Blood_Vessels__Study_of_
advertisement

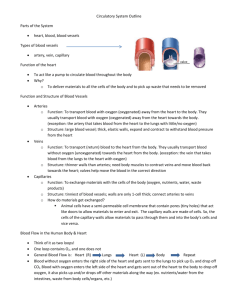
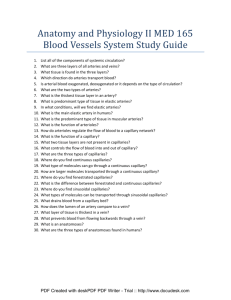
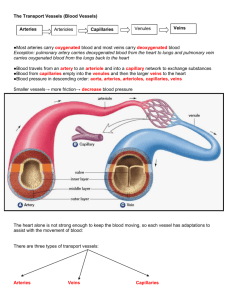
A Study of Blood Vessels Mike Clark, M.D. Types of Blood Vessels 1. Arteries 2. Capillaries 3. Veins Three Generic Circulations in the Body 1. Systemic – blood goes from left ventricle to Right Atrium 2. Pulmonary – blood goes from right ventricle through lungs to left atrium 3. Hepatic Portal – venous circulation – drains blood from portions of gastrointestinal tract (intestines) and takes it to the liver Schematic System Circulation Figure 19.2 Pulmonary Circulation Figure 19.18a Hepatic Portal Circulation Cross Section of Typical Blood Vessel Figure 19.1b Tunica interna (intima) • composed of endothelium cells (simple squamous) - these cells must be smooth in order to not to activate the intrinsic clotting cascade – additionally these cells secrete various paracrine chemicals • Basement membrane or basal lamina • Small amount of loose connective tissue • In some vessels have an internal elastic lamina composed of elastin – particularly in muscular arteries Tunica Media • Composed of various amounts of smooth muscle depending on the blood vessel type • Composed of some loose connective tissue • Larger muscular arteries have an external elastic lamina Tunica Adventitia • Outermost layer of blood vessels – composed of fibroblasts, collagen and elastic fibers. This layer becomes continuous with the connective tissue elements surround the blood vessel – so the vessel in held in place. • Vasa Vasorum – in the walls of the larger thicker blood vessels – the cells of the vessel wall itself needs a blood supply – thus “a vessel to a vessel”. Since veins generally have less oxygen than arteries – the larger veins need more vasa vasorum vessels than the larger arteries • Note: larger thick lymphatic vessels also have vasa vasorum vessels Types of Blood Vessels • Arteries • Arterioles (resistance vessels) • Capillary Bed (inclusive of capillaries) – exchange vessels • Post Capillary Venules – location where most white blood cells leave circulation (diapedesis) • Venules • Small, Medium and Large Veins (capacitance vessels) Figure 19.1 Arteries • Artery – a blood vessel that transports blood away from the heart. The arteries branch considerably as they get further from the heart and the diameter gets smaller. There different types of arteries. Types of Arteries 1. Elastic (Conducting) Arteries – arteries proximal to the heart that can easily stretch and conduct blood from the heart ( aorta, common carotids, subclavian, common iliac arteries and pulmonary trunk 2. Muscular (Distributive) Arteries –arteries with considerable smooth muscle in the walls – thus can vasoconstrict and channel (distribute) blood to organs that need it. The muscular arteries include almost all of the arteries in the body besides those of the elastic – these arteries are large, medium and small. 3. Arteriole – (resistance vessel) very, very tiny artery with a diameter of 0.1mm or less – but considerable smooth muscle in the wall – can perform considerable vasoconstriction (resistance). Table 19.1 (1 of 2) Figure 19.1a Capillaries and Capillary Bed • Capillaries (exchange vessels) are short length (0.25 μm – 1 μm) and thin diameter (10 μm - 30 μm) small vessels. There walls are very thin and sometimes porous (fenestrated, sinusoidal) – thus providing great diffusive ability. The three anatomical types of capillaries will be discussed later in this PowerPoint. • True capillaries are generally located in capillary beds. There are millions of capillary beds in the body. Each population cells needs a capillary bed in order to get oxygen and nutrients. • Capillary beds contain metarterioles and thoroughfare channels. Table 19.1 (2 of 2) Figure 19.4 Venules and Veins • Vein (capacitance vessels) – a blood vessel that returns blood back to the heart. As with arteries – there are different types of veins. Types of Veins 1. Post capillary venule – A tiny (15 μm – 20 μm) blood vessel that has a wall as thin as the capillaries – this is where most white blood cells leave the circulation (diapedesis) 2. Small, medium (less than 1 cm) and large veins Veins generally have a wider inside lumen diameter than an artery – and have less smooth muscle in their