ELECTROCARDIOGRAPH INTERPRETATION Advanced
advertisement

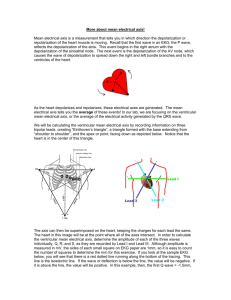
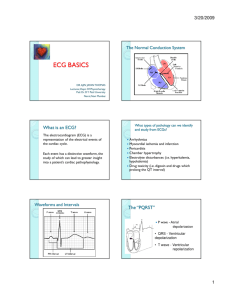
ADVANCED EKG INTERPRETATION Edward Briggs DNP 12 LEAD EKG INTERPRETATION • Objectives • Review basic EKG components • Discuss the process of interpreting an EKG • Discuss Axis interpretation and clinical significance • Discuss EKG changes indicative of: • Ischemia (acute and resolving) • Myocardial scar/old MI • Hypertrophy/Strain • Pericarditis • Other (i.e. electrolytes and EKG changes, medication effects) KEY POINTS • Establish a process and follow it each time you interpret an EKG • Don’t skip steps • Never trust the EKG interpretation and always confirm the interpretation yourself • If unsure of the interpretation consult KEY POINTS • Make sure it is a good tracing • If difficult to read it have it repeated • If old EKG is available always compare to the old EKG • Remember to treat the clinical presentation and not the EKG. Myocardial Infarction may not demonstrate EKG changes initially, especially in small or multi - vessel disease 12 Lead EKG Interpretation • Follow the process 1. Determine rate (normal, tachy, brady) 2. Regularity (regular, irregular) 3. Intervals (PR interval, QRS duration, QTc) 4. Define underlying rhythm (sinus rhythm, atrial fib, 1st degree block, etc.) 12 Lead EKG Interpretation • Follow the process 5. Determine Axis (Normal, RAD, LAD, indeterminate) 6. Evaluate waveform morphology • P wave (Peaked, notched – suggestive of atrial/pulmonary disease process) • QRS height (LVH), BBB, pacer spikes, widening • T wave slurring, peaked (hyperkalemia) 12 Lead EKG Interpretation • Follow the process • 7. Evaluate ST segments • Evaluate all ST’s • Consider ST changes corresponding to region (II, III, AVF = inferior wall, etc) • Note the deflection and shape of any ST changes • Depression, elevation, concave, convex • 8. Evaluate for Q Waves Quick Review • The various intervals seen on the EKG include: • The P wave: represents atrial depolarization Norm 0.12 - 0.2ms Short PR <0.12 ms = Wolf Parkinson White Pr > 0.2 = 1ST or 2nd Degree AVB Quick Review • The various intervals seen on the EKG include: QRS Duration 0.06 – 0.12 ms • The P wave: represents atrial • • • • depolarization The QRS complex: represents ventricular depolarization The ST segment: represents the total ventricular repolarization time The T wave: represents the rapid phase of ventricular repolarization The QT interval: represents the entirety of ventricular systole Norm 0.12 - 0.2ms Short PR <0.12 ms = Wolf Parkinson White Pr > 0.2 = 1ST or 2nd Degree AVB QRS >0.12 ms =BBB or IVCD Quick Review • The various intervals seen on the EKG include: QRS Duration 0.06 – 0.12 ms QRS >0.12 ms =BBB or IVCD • The P wave: represents atrial depolarization • The QRS complex: represents ventricular depolarization • The T wave: represents the rapid phase of ventricular repolarization • The QT interval: represents the entirety of ventricular systole Norm 0.12 - 0.2ms QT Interval Rate dependent Normal Rate <0.44ms Short PR <0.12 ms = Wolf Parkinson White Pr > 0.2 = 1ST or 2nd Degree AVB Quick Review • The baseline of the EKG is defined as the isoelectric or flat line seen between the waveforms that comprise the P wave, QRS complex, and T wave. • When considering segment elevation or depression, each small box represents 1 mm. You will hear ST segment elevation or depression described by the number of millimeters it is above or below the baseline. Isoelectric line Quick Review • The ST segment is the flat area of baseline situated between the QRS complex and T wave that represents the initial phase of ventricular repolarization, referred to as the plateau phase Quick Review - Rate • The classic 12-lead EKG represents about 6 seconds of time. On the EKG paper, one large box is equal to 200 milliseconds or 0.2 seconds. Each large box is composed