metabolism and PK – Consider active metabolite(s) • Limited/No human ADMET data available – Discovery studies predictive rather than mechanistic • Revise as human data become available 7 Overview of Drug-Metabolizing Enzymes and Associated Concerns 8 Cytochromes P450 • Cytochromes P450 (CYPs) are a hemethiolate superfamily of enzymes that are widely distributed across species (bacteria → human) • In mammals CYPs expressed in many tissues; most highly expressed in the liver • Regulate the metabolism of structurally diverse xenobiotics and some endobiotics (e.g. steroids) – Most important class of drug-metabolizing enzymes • CYP nomenclature is based on shared homology of amino acid sequence: Family (>40%) Subfamily (>55%) CYP2C19 Isoform Family (>40%) Subfamily (>55%) CYP2C9*2 Isoform Allele Genotype/ Phenotype 9 Relative Amounts of Individual Human Hepatic CYPs Shimada et al., JPET: 1994 Lasker et al., Arch. Bioch. Biophys:1998 10 Human Cytochromes P450 and their Relative Contribution to Hepatic Drug Metabolism Bertz & Granneman, ClinPK: 1997 ≈ 60% of drugs are metabolized primarily by CYPs: • CYP3A4 is involved in the metabolism of most of them • large active site volume can accommodate multiple substrates • CYP2D6 is involved in the metabolism of many CNS drugs 11 Polymorphic Distribution Simple bimodal distribution Frequency Fast CL Phenotype Antimode Slow CL Phenotype 1 2 3 4 5 6 7 8 9 10 11 Phenotype (e.g. Cmax µg/mL) • A trait with differential expression in >1% of the population 12 12 Frequency of CYP Polymorphic Phenotypes (divers sources) • CYP2D6 has a complex genotype and trimodal phenotype • Slow, Fast and UltraFast Metabolizers 13 13 CYP2D6 Genotype and Nortriptyline PK Dalen P, et al. Clin Pharmacol Ther (1998) • The clearance of an equivalent dose of nortriptyline in humans is markedly dependent on the relative expression and functional activity of CYP2D6 14 CYP Polymorphisms and Adverse Drug Reactions Enzyme Variant Allel (Frequency in Caucasian) Examples of ADRs associated with Variant Allele CYP1A2 CYP1A2*1F (68%) Antipsychotics: tardive dyskinesia CYP2C9 CYP2C9*2 (8-13%); CYP2C9*3 (7-9%) Warfarin: haemorrhage Phenytoin: phenytoin toxicity Tolbutamide: hypoglycaemia CYP2C19 CYP2C19*2 (13%); CYP2C19*3 (0%) Mephenytoin: toxicity Diazepam: prolonged sedation CYP2D6 CYP2D6*4 (12-21%); CYP2D6*5 (4-6%); CYP2D6*10 (1-2%); CYP2D6*17 (0%) Propafenone: arrhythmias Metoprolol: bradycardia Nortriptyline: confusion Opioids: dependence Phenformin: lactic acidosis Perhexiline: hepatotoxicity CYP3A4 CYP3A4*1B (5.5%) Epidophyllotoxins: treatmentrelated leukaemias Pirmohamed and Park Toxicology (2003): Adapted from Ingelman-Sundberg et al. (1999), Ingelman-Sundberg (2001) and Primohamed and Park (2001) 15 Non-CYP Drug Metabolizing Enzymes • Cytochromes P450 are not the only drug-metabolizing enzymes: – Flavin Monooxygenases (FMOs; membrane-bound & NADPH-dependent) – Esterases: AChe BChe, CE1, CE2 et al (drugs and prodrugs) – Amidases (peptides including “biologicals”) – Uridine Glucuronosyl-S-Transferases (UGTs) – Glutathione-S-Transferases (GSTs) – Aldehyde Oxidase (AO) – Xanthine Oxidase (XO) – Monoamine Oxidase (MAO) – Alcohol & Aldehyde Dehydrogenase (non-specific) – N-Acetyl Transferases (NATs) – Sulfotransferases (STs) – Many others: e.g. Epoxide hydrolases; DT Diaphorase; O-Methylation; SMethylation; Amino Acid Conjugation: glycine, taurine; histamine methyltransferase (HMT); thiopurine methyltransferase (TPMT); catechol O-methyltransferase (COMT)... 