walls. It was this reason that veins easily stretch and hold onto to more blood. Most of the blood (around 60%) in the body is located in the veins (high capacitance) at any given time. Table 19.1 (2 of 2) Figure 19.1a Secretions and receptors of Endothelial Cells •Collagens Type II, IV, and V •Lamin – type of intermediate filament •Endothelin – causes vasoconstriction •Nitric Oxide – (Endothelial Derived Relaxing Factor) has many actions like vasodilation and keeps platelets off wall of blood vessels •Von Willebrand Factor – used to assist Clotting Factor VIII to work •Angiotensin Converting Enzyme – converts angiotensin I to angiotensin II •Enzymes that degrade Bradykinin, Serotonin, Prostaglandins, Thrombin and Norepinephrine •Can Bind Lipoprotein Lipase 1. Normally the intact endothelium produces prostacyclin (PGI2)and Nitric Oxide, which inhibit platelet aggregation. It also blocks coagulation by the presence of thrombomodulin and heparin-like molecule on its surface membrane. These two membrane-associated molecules inactivate specific coagulation factors. 2. Injured endothelial cells release Von Willebrand factor and tissue thromboplastin and cease the production and expression of inhibitors of coagulation and platelet aggregation. They also release endothelin, a powerful vasoconstrictor. Factors Preventing Undesirable Clotting • Unnecessary clotting is prevented by endothelial lining the blood vessels • Platelet adhesion is prevented by: – The smooth endothelial lining of blood vessels – Heparin and PGI2 secreted by endothelial cells – Vitamin E quinone, a potent anticoagulant Smooth Muscle For an understanding of smooth muscle excitation- contraction please refer To my PowerPoint Smooth Muscle Excitation Contraction under A&P II Figure 9.25 Figure 9.26 Smooth muscle like cardiac muscle receives some calcium from the outside of the cell for contraction thus it too can be slightly relaxed by administering calcium channel blocker medications. Figure 9.27 Classes of Calcium Channel Blockers 1. Dihydropyridine calcium channel blockers are often used to reduce systemic vascular resistance "-dipine". Amlodipine (Norvasc) Nifedipine (Procardia, Adalat) 2. Phenylalkylamine calcium channel blockers are relatively selective for myocardium, reduce myocardial oxygen demand and reverse coronary vasospasm, and are often used to treat angina. They have minimal vasodilatory effects. Therefore, as vasodilation is minimal with the phenylalkylamines, the major mechanism of action is causing negative inotropy. Phenylalkylamines are thought to access calcium channels from the intracellular side, although the evidence is somewhat mixed. Verapamil (Calan, Isoptin) Gallopamil (Procorum, D600 3. Benzothiazepine calcium channel blockers are an intermediate class between phenylalkylamine and dihydropyridines in their selectivity for vascular calcium channels. By having both cardiac depressant and vasodilator actions, benzothiazepines are able to reduce arterial pressure without producing the same degree of reflex cardiac stimulation caused by dihydropyridines. Diltiazem (Cardizem) Mathematical Analysis of the Circulatory System 1. 2. 3. 4. 5. • • 6. 7. 8. 9. Discussion of Pressure Discussion of Pressure in a pipe without an external compression device (pressure in the blood vessels without the heart) known as “Mean Circulatory Filling Pressure”. Discuss unstressed and stressed blood volume Discuss pressure in blood vessels with heart compression Discuss Flow – velocity of flow versus rate of flow Discuss Resistance – resistance in pipes arranged in series versus those arranged in parallel Total Peripheral Resistance Examine Diffusion Formula Examine Capacitance (Compliance) Formula Examine the Mean Arterial Pressure Formulas Wall Tension Formulas of importance Flow = ∆P/ R, ∆P is the change in pressure from one area to another (P1 – P2) – in the direction of flow, R is the resistance (Note: pressure drops off as a fluid or gas passes further down the pipe – thus the pressure in proximal area 1 (P1) is higher than the pressure is distal area 2. The more pressure drop off the more the flow. Also, the less the resistance the better the flow. • Rate of Flow = amount of gas or liquid/time (example ml/min) • Velocity of flow = amount of gas or liquid/time/cross sectional area (another way of looking