of five smaller boxes, each equal to 40 milliseconds or 0.04 seconds. This is helpful to remember when 0.04 seconds estimating intervals 0.2 seconds Rate can be measured by counting QRS occurrence in 6 seconds and multiply by ten, or by counting number of large boxes between QRSs, if regular (300,150,100,75,60,50) RATE Quick and easy way to “guess” rate: 1. IF regular rhythm count the number of large boxes between QRS If one large box between QRS then rate = 300 BPM If two large boxes between QRS then rate = 150 If three large boxes between QRS then rate = 75 Etc. If irregular rhythm count the number of QRS complexes documented on the EKG in the rhythm strip and multiply by 10 REGULARITY QUICK AND EASY WAY TO DETERMINE REGULARITY IS TO MEASURE ONE QRS COMPLEX TO THE NEXT. THEN EVALUATE IS THIS IS CONSISTENT THRO THE EKG. Quick Review • The various intervals seen on the EKG include: QRS Duration 0.06 – 0.12 ms • The P wave: represents atrial • • • • depolarization The QRS complex: represents ventricular depolarization The ST segment: represents the total ventricular repolarization time The T wave: represents the rapid phase of ventricular repolarization The QT interval: represents the entirety of ventricular systole Norm 0.12 - 0.2ms QT Interval Rate dependent Normal Rate <0.44ms RHYTHM • Determine the underlying rhythm • Normal Sinus Rhythm • Sinus Arrhythmia • Atrial Fibrillation • Ectopic Beats • Etc. 12 LEAD EKG Review and discussion 12 Lead EKG • Each of these leads records the same electrical activity, but from a different angle. • This is why the EKG tracing will vary from lead to lead. • As depolarization spreads toward a positive pole, there is an upward deflection in that lead. • As it spreads away from a positive pole, there is a downward deflection in that lead. Take the vantage point of each positive pole. As electricity moves toward it, the respective EKG deflection appears positive. As electricity moves away from it, it appears negative EKG CHANGES • An analogy • Think of the electrical flow across the myocardium as a river • If you look at the river from different banks it looks different, but the river hasn’t changed • Now imagine a beaver builds a dam along that river, we see actual change in the flow of the river • The “dam” would be ischemia/scar that would be changing the course of the myocardial electrical flow 12 lead EKG • Made up of • Bipolar leads : I, II, III • Lead I records the electrical difference between the left arm and the right arm electrodes and is positive on the left and negative on the right • Lead II records the electrical difference between the left leg and the right arm electrodes and is positive at the leg and negative at the arm • Lead III records the electrical difference between the left leg and the left arm electrodes and is positive at the leg and negative at the arm 12 lead EKG • Unipolar Augmented Leads – aVR, aVF, and aVL • aVR: Augmented voltage right arm: a combination of leads I and II • aVL: Augmented voltage left arm: a combination of leads I and III • aVF: Augmented voltage foot: a combination of leads II and III 12 Lead EKG • Precordial Leads: V1 V2 V3 V4 V5 V6 12 Lead EKG • Combinations of leads represent flow of electricity as moves over different aspects of the heart • These 12 leads should be always considered in groups because • • • • each set of leads represents a specific area of the myocardium Leads I, aVL, V5, and V6 are the lateral leads. Leads II, III, and aVF are the inferior leads. Leads V1 to V4 are the anterior chest leads. Leads V1, V2 are the anterior septal leads 12 Lead EKG • Each myocardium region is perfused by specific coronary arteries, therefore each cardiac region has corresponding coronary arteries • Anterior • AnterioSeptal • Inferior • Lateral Determine Axis • Axis = electrically where the heart lies in the chest Axis • Axis refers to the general direction of electrical