16 NAT2: Isoniazid Exposure and Bimodal Phenotype H N O Frequency of Slow Acetylator Phenotype (Evans 1989): Canadian Eskimos: Asian: European/Caucasian: Egyptian: Moroccan: 5% 10-20% 40-70% 80% 90% NH2 N Isoniazid (Isonicotinyl Hydrazine) TOXICITY: Isoniazid-related peripheral neuropathy greater in slow acetylators (still used to treat non-resistant TB) 17 Drug Metabolizing Enzymes and Bioactivation • Typically NATs mediate a detoxification pathway with side effects more prevalent in Slow Acetylators • N-Acetylation also involved in toxicity, with NATs mediating bioactivation e.g. of procarcinogens Metabolism and Bioactivation of Arylamines (spontaneous) Target nucleophiles e.g DNA and proteins…. Potential for toxicity (structural alert) • Knowing the enzyme(s) that metabolize your drug helps you to understand mechanisms involving species and/or organ-specific toxicity and their relevance to human safety 18 Genetic Polymorphisms of Non-CYP Drug Metabolizing Enzymes that Increase the Risk of Adverse Drug Reactions Enzyme/Target/Gene Drug Adverse Drug Reaction Butyrylcholinesterase Succinylcholine Prolonged apnoea N-acetyltransferase 2 (NAT2) Sulphonamides Hydralazine Isoniazid Hypersensitivity Lupus erythematosus Neuoropathy Dihydropyrimidine dehydrogenase Fluorouracil Azathioprine Mercaptopurine Myelotoxicity Myelotoxicity Myelotoxicity UGT1A1 Irinotecan Diarrhoea, myelotoxicity (Güzey & Spigset: Drug Safety, 2002) 19 Human Arylamine N-Acetyl Transferases Figure from Patin (AJHG, 2006) • When a drug is metabolized primarily by one pathway ethnic differences in its metabolism should be considered in the dose prescribed Tools for predicting human drug metabolism and pharmacokinetics 21 Tools for Studying Drug Metabolism In Vitro: • Fresh or cryopreserved hepatocytes: gold standard – Human cells available for biomedical research • Liver subfractions: cheap and simple to prepare – S9, Microsomes, Cytosol, Mitochondria • Liver slices: cheap, not as simple to prepare; multiplexed assays – Fresh human liver tissue has very limited availability • Recombinant enzymes: very specific – Transfected cells; Microsomes/Supersomes • Inhibition studies – Typically with human liver microsomes with drug ± CYP-selective inhibitor. (e.g. ketoconazole for CYP3A; quinidine for CYP2D6) 22 Tools for Studying Drug Metabolism In Vivo: • Transgenic animals – Knockout mice/rats – Humanized mice/rats • In vivo inhibition studies: complex model – 1-Aminobenzotriazole (non-selective mechanistic CYP inhibitor) – Cimetidine (rat CYP2C11 inhibitor) 23 Scaling preclinical data to predict human pharmacokinetics 24 Predicting Human Clearance and PK Generate In Vitro Data: • Incubate drug with liver microsomes or hepatocytes, measure intrinsic clearance and apply scaling factors to predict in vivo clearance – co-incubate with a series of CYP-selective inhibitors to get a relative contribution • Incubate drug with recombinant enzymes, measure turnover, correct for relative abundance and kcat – apply scaling factors to predict in vivo clearance Generate In Vivo Data: • Use allometric-scaling of CL and Vss in animal PK studies to predict equivalent parameters in human Predict PK: • Use the in vitro/in vivo CL and Vss values and relevant absorption data to predict a human PK exposure profile and simulate scenarios for bioavailability, CL and DDI 25 Reaction-Phenotyping Methods: Calculating Intrinsic Clearance • Intrinsic clearance (CLint) is the enzyme-mediated clearance that would occur without physiological limitations (e.g. hepatic blood flow) Metabolite-Formation Approach: Rate of Metabolism, ν = Vmax * CE Km + CE CLint = Vmax/Km Rate (nmol/min/mg protein) Michaelis-Menten Kinetics (Simple form) Vmax 15 Rate-linear metabolite formation kinetics 0 0 10 Km Substrate Concentration (uM) CLint = (ml/min/mg) t1/2 = ln2/k ln2 t1/2 * [HLM] Time 1 0 -1 0 ln[S] (uM) When CE << Km C = C0 * e-kt Substrate Concentration (uM) Substrate-Depletion Approach: 60 -2 -3 -4 -5 y = -0.0693x (slope = -k) -6 First-Order kinetics 0 0 60 Time 26 Reaction-Phenotyping Methods: Scaling Intrinsic Clearance in Liver Microsomes or Hepatocytes to In Vivo Hepatic Clearance Using CLint from MM or substrate-depletion kinetics: CLintin vitro Scaling factors (e.g. microsomal; hepatocellularity) CLint’in vivo Models of hepatic clearance (apply blood-flow limits) CLh as %QH In Vivo Clearance (Exemplified by Houston, 1994) • By modifying CLint, the effect of polymorphisms and/or DDIs on total exposure can be predicted 27 In Vivo Hepatic Clearance and the