at it is Vf = rate of flow/cross sectional area) example of velocity of flow ml. /min per cm2 Note: Area of a circle (like the inside of a vessel ) = equals pi (π) times the radius squared (π⋅r2), example ml. /min per cm2 Flow formula derived Ohm’s Law Formulas of Importance • Resistance –a force of impedance (holding back) R = 8ηL/πR4 , η is viscosity of the gas or liquid, L is the length of the vessel, and R is the resistance raised to the 4th power • Summation (∑) of Resistances – adding up the resistors in flow arrangement a series arrange • Resistors in series – one resistor in front of another ∑ = R1 + R2 + R3 + …… • Resistors in parallel – a pipe leads into a branching set of pipes ∑ = 1/R1 + 1/R2 + 1/R3 +.. • Note: resistors in parallel give less total resistance than those in series (think of the capillary arrangement) Total Peripheral Resistance (Systemic Vascular Resistance) • The TPR (SVR) is the summation (∑ ) of all the resistors in the systemic (Left Ventricle – to Right Atrium) circulation. Some of the blood vessel resistors are in series (R1 + R2 + R3 + ……) and some are in parallel (1/R1 + 1/R2 + 1/R3 )– thus the two different formulas must be used. • Since R is raised to 4th power it numerically is the most significant contributor to Total Peripheral Resistance – thus vasoconstriction and vasodilation are the most important contributors to TPR. • Alternate calculations are Total Pulmonary Resistance which is resistance in the pulmonary circulation – as well as other organ and circulatory resistances can be calculated Formulas of Importance Diffusion – net movement of certain particles from a region of high concentration of those certain particles to region of low concentration of those certain particles D = A x Dc /t (Co – Ci) • A is the area of the membrane being diffused through, Dc is the diffusion coefficient, t- is the thickness of the membrane being diffused through, Co – Ci is the concentration difference between the o (outside) and I (inside) of the container • The diffusion coefficient = solubility coefficient divided by the square root of the molecular weight of the substance diffusing (this applies more to gases) • Analysis- the greater the area and/or diffusion coefficient – the faster the rate of diffusion. The more the concentration difference the faster the rate of diffusion. However, the thicker the membrane to diffuse through the slower the rate of diffusion. Formulas of Importance • Capacitance (Compliance) C – is the ease at which a container can stretch to accommodate increased volumes of gases or liquids. C = ∆V/∆P, • ∆P is change in pressure, and ∆V is change in volume • The more volume change without a change in pressure (due to compression of atoms and molecules in a minimally stretchable container) the greater the capacitance (compliance) • Thus a balloon would have greater capacitance (compliance) that a leather container. Laminar Flow Versus Turbulent Flow Laminar flow, sometimes known as streamline flow, occurs when a fluid flows in parallel layers, with no disruption between the layers. It is the opposite of turbulent flow. In nonscientific terms laminar flow is "smooth," while turbulent flow is "rough." Laminar Flow is a quiet smooth flow through blood vessels – whereas turbulent flow makes a noise as it flows – the more turbulent the flow the louder the noise. Turbulent flow produces murmur like sounds in the heart. A Bruit is the unusual sound that blood makes when it rushes past an obstruction (called turbulent flow) in an artery when the sound is auscultated with the bell portion of a stethoscope. A related term is "vascular murmur", which should not be confused with a heart murmur. Note- that once laminar flow hit the obstruction (like blood wall atherosclerotic plaque – it converted to turbulent flow. Reynolds number (Re) is the ratio of inertial forces to viscous forces and is given by the formula: Re = ρVD/μ where ρ = density of the fluid, V = velocity, D = pipe diameter, and μ = fluid viscosity. Reynolds number is used to determine whether a flow will be laminar or turbulent. If Re is high (>2100), inertial forces dominate viscous forces and the flow is turbulent; if Re number is low (<1100), viscous forces dominate and the flow is laminar. Determining if flow is Laminar versus Turbulent The Reynolds number