conduction through the heart. • It gives a graphical representation of the electrical position of the heart • Deviation from “normal” represents either malposition of the heart itself or; • Something is altering how the electricity flows over the heart (ischemia, scar, blocks, etc.) AXIS • Axis deviations are divided into 2 categories: • Right Axis Deviation (RAD) • Left Axis Deviation (LAD) • Deviations can occur from physiologic conditions such as obesity, physical morphology (tall thin stretching out myocardium, cavitus pectorum physically rotating the heart) • Deviations can occur from pathologic conditions such as ischemia, infarct altering the electrical flow Determining Axis • Normal axis : 0 to -90 degrees • RAD : + 90 to +/- 180 degrees • LAD : 0 to -90 degrees • Indeterminate : -90 to +/- 180 Determining Axis • Easy Trick: • Hold up your left thumb and right thumb • Left thumb corresponds to lead I • Right thumb corresponds to lead AVF • If lead I is upright and aVF is upright axis is normal • If lead I is upright and aVF is downward axis is left (LAD) • If lead I is downward and aVF is upright axis is right (RAD) • If Lead I and AVF are downward Northwest Region (No Man’s Land) AXIS DEVIATIONS • • • • LEFT AXIS DEVIATION (LAD) Lateral wall myocardial infarction Left ventricular hypertrophy Left bundle branch block Left anterior fascicular block AXIS DEVIATIONS • • • • • • RIGHT AXIS DEVIATION (RAD) Left posterior fascicular block Right bundle branch block Right ventricular hypertrophy Obesity Tall, thin frame, cavitus pectorum Inferior wall myocardial infarction COPD AXIS DEVIATIONS NO MAN’S LAND (NORTHWEST REGION) •emphysema/copd •hyperkalaemia •lead transposition •artificial cardiac pacing •ventricular tachycardia Wave Form Morphology P-Wave • • • • Represents Depolarization across the Atria Normal – 1 P wave precedes each QRS Rounded hump Normal PR interval is < 0.20 ms Wave Form Morphology P-Wave Wave Form Morphology P-Wave The principal cause is pulmonary hypertension due to: •Chronic lung disease (cor pulmonale) •Tricuspid stenosis •Congenital heart disease (pulmonary stenosis, Tetralogy of Fallot) •Primary pulmonary hypertension Wave Form Morphology P-Wave P mitrale The presence of broad, notched (bifid) P waves in lead II is a sign of left atrial enlargement, classically due to: mitral stenosis. Wave Form Morphology QRS Complex • Represents depolarization of the left and right ventricle • Look to the QRS complexes in the precordial leads (V1- V6) • Evaluate R wave progress • Evaluate height and width of the QRS complexes Hypertrophy • Hypertrophy is thickening of the heart muscle secondary to some strain • Think of increased workload (Body builders muscles become hypertrophic in response to increase workload) • CLUE: • Right side think pulmonary • Left side think systemic Poor R Wave Progression • Definition • R wave height ≤ 3 mm in V3. • Causes • Prior anteroseptal MI • Left ventricular hypertrophy • Inaccurate lead placement (e.g. transposition of V1 and V3) • Dilated cardiomyopathy • May be a normal variant Wave Form Morphology QRS Complex – Left Ventricular Hypertrophy -QRS complex is slightly widened (about 0.11 sec), -Left Axis Deviation -Tall R waves are present in multiple leads, and -ST-T changes (formerly called a "strain" pattern) are present. -Frequent concurrent P wave abnormalities Left ventricular hypertrophy (LVH) refers to an increase in the size of myocardial fibers in the main cardiac pumping chamber. Such hypertrophy is usually the response to a chronic volume or pressure load. ●The two most important pressure overload states are systemic hypertension and aortic stenosis ●The major conditions associated with left ventricular volume overload are aortic or mitral valve regurgitation and dilated cardiomyopathy. Wave Form Morphology QRS Complex – Right Ventricular Hypertrophy Clues to the diagnosis include: ●Right axis deviation (>+90) ●R in V1 >6 mm ●R/S ratio in V1 >1 ●Incomplete right bundle branch block ●ST-T wave abnormalities ("strain") in inferior leads ●Right atrial hypertrophy/overload (“P pulmonale”) ●S>R in leads I, II, III, particularly in children (S1S2S3 pattern) Right ventricular hypertrophy (RVH) is present when there is a pathologic increase in muscle mass of the right ventricle. Commonly seen with pulmonary hypertension, pulmonic stenosis, or severe lung disease and cor pulmonale. ABNORMAL EKG - blocks • RIGHT BUNDLE BRANCH BLOCK • In RBBB, activation of the right ventricle is delayed as depolarization • • • • has to spread across the septum from the left ventricle. The left ventricle is activated normally, meaning that the early part of the QRS complex is unchanged. The delayed right ventricular activation produces a secondary R wave (R’) in the right precordial leads (V1-3) and a wide, slurred S wave in the lateral leads. Delayed activation of the right ventricle also gives rise to secondary repolarization abnormalities, with ST depression and T wave inversion in the right precordial leads. In isolated RBBB the cardiac axis is unchanged, as left ventricular activation proceeds normally via the left bundle branch. ABNORMAL EKG - blocks • RIGHT BUNDLE BRANCH BLOCK • Causes of RBBB • Right ventricular hypertrophy / cor pulmonale • Pulmonary embolus • Ischemic heart disease • Rheumatic heart disease • Myocarditis or cardiomyopathy • Degenerative disease of the conduction system • Congenital heart disease (e.g. atrial septal defect) ABNORMAL EKG - blocks • RIGHT BUNDLE BRANCH BLOCK • Diagnostic Criteria • •Broad QRS > 120 ms • •RSR’ pattern in V1-3 (‘M-shaped’ QRS complex) • •Wide, slurred S wave in the lateral leads (I, aVL, V5-6) QRS >120ms Slurred S Wave ABNORMAL EKG - blocks • LEFT BUNDLE BRANCH BLOCK • Normally the septum is activated from left to right, producing small Q • • • • waves in the lateral leads. In LBBB, septal depolarization is reversed (becomes right to left), as the impulse spreads first to the RV via the right bundle branch and then to the LV via the septum. This sequence of activation extends the QRS duration to > 120 ms and eliminates the normal septal Q waves in the lateral leads. The overall direction of depolarization (from right to left) produces tall R waves in the lateral leads (I, V5-6) and deep S waves in the right precordial leads (V1-3), and usually leads to left axis deviation. As the ventricles are activated sequentially (right, then left) rather than simultaneously, this produces a broad or notched (‘M’-shaped) R wave in the lateral leads. ABNORMAL EKG - blocks • LEFT BUNDLE BRANCH BLOCK • Causes • Aortic stenosis • Ischemic heart disease • Hypertension • Dilated cardiomyopathy • Anterior MI • Primary degenerative disease (fibrosis) of the conducting system (Lenegre disease) • Hyperkalemia • Digoxin toxicity ABNORMAL EKG - Blocks • • • • • • LEFT BUNDLE BRANCH BLOCK Diagnostic Criteria •QRS duration of > 120 ms •Dominant S wave in V1 •Broad monophasic R wave in lateral leads (I, aVL, V5-V6) •Absence of Q waves in lateral leads (I, V5-V6; small Q waves are still allowed in aVL) • •Prolonged R wave peak time > 60ms in left precordial leads (V5-6) QRS >120ms Monophasic R waves Dominant S EXAMPLES QRS >120ms ‘W’ V1 ‘M’ V6 Interpretation : Rate – 126 Regularity – Regular Intervals • PR – 0.16 • QRS – 160 ms • QT – 350ms • AXIS – Left Axis Deviation SINUS TACH WITH LEFT “W” in V1 “M” in V6 BBB EXAMPLES QRS >120ms ‘M’ V1 ‘W’ V6 Interpretation : Rate – 78 Regularity – Regular Intervals • PR – 0.16 • QRS – 160 ms • QT – 340ms • AXIS – normal SINUS TACH WITH RIGHT “M” in V1 “W” in V6 BBB ABNORMAL EKG - blocks • INTRAVENTRICULAR CONDUCTION DELAY • Definition : Conduction of impulse is delayed as it moves through the ventricle • QRS duration > 100 ms in the presence of a supraventricular rhythm. • Most commonly