Chapter 20
advertisement

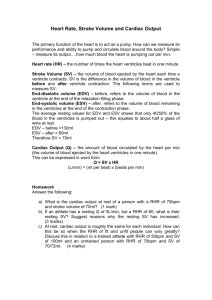
Chapter 20 the heart Anatomy review Electrical activity of the whole heart (EKG) Electrical activity of the heart cells The Cardiac Cycle Cardiac Input and Output (dynamics) Heart review 4 chambers 2 atria 2 ventricles receive send 4 valves 2 AV valves 2 semilunar valves 2 circuits systemic pulmonary external heart anatomy fig. 20-9 internal heart anatomy fig. 20-6 100 keys (pg. 678) “The heart has four chambers, two associated with the pulmonary circuit (right atrium and right ventricle) and two with the systemic circuit (left atria and left ventricle). The left ventricle has a greater workload and is much more massive than the right ventricle, but the two chambers pump equal amounts of blood. AV valves prevent backflow from the ventricles into the atria, and semilunar valves prevent backflow from the aortic and pulmonary trunks into the ventricles.” cardiac conduction system modified cardiac muscle cells •SA node (sinoatrial node) wall of RA •AV node (atrioventricular node) between atrium and ventricle •conducting cells AV bundle (of His) conducting fibers Purkinje fibers conducting system of heart fig. 20-12a prepotential cannot maintain steady resting potential gradually drift toward threshold SA node 80-100 bpm AV node 40-60 bpm fig. 20-12b because SA node is faster… …it controls the heart rate (pacemaker) but heart rate is normally slower than 80-100 bpm (parasympathetics) if SA node is damaged, heart can still continue to beat, but at a slower rate if heartbeat is slower than normal… … bradycardia if heartbeat is faster than normal… … tachycardia impulse conduction fig. 20-13 impulse conduction SA node atria get signal - contract signal to AV Node AV node sends signal to ventricles (time delay) ventricles contract after atria are done damage to any part of conducting system may result in abnormalities (EKG) ECG’s EKG’s electrocardiagram recording of the electrical activity of the heart (from the surface of the body) fig 20-14 ECG’s different components: P wave depolarization of the atria QRS complex depolarization of the ventricles bigger stronger signal T wave repolarization of the ventricles ECG’s fig 20-14 EKG ECG’s to analyze: size of voltage changes duration of changes timing of changes intervals ECG’s fig 20-14 EKG ECG’s intervals: P-R interval from start of atrial depolarization to start of QRS complex time for signal to get from atrium to ventricles if longer than 200 msec can mean damage to conducting system ECG’s intervals: Q-T interval time for ventricular depolarization and repolarization (ventricular systole) if lengthened, may indicate, [ion] disturbances, medications, conducting problems, ischemia, or myocardial damage. ECG’s intervals: T-P interval from end of ventricular repolarization to start of next atrial depolarization the time the “heart” is in diastole the “isoelectric line” fig 20-14 EKG T-P interval ECG’s intervals: abnormalities cardiac electrical activity = cardiac arrhythmias some are not dangerous others indicate damage to heart 100 keys (pg. 688) “The heart rate is normally established by cells of the SA node, but that rate can be modified by autonomic activity, hormones, and other factors. From the SA node the stimulus is conducted to the AV node, the AV bundle, the bundle branches, and Purkinjie fibers before reaching the ventricular muscle cells. The electrical events associated with the heartbeat can be monitored in an electrocardiagram (ECG).” Electrical activity of the heart cells 99 % of heart is contractile cells similar to skeletal muscle AP leads to Ca2+ around myofibrils Ca2+ bind to troponin on thin filaments initiates contraction (cross-bridges) but there are differences… nature of AP location of Ca2+ storage duration of contraction Electrical activity of the heart cells The action potential resting potential of heart cells ~ -90mV threshold is reached near intercalated discs signal is AP in an adjacent cell (gap junctions) Electrical activity of the heart cells The action potential review skeletal muscle fig. 20-15 Electrical activity of the heart cells The action potential once threshold is reached the action potential proceeds in three steps. Electrical activity of the heart cells The action potential - step 1 rapid depolarization (like skeletal muscle) Na+ into cell through voltage-gated channels (fast channels) Electrical activity of the heart cells The action potential - step 2 the plateau Na+ channels close Ca2+ channels open for a “long” time (slow calcium channels) Ca2+ in balances Na+ pumped out Electrical activity of the heart cells The action potential - step 3 repolarization Ca2+ channels begin closing slow K+ channels begin opening K+ rushes out restoring resting pot. Electrical activity of the heart cells The action potential - step 3 repolarization Na+ channels are still inactive cell will not respond to stimulus = refractory period fig. 20-15a Electrical activity of the heart cells The role of calcium extracellular Ca2+ enters cells during the plateau phase (20%) Ca2+ entering triggers release of Ca2+ from sarcoplasmic reticulum ... heart is highly sensitive to changes in [Ca2+] of the ECF Electrical activity of the heart cells The role of calcium in skeletal muscle, refractory period ended before peak tension developed… …summation was possible …tetanus. in cardiac muscle refractory period lasts until relaxation has begun… …no summation …no tetanus. Clinical note: Heart attacks blockage of coronary vessels myocardium without blood supply… …cells die (infarction) myocardial infarction (MI) = heart attack Clinical note: Heart attacks blockage of coronary vessels due to: CAD (coronary artery disease) (plaque in vessel wall) blocked by clot (thrombosis) Clinical note: Heart attacks blockage of coronary vessels as O2 levels fall, cardiac cells will: accumulate anaerobic enzymes die and release enzymes LDH SGOT CPK CK-MB lactose dehydrogenase serum glutamic