is used to determine whether a flow will be laminar or turbulent. Reynolds number (Re) is the ratio of inertial forces to viscous forces and is given by the formula: Re = ρVD/μ where ρ = density of the fluid, V = velocity, D = pipe diameter, and μ = fluid viscosity. If Re is high (>2100), inertial forces dominate viscous forces and the flow is turbulent; if Re number is low (<1100), viscous forces dominate and the flow is laminar. Mean Arterial Pressure It is defined as the average arterial pressure during a single cardiac cycle. MAP (SYSTEMIC) = CO X TPR (SVR) MAP (SYSTEMIC) is the average pressure in the systemic circulation (Left Ventricle to Right Atrium). Thus MAP (pulmonic) can be calculated also as well as other circulations. CO is the cardiac output = heart rate x stroke volume (stroke volume is End Diastolic Volume – End Systolic Volume) TPR (SVR) is the total resistance in the systemic circulation MAP (SYSTEMIC) = CO X TPR (SVR) • This formula is an excellent one to use to understand pressures in the blood vessels. It can explain hypertensive pressures, normotensive pressures and hypotensive pressures. However, it cannot be actually calculated in that the TPR cannot be calculated. TPR in involves calculating the radius of the blood vessels at each millimeter along the circulation – the human body has approximately 60,000 miles of blood vessels – thus this is impossible to calculate. • The algebraic formula used to calculate MAP is MAP = DBP + 1/3 (SBP – DBP) DBP is the Diastolic Blood Pressure, and SBP is the Systolic Blood Pressure SBP – DBP is the Pulse Pressure MAP = DBP + 1/3 (SBP – DBP) Systolic Blood Pressure – occurs during Ejection Contraction Time The Diastolic Blood Pressure has more weight (significance) in this formula – because during one cardiac cycle there is more time spent in diastole in the blood vessels than is systole. The actual way MAP is calculated by the computer (arterial line) is using differential Calculus. Differential calculus exactly calculates the area under a curve. Blood Vessel Wall Tension • Tension = Pressure inside vessel x r/ 2 • r is radius of the vessel • Interpretation: For a given blood pressure, increasing the radius of the blood vessel leads to a linear increase in tension. This implies that large arteries must have thicker walls than small arteries in order to withstand the level of tension. Arteries 1. Elastic (Conducting) Arteries – first vessels to leave heart – act as a second pump – since the heart is an intermittent pump. (Aorta, Common Carotids, Subclavian, Common iliacs and pulmonary trunk) 2. Muscular (Distributive) Arteries arteries with considerable smooth muscle in the walls – thus can vasoconstrict and channel (distribute) blood to organs that need it. The muscular arteries include almost all of the arteries in the body besides those of the elastic – these arteries are large, medium and small. 3. Arterioles (Resistance Vessels) • very, very tiny artery with a diameter of 0.1mm or less – but considerable smooth muscle in the wall – can perform considerable vasoconstriction (resistance). 4. Capillary and Capillary Bed • True capillary (three types) continuous, fenestrated and sinusoidal – degree of permeability makes the difference • Metarteriole – tiny blood vessel with space intermittent smooth muscle in its wall – generally its entrance is guarded by a precapillary sphincter • Precapillary sphincter – valve type structure comprised of surrounding smooth muscle at the entrance of metarterioles and true capillaries • Thoroughfare channels – anatomic structure with very low resistance and not guarded by a precapillary sphincter – leads to venules Capillaries are the exchange (diffusion) vessels. There are millions of capillary beds in the body. Each population cells needs a capillary bed in order to get oxygen and nutrients. The true capillary and the associated capillary bed are excellent for diffusion because (1) they have very thin walls (2) a large cross sectional area to diffuse through and (3) the large cross sectional area slows the velocity of flow (4) they are narrow in diameter (10 μm - 30 μm) therefore less distance from lumen to membrane. Because they are narrow in diameter – this could significantly increase the resistance – but the parallel arrangement reduces this. D = A x Dc /t (Co – Ci) Capillary • The the peripheral circulation of the whole body has about 10 billion capillaries with a total surface area estimated to be 500 -700 square meters (about 1/8th the surface area of a football field). It is rare for any functional cell of the body to be more than 20 – 30 micromillimeters from a capillary – definitely no more than 100 micromillimeters. Blood Flow Through Capillaries • Vasomotion – Slow and intermittent flow – Reflects the on/off opening and closing of precapillary sphincters Parallel arrangement of vessels reduces resistance. R = 1/R1 + 1/R2 + 1/R3 Capillary bed has very slow velocity of flow due to its large cross sectional area. Figure 19.13 Capillaries The three anatomical types of capillaries differ in the degree of permeabilities Three anatomical types 1. Continuous capillaries (least permeable) 2. Fenestrated capillaries (medium permeability) 3. Sinusoidal capillaries (sinusoids) – very permeable Continuous capillary Fenestrated capillary Sinusoidal Capillary Figure 19.3 Continuous Capillaries • Abundant in the skin and muscles – Tight junctions connect endothelial cells – Intercellular clefts allow the passage of fluids and small solutes • Continuous capillaries of the brain & Thymus – Tight junctions are complete, forming the bloodbrain barrier and in the thymus Gland- forming the blood-thymic Barrier – In brain the capillaries are surrounded by astrocytes and in the thymus surrounded by reticular epithelial cells Continuous capillary Least permeable capillaries found in skin and muscles. Blood – Brain barrier and Blood- Thymic Barrier have even less permeability. Figure 19.3a Fenestrated Capillaries • Some endothelial cells contain pores (fenestrations) • More permeable than continuous capillaries • Function in absorption or filtrate formation (small intestines, endocrine glands, and kidneys) Fenestrated Capillary Have more permeability – found in small intestine and endocrine glands, kidneys Figure 19.3b Sinusoidal Capillaries • Fewer tight junctions, larger intercellular clefts, large lumens • Usually fenestrated • Allow large molecules and blood cells to pass between the blood and surrounding tissues • Found in the liver, bone marrow, spleen Sinusoidal Capillary Have considerable permeability – found in liver, spleen, bone marrow and adrenal medulla Figure 19.3c What routes do substances enter and exit the capillaries? 1. Diffusion through the endothelial cells (transcellular) - transudative 2. Diffusion between the endothelial cells (exudative) 3. Movement through the fenestra 4. Movement using pinocytotic Vesicles (pinocytosis). Figure 19.15 Capillary Exchange of Respiratory Gases and Nutrients • Diffusion of – O2 and nutrients from the blood to tissues – CO2 and metabolic wastes from tissues to the blood • Lipid-soluble molecules diffuse directly through endothelial membranes (Transudative) • Water-soluble solutes pass through clefts and fenestrations (Exudative) • Larger molecules, such as proteins, are actively transported in pinocytotic vesicles or caveolae Understanding the significance of the capillary Slide 1 As you should be aware of – the blood circulation, unlike the lymphatic circulation, is a continuous loop – a continuous set of pipes from the heart and back to the heart. The purpose of the bloodstream is to act as a transportation system -transporting good fresh materials to the tissue cells and picking up the tissue cells’ waste so as to transport these substances to the organs (kidneys, sweat glands, etc) that can excrete them from the body. Understanding the significance of the capillary Slide 2 The entrance into and out of the bloodstream for the fresh substances and waste is by simple diffusion. Diffusion (Diffusion Equation) occurs best through a barrier that is thin (the capillary wall). If blood goes into a pipe that is thin – it will unload its fresh products there and pickup waste there – it has no choice but to do this- it does not have a brain that gives it a choice where to pickup and deliver substances– just wherever the wall is thin enough. Thus the blood cannot enter a thin walled pipe unless it is ready to unload and load substances. Understanding the significance of the capillary Slide 3 Therefore, if the cells in the toe (for example) need some fresh substances and/or need to unload waste – the