due to bundle branch block or left ventricular hypertrophy. • The most important life-threatening causes of QRS widening are hyperkaliemia and tricyclic antidepressant poisoning. New Onset block? Think electrolytes and overdose! ABNORMAL EKG - blocks • INTRAVENTRICULAR CONDUCTION DELAY • Types • Left anterior fascicular block • Left posterior fascicular block • Left bundle branch block • Right bundle branch block • Bifascicular block • Trifascicular block ABNORMAL EKG - blocks • INTRAVENTRICULAR CONDUCTION DELAY • Types • •Left anterior fascicular block • In left anterior fascicular block (aka left anterior hemiblock), impulses are conducted to the left ventricle via the left posterior fascicle, which inserts into the infero-septal wall of the left ventricle along its endocardial surface. ABNORMAL EKG - blocks • INTRAVENTRICULAR CONDUCTION DELAY • Types • In left posterior fascicular block • (aka left posterior hemiblock), impulses are conducted to the left ventricle via the left anterior fascicle, which inserts into the upper, lateral wall of the left ventricle along its endocardial surface. ABNORMAL EKG - blocks • INTRAVENTRICULAR CONDUCTION DELAY • Types • •Bifascicular block is the combination of RBBB with either LAFB or LPFB. • Trifascicular block (TFB) refers to the presence of conducting disease in all three fascicles: • Right bundle branch (RBB) • Left anterior fascicle (LAF) • Left posterior fascicle (LPF) Electrolyte effects Electrolyte effects HYPERCALCEMIA T wave Broad tall Peaked P wave Flattening/absent QRS Widening ST Segment QT HYPOCALCEMIA narrow Prolonged, depressed shortened Prolonged U wave Ectopy Uncommon J-waves Torsades De Pointes Electrolyte effects HYPERKALEMIA HYPOKALEMIA T wave Peaked Negative P wave Flattening QRS Widening ST Segment Depression/flatten QT Prolonged U wave Present Ectopy Ventricular ectopy Atrial Fib/Flutter Vent fib Medication Effects on ECG The most common drugs ingested that may show QRS and/or QT prolongation and arrhythmias (though these are not always present) are: •Calcium channel blockers (particularly verapamil and diltiazem) •Beta blockers (particularly propranolol and sotalol ) •Digoxin •Tricyclic antidepressants •Antipsychotic drugs (particularly thioridazine) •Anticonvulsants (particularly carbamazepine and phenytoin) •Dextropropoxyphene •Antimalarial drugs (chloroquine, quinine) •Antiarrhythmic drugs •Orphenadrine •Lithium (cation) ST Segment • When examining the ST segment, be careful to look for the presence of ST segment elevation or depression. The ST segment should be isoelectric or flat on the baseline. Clinical Point : Deviation of 2 mm (two small boxes) above or below the baseline is indicative of a pathologic process. ST SEGMENT Critical analysis for acute ischemic events ST Segment • The T wave is usually concordant with the QRS complex. Thus if the QRS complex is positive in a certain lead than the T wave usually is positive too in that lead. • Accordingly the T wave is normally upright or positive in leads I, II, AVL, AVF and V3-V6. The T wave is negative in V1 and AVR. The T wave flips around V2, but there is likely some genetic influence in this as in Blacks the T wave usually flips around V3. • The T wave angle is the result of small differences in the duration of the repolarization between the endocardial and epicardial layers of the left ventricle. ST Segment elevation ELEVATION OF THE ST SEGMENT OF THE ECG CAN RESULT FROM MULTIPLE PATHOLOGIES, INCLUDING: • LVH, LBBB, Pericarditis, Hyperkalemia, Anterior AMI. • Acute pericarditis: ST elevation in all leads except aVR • Pulmonary embolism: ST elevation in V1 and aVR • Hypothermia: ST elevation in V3-V6, II, III and aVF • Hypertrophic cardiomyopathy: V3-V5 (sometimes V6) • High potassium (hyperkalemia): V1-V2 (V3) • During acute neurologic events: all leads, primarily V1-V6 • Acute sympathic stress: all leads, especially V1-V6 • Brugada syndrome.