oxaloacetic transaminase creatine phosphokinase cardiac muscle creatine phosphokinase to here 3/26 lec # 31 Clinical note: Heart attacks anticoagulants (aspirin) clot-dissolving enzymes quick treatment will help reduce damage due to blockage Clinical note: Heart attacks risk factors: smoking high blood pressure high blood cholesterol high [LDL] diabetes male severe emotional stress obesity genetic predisposition sedentary lifestyle any 2 more than doubles your risk of MI The cardiac cycle contraction (systole) relax (diastole) fluid (blood) moves always moves from higher pressure… …toward lower pressure fig. 20-16 The cardiac cycle atrial systole atrial diastole together ventricular systole ventricular diastole generic heart rate 75 bpm fig. 20-17 The cardiac cycle atrial systole (100 msec) 1+2 blood in atria is pushed through AV valves into ventricles (follows path of least resistance) “tops off” the ventricles blood in ventricles is called EDV (end diastolic volume) 3… end of atrial systole ventricular diastole begins The cardiac cycle ventricular systole (270 msec) …3 pressure start to rise in ventricle when it is greater than pressure in atria, the AV valves will close (chordae tendineae and papillary m.) “lubb” 4 pressure continues to build until it can force open the semilunar valves The cardiac cycle ventricular systole (270 msec) 4 up until now, ventricles have been contracting but no blood has flowed: isovolumetric contraction ventricular volume has not changed but the pressure has increased The cardiac cycle ventricular systole (270 msec) when pressure in ventricle is greater than pressure in the arteries, the semilunar valves will open 5 ventricular ejection stroke volume some blood left behind end systolic volume (ESV) The cardiac cycle ventricular systole (270 msec) 6 as pressure drops below that of arteries, the semilunar valves will close again “Dupp” The cardiac cycle ventricular diasatole (430 msec) 7 semilunar valves are shut AV valves are shut too (temporarily) isovolumetric relaxation 8 when pressure gets below atrial pressure, AV valves will open and ventricle will begin to fill passively fig. 20-17 Heart sounds auscultation stethoscope lubb lubb DUPP DUPP Heart sounds lubb closing of the AV valves as ventricular contraction begins Heart sounds DUPP closing of the semilunar valves as ventricular relaxation begins Heart dynamics cardiac output heart rate stroke volume variation & adjustments Heart dynamics EDV definitions end diastolic volume ventricle is full beginning to contract ESV end systolic volume ventricle is done contracting (a little blood left inside) Stroke volume SV = EDV - ESV Heart dynamics definitions cardiac output (CO) CO = HR (heart rate) x SV how much blood the heart pumps in a minute both the SV and the HR can vary Heart dynamics both the SV and the HR can vary fig. 20-20 Heart dynamics variation in HR autonomics dual innervation to SA node Heart dynamics HR parasympathetics releases ACh opens K+ channels lowers the resting potential (hyperpolarize cell) slows heart rate controlled by cardioinhibitory centers in the medulla oblongatat Heart dynamics HR parasympathetics controlled by cardioinhibitory centers in the medulla oblongata reflexes hypothalamus Normal: Parasympathetics: fig 20-22 Heart dynamics HR sympathetics releases NE binds to beta-1 receptors opens Na+/Ca2+ channels depolarize cell speeds up heart rate Heart dynamics HR sympathetics controlled by cardioacceleratory centers in the medulla oblongata reflexes hypothalamus Normal: Sympathetics: fig 20-22 Heart dynamics HR atrial (Bainbridge) reflex increased venous return stretches atria stimulates stretch receptors stimulates sympathetics increase HR (and CO) Heart dynamics HR hormones E, NE, thyoid hormone affect SA node speed up HR to here 3/30/07 lec# 33 Heart dynamics stroke volume (SV) remember SV = EDV - ESV Heart dynamics SV EDV the amount of blood in the ventricle at the end of its diastolic phase, just before contraction begins. Heart dynamics SV EDV affected by the filling time & venous return preload Heart dynamics SV EDV preload the degree of stretching of the ventricle during diastole preload is proportional to EDV preload affects heart muscles ability to generate tension Heart dynamics EDV preload SV Heart dynamics SV EDV preload “more in = more out” Frank-Starling principle fig. 20-23 Heart dynamics ESV preload contractility afterload SV Heart dynamics SV ESV contractility amount of force generated with a contraction increase + inotropic action decrease - inotropic action Heart dynamics SV ESV contractility factors that influence: ANS hormones Heart dynamics SV sympathetic NS NE, E ESV + inotropic effect contractility ANS parasympathetic NS ACh - inotropic effect fig. 20-23 Heart dynamics SV NE, E, glucagon, thyroid hormones ESV contractility hormones (and drugs) dopamine, dobutamine isoproterenol digitalis + inotropic effect (hypertension) Heart dynamics SV propanolol timolol etc., (beta-blockers) ESV contractility hormones (and drugs) verapamil nifedipine (Ca2+ blocker) - inotropic effect fig. 20-23 Heart dynamics SV ESV preload contractility afterload the amount of tension needed to open semilunar valves and eject blood Heart dynamics SV ESV afterload the amount of tension needed to open semilunar valves and eject blood greater afterload longer isovolumetric contraction less ejected, larger ESV Heart dynamics SV ESV afterload restrict blood flow inc. afterload constrict peripheral vessels circulatory blockage fig. 20-23 Summary Heart rate hormones venous return EDV filling time venous return ESV preload contractility afterload SV = EDV-ESV 100 keys (pg. 703) “Cardiac output is the amount of blood pumped by the left ventricle each minute. It is adjusted on a moment-to-moment basis by the ANS, and in response to circulating hormones, changes in blood volume, and alternation in venous return. Most healthy people can increase cardiac output by 300-500 percent.”