blood going to the toe should not enter a thin walled pipe (capillary) till it gets to the toe. Thus the blood needs to stay in the thicker walled pipes (arteries, arterioles) on the way to the toe capillaries (thin walled) – unload the fresh stuff and pick up the waste – then again enter a thick walled pipe (veins) till it gets to the area where it will unload the waste. Understanding the significance of the capillary Slide 3 In our continuous loop circulation - the capillaries act as the exchange vessels. All the other blood vessels from the heart (arteries and arterioles) and back to the heart (venules and veins) are conduit vessels (hallways) getting the blood to the main area of work for the bloodstream – the capillaries where all the fresh materials needed for tissue cells exits the bloodstream and all of the waste enters the bloodstream. Net Filtration Pressure The next slide will explain how water enters and leaves the capillaries. There are many substances that enter and leave the capillaries (gases, nutrients, hormones, etc.) using simple diffusion – but net filtration pressure only explains how water enters and exits the capillaries. Starling’s Law of the Capillaries states that the amount of water exiting the capillary should equal the amount of water reentering the capillary. If more water exits the capillary than reenters – edema occurs in that area. On the other hand if more enters that leaves that area becomes dehydrated. Net Filtration Pressure Calculation NFP = (Amount of Fluid out of capillary) – (Amount of Fluid Reentering capillary) NFP is generally calculated at two locations – at the arteriolar end of the capillary (water exit location) and at the more distal venous end of the capillary (water reentry into capillary location) ------------------------------------Forces out of capillary are (1) Hydrostatic (water) pressure of the blood – which is the mean arterial pressure (average blood pressure) – this pressure pushes water out of the capillary and (2) osmotic Pressure of the surrounding tissue fluids – sucking the water out of the blood vessels. Forces into capillary are (1) Hydrostatic (water) pressure of the surrounding tissue fluids – pushing water into the capillary and (2) osmotic pressure of the blood – sucking water back into the capillary. Arteriole Venule Interstitial fluid Net HP—Net OP (35—0)—(26—1) Net HP 35 mm Capillary Net OP 25 mm NFP (net filtration pressure) is 10 mm Hg; fluid moves out Net HP—Net OP (17—0)—(26—1) Net HP 17 mm Net OP 25 mm NFP is ~8 mm Hg; fluid moves in HP = hydrostatic pressure • Due to fluid pressing against a wall • “Pushes” • In capillary (HPc) • Pushes fluid out of capillary • 35 mm Hg at arterial end and 17 mm Hg at venous end of capillary in this example • In interstitial fluid (HPif) • Pushes fluid into capillary • 0 mm Hg in this example OP = osmotic pressure • Due to presence of nondiffusible solutes (e.g., plasma proteins) • “Sucks” • In capillary (OPc) • Pulls fluid into capillary • 26 mm Hg in this example • In interstitial fluid (OPif) • Pulls fluid out of capillary • 1 mm Hg in this example Figure 19.17 Net Filtration Pressure is a calculation for fluid transfer into and out of capillaries Figure 19.16 • NFP (arterial end) = (35 mm Hg + 1mm Hg) - (26 mmHg + 0) = 10 out • NFP (venous end) = (17 mmHg + 1 mmHg) – (26 mm Hg + 0) = 8 in • At the arterial end of a bed, hydrostatic forces dominate (fluids flow out) and at the venous end forces dominate back into blood vessel – however more fluid does exit than comes back in – the role of the lymphatics is to correct that amount. The lymphatics return the excess fluid to the circulation. Now hopefully, you can understand that if the lymphatics are blocked in a certain area of the body, that area will swell (edema). Venules, Veins • Vein (capacitance vessels) – a blood vessel that returns blood back to the heart. As with arteries – there are different types of veins. • By the time the blood has reached the veins it is fairly devoid of pressure – so the dependent veins (veins below the heart) need external compression to bring blood back to heart – they also need valves. Venules • Formed when capillary beds unite • Very porous; allow fluids and WBCs into tissues • Postcapillary venules consist of endothelium and a few pericytes • Larger venules have one or