Venous Equilibrium or “Well-Stirred” Model The Well-Stirred model is the one most commonly used for scaling hepatic clearance (CLH): CLH = QH * fub*CLint’in vivo QH + fub*CLint’in vivo (NB: with in vivo data, this variation assumes concentration in blood and plasma to be the same: CB/CP = 1) High Clearance drugs: (i.e. blood-flow limited) CLH ≈ QH Low Clearance drugs: CLH ≈ fub*CLint’in vivo There are many other factors to consider in predicting human PK 28 Scaling rCYPs to HLM Total metabolic clearance is the sum of individual reactions: n Vtotal = i=1 Vmaxi * S Kmi + S The Total Normalized Rate (TNR) approach uses the rate of metabolism measured in each rCYP, and factors based on the relative abundance of the CYP in HLM to get an HLM equivalent: n V(s)HLM = Ai * Vi(s)rCYPi i=1 Theoretically: V(s)HLM = % Contribution CYPiHLM = CLintHLM (if kcatrCYPi = kcatHLMCYPi) Ai * Vi(s)rCYPi* 100 V(s)HLM Ai denotes the relative abundance of the enzyme (e.g. pmol CYP/mg liver microsomal protein) 29 Predicted Human Reaction-Phenotype • Measure metabolism in human recombinant CYPs: Drug A shows the same rate of metabolism in each; Drug B shows greater metabolism in CYP2D6 (polymorphic). • The predicted phenotype depends on the relative expression of the native human CYPs 30 Allometric-Scaling Y = aWb (Y= CL or Vss) • In vitro and in vivo data can be fitted to predict the human clearance • Using the exponents and Species Invariant-Time methods, the human PK exposure profile can be predicted and used for simulations 31 The Significance of Drug Metabolism • Calculate the relative contribution of a CYP-mediated pathway to the overall clearance and thus predict the effect of a co-administered CYP inhibitor on oral exposure: AUCpo (Inhibitor) AUCpo (Substrate) 1 = fm*fmP450 CLint(Substrate)/CLint(Inhibitor) + [1-(fm*fmP450)] • Single CYP primary clearance mechanisms are unattractive in that they are susceptible to altered oral exposure following coadministration of a potent CYP inhibitor 32 Reaction-Phenotyping • Predict the in vivo metabolic clearance and the contribution of individual Drug Metabolizing Enzymes to the total in vivo clearance – A drug with a metabolic clearance (e.g. >40% of the total clearance) and metabolized by a polymorphic enzyme and/or a primary enzyme (e.g. >30-50% of the total metabolic clearance) has an increased relative risk of drug-drug interactions and/or individual variation – Reaction-phenotyping can refine the human dose projection 33 Putting Some of it Together IMPACT OF RESULTS If unsafe, the drug won’t be developed If target efficacious levels can’t be reached, the drug won’t be developed • The predicted human PK and drug metabolism can point towards potential drug-drug interactions and/or polymorphisms that may affect the new drug (a multitude of factors can confound the predictions) • First in Human (FIH) starting doses and controlled human CYP inhibition studies provide adjustments for better prospective modeling of lead/backup drugs 34 Summary • Enzyme-mediated clearance affects most drugs, with the CYP superfamily of enzymes usually involved and CYP3A4 the worst offender • Metabolic clearance is a significant factor in oral bioavailability and thus the dose prescribed • Many CYPs are polymorphically expressed: profound differences can be seen between humans in their exposure to the drug and/or metabolite(s) • Major clearance pathways (>40% of total) mediated by a single enzyme can be a concern if that enzyme is polymorphically expressed or inhibited or induced (co-medicant/herbal supplement/diet/environment) – Drug metabolizing enzymes generate active/reactive metabolites that may be involved in efficacy and/or toxicity associated with the drug • An array of tools are available (in vitro and in vivo) that allow early screening and prediction of human PK and drug metabolism – These tools have reduced attrition, with better PK properties associated with new drugs: improved safety, faster development and lower R&D costs 35 Thanks for your attention