** • Cardiac aneurysm. • Cardiac contusion • Left ventricular hypertrophy • Idioventricular rhythm including paced rhythm • ** Brugada syndrome is a genetic disease that is characterised by abnormal electrocardiogram (ECG) findings and an increased risk of sudden cardiac death. ST Segment depression • ST SEGMENT DEPRESSION CAN • • • • • • • RESULT FROM MULTIPLE PATHOLOGIES, INCLUDING: Myocardial ischemia Reciprocal ST segment depression. If one lead shows ST segment elevation then usually the lead 'on the other side' shows ST segment depression. (This is usually seen in ischemia as well. Left ventricular hypertophy with "strain" or depolarization abnormality Digoxin effect Low potassium / low magnesium Heart rate-induced changes (post tachycardia) During acute neurologic events. ST Segment depression • Morphology of ST Depression • ST depression can be either • • • • upsloping, downsloping, or horizontal. Horizontal or downsloping ST depression ≥ 0.5 mm at the J-point in ≥ 2 contiguous leads indicates myocardial ischaemia Upsloping ST depression in the precordial leads is highly specific for occlusion of the LAD. Reciprocal change has a morphology that resembles “upside down” ST elevation and is seen in leads electrically opposite to the site of infarction. Posterior MI manifests as horizontal ST depression in V1-3 and is associated with upright T waves and tall R waves. T-Wave Inversion • negative (or inverted) T wave> 0.5 mm negative T wave in leads I, II, V3, V4, V5 or V6 • Possible causes of T wave changes: • Ischemia and myocardial infarction • Pericarditis • Myocarditis • Cardiac contusion • Acute neurologic events, such as a subarachnoid bleed. • Mitral valve prolapse • Digoxin effect • Right and left ventricular hypertrophy with strain T-Waves • Two characteristics should be always noted with regard to the T wave: inversion and peaked appearance . • Inversion: May represent old infarction or resolving ischemia • Peaked: Electrical instability (i.e. electrolyte imbalance hyperkalemia) Anatomy correlation EKG leads generally correlate to different anatomical portions of the Myocardium and the blood vessels that perfuse that region. J point elevation • The J point is where the QRS complex ends and the ST segment begins. J point elevation is a common and usually benign finding on EKG in younger patients. • Early repolarization is a common finding in young, healthy individuals. It appears as mild ST segment elevation that can be diffuse, however is more prominent in the precordial leads. Early repolarization changes are simply “J point” elevation. Pathologic Q Waves • Pathologic Q waves occur when the electrical signal passes through stunned or scarred heart muscle; as such, they are usually markers of previous myocardial infarctions, with subsequent fibrosis. • A pathologic Q wave is defined as having a deflection amplitude of 25% or more of the subsequent R wave, or being > 0.04 s (40 ms) in width and > 2 mm in amplitude. However, diagnosis requires the presence of this pattern in more than one corresponding lead. • Myocardial infarctions with pathological Q waves are referred to as ST elevation MIs.[5] FOLLOW THE STEPS 1. 2. 3. 4. 5. Rate Regularity Intervals Rhythm Axis Normal RAD LAD No Man’s Land 6. Waveform Morphology Peaked/biphasic P waves QRS changes BBB/conduction delay Low or High Voltage Pacer T-waves Inversions 7. ST Segment Elevation Depression 8. Q-Waves CASE 1 • Rate: • Rhythm: • ST/T: 47 year old male presents with chest pain, dyspnea and diaphoresis. Sudden onset. No prior medical history. No medications. No cardiac risk factors. HR -122 R – 30 B/P 210/110 Pulse ox 84% PR: QRS: Morphology: Q-Waves: Axis: 47 year old male presents with chest pain, dyspnea and diaphoresis. Sudden onset. No prior medical history. No medications. No cardiac risk factors. HR -122 R – 30 B/P 210/110 Pulse ox 84% • Rate: 142 PR: 0.12 QRS: 0.06 Axis: LAD • Rhythm: sinus tach Morphology: Peaked P waves/notched • ST/T: T-wave inversion III and T-wave inversion v1-3 Q-Waves: none This ECG is classic for PE: 1) sinus tach Hypoxia 2) right ventricular conduction delay (R' in V1) 3) T-wave inversions in BOTH precordial leads and in lead III. 4) S1Q3T3 (a tiny R-wave in III is equivalent to a Q-wave). CASE 2 • Rate: • Rhythm: • ST/T: 64 year old male. PMH: HTN DM Lipids PSH 2 ppd x 20 yrs No cardiac hx Sudden onset dyspnea, diaphoresis, weakness approx 1 hour ago. PR: QRS: Morphology: Q-Waves: Axis: CASE 2 • Rate: 100 PR:0.16 QRS: 0.06 Axis: normal to LAD • Rhythm: Sinus tach Morphology: T wave inversion diffuse • ST/T: ST elevation II, III, AVF. ST Depression AVL. V2-5 Q-Waves: II, III, AVF • Dx: acute inferior/lateral wall MI CASE 3 • Rate: • Rhythm: • ST/T: 45 Year old male presents for preoperative clearance for hip surgery. PMH: HTN, Dyslipidemia, Tobacco. Remote cocaine use. PFH: adopted. PSH: None Works as a truck driver. HR – 72 B/P 124/78 R-19 BMI -35 PR: QRS: Morphology: Q-Waves: Axis: CASE 3 • • • • • 45 Year old male presents for preoperative clearance for hip surgery. PMH: HTN, Dyslipidemia, Tobacco. Remote cocaine use. PFH: adopted. PSH: None Works as a truck driver. HR – 72 B/P 124/78 R-19 BMI -35 Rate: 98 PR:0.12 QRS: 0.06 Axis: normal Rhythm: Sinus Morphology: T-wave inversion I, aVL ST/T: ST elevation III, AVF, V2 Q-Waves: III, V2-V6 Dx: Anterior wall MI (Possible acute), lateral wall (old?) CASE 4 HR: 74 Resp: 24 B/P 190/108 Pulse Ox 91% 61 year old female new to practice. Presents for first exam. Denies any medical history but has not seen MD in a decade. PMH: None PSH: None Meds: None PFH: Colon Ca, stroke, MI • Rate: • Rhythm: • Q-Waves: • Dx: PR: QRS: Axis: Morphology: CASE 4 HR: 74 Resp: 24 B/P 190/108 Pulse Ox 91% 61 year old female new to practice. Presents for first exam. Denies any medical history but has not seen MD in a decade. PMH: None PSH: None Meds: None PFH: Colon Ca, stroke, MI • Rate: 104 PR: 0.10 QRS: 0.06 Axis: normal • Rhythm: Sinus Tach Morphology: Tall QRS anterior leads, Peaked T waves ant. T-wave inversion III, Short PR and peaked P • Q-Waves: None • Dx: Left ventricular hypertrophy with p pulmonale CASE 5 • • • • • Rate: 104 Rhythm: Short Q-Waves: Dx: 68 year old male, presents with dyspnea for 1 day. Had Substernal chest pain aaprox 8 hours ago. PMH: HTN Lipids DM PSH 60 pk yr Meds: Atenolol, silfenadil, lipitor, metformin 138/72 HR 58 R-22 Pulse Ox 94% PR: QRS: Morphology Axis: CASE 6 • • • • • Rate: 104 Rhythm: Short Q-Waves: Dx: 94 yr old female local ALF, found unresponsive. No medical history available, patient unresponsive B/P 84/56 R-28 HR 75 Pulse ox 93% PR: QRS: Morphology Axis: CASE 7 • • • • • Rate: 104 Rhythm: Short Q-Waves: Dx: 48 year old male presents for employment physical PMH: None PSH: None Meds: None Tobacco: None Recreational drug use : None PR: QRS: Morphology Axis: CASE 8 • • • • • Rate: 104 Rhythm: Short Q-Waves: Dx: 64 year old male presents to office because “Doesn’t feel good” PMH: Htn PSH: None Meds: lisinopril, silfenadil BP 178/102 HR 54 R-20 Pulse Ox 99% PR: QRS: Morphology Axis: CASE 9 • • • • • Rate: 104 Rhythm: Short Q-Waves: Dx: 64 yr old male presents for DMV clearance. Denies any complaints PMH: None PSH: None Meds: None Tobacco: remote history Drugs: none 156/95 HR 98 Resp: 24 PR: QRS: Morphology Axis: CASE 10 • • • • • Rate: 104 Rhythm: Short Q-Waves: Dx: 92 yr old female from nursing home, “confused” PMH: HTN, CHF, Lipids, DM PSH: CABG Meds: Metoprolol, lasix, lisinopril, spironolactone 96/48 HR: 60 Resp: 16 Pulse Ox 98% PR: QRS: Morphology Axis: CASE 10 • • • • • Rate: PR: Rhythm: Short Q-Waves: Dx: 74 year old male presents for routine follow up/physical exam PMH: CAD/MI, CABG, HTN, obesity, DM Meds: glipizide, metformin, lisinopril/hctz BP 126/80 HR 100 R 24 Pulse ox: 100% QRS: Axis: Morphology