two layers of smooth muscle cells Veins • Formed when venules converge • Have thinner walls, larger lumens compared with corresponding arteries • Blood pressure is lower than in arteries • Thin tunica media and a thick tunica externa consisting of collagen fibers and elastic networks • Called capacitance vessels (blood reservoirs); contain up to 65% of the blood supply C = ∆V/∆P Pulmonary blood vessels 12% Systemic arteries and arterioles 15% Heart 8% Capillaries 5% Systemic veins and venules 60% Veins are our capacitance vessels – they contain most of the blood in the body at any given time. Figure 19.5 Little to no pressure in veins – so hard to get venous return to In the dependent body areas. Figure 19.5 Need external compression and valves to assist blood back to the heart in the dependent body areas (areas of the body below the heart) If blood cannot come back to the heart get “venous stasis”. This could lead to Deep Venous Thrombosis or Varicose Veins. Figure 19.6 Differences Between Arteries and Veins Arteries Veins Delivery Blood pumped into single systemic artery—the aorta Blood returns via superior and interior venae cavae and the coronary sinus Location Deep, and protected by tissues Both deep and superficial Pathways Fairly distinct Numerous interconnections Supply/drainage Predictable supply Usually similar to arteries, except dural sinuses and hepatic portal circulation Vascular Anastomoses • Interconnections of blood vessels • Arterial anastomoses provide alternate pathways (collateral channels) to a given body region – Common at joints, in abdominal organs, brain, and heart • Vascular shunts of capillaries are examples of arteriovenous anastomoses • Venous anastomoses are common • End Artery – when only one artery goes to an area (kidney for example) no collateral THE PULSES Pulse • The pulse rate generally is the same as the heart rate – thus normal resting pulse rate is between 60 and 100. • The pulse pressure is the difference between the systolic blood pressure and the diastolic pressure – generally equal to slightly greater than 40 mmHg. Various conditions can lower or elevate the pulse pressure. Low blood volume can decrease pulse pressure, exercise may temporarily elevate pulse pressure and stiffness of major arteries may consistently elevate the pulse pressure. Strengths of Palpable Pulse • • • • • 0 = Absent 1 = Barely palpable 2 = Easily palpable 3 = Full 4 = Aneurysmal or Bounding pulse Pulse • The pulse represents the tactile arterial palpation of the heartbeat (whether normal or abnormal) • The pulse may be palpated in any place that allows an artery to be compressed against a bone such as at the neck (carotid artery), at the wrist (radial artery), behind the knee (popliteal artery), on the inside of the elbow (brachial artery), and near the ankle joint (posterior tibial artery). Figure 19.11 Pulse • Pressure waves generated by cardiac systole move the artery walls, which are pliable and compliant. These properties form enough to create a palpable pressure wave. • The Heart Rate may be greater or lesser than the Pulse Rate depending upon physiologic demand. In this case, the heart rate are determined by auscultation or audible sounds at the heart apex, in which case it is not the pulse. The pulse deficit (difference between heart beats and pulsations at the periphery) is determined by simultaneous palpation at the radial artery and auscultation at the heart apex. Pulse Pressure The alternating expansion (ejection contraction) and contraction (diastole) of the arteries during a heart beat causes the pulse. The further an artery is away from the heart – the less the alternating Expansion and contraction – due to resistance – the magnitude of the pulse will The pulse pressure is the difference between the systolic blood pressure and the diastolic blood pressure Abnormal Pulses 1. Pulsus alternans - a physical finding with arterial pulse waveform showing alternating strong and weak beats. It is almost always indicative of left ventricular systolic impairment, and carries a poor prognosis. 2. Pulsus bigeminus - a cardiovascular phenomenon characterized by groups of two heartbeats close together followed by a longer pause. The second pulse is weaker than the first. It is caused by premature contractions ventricular contractions (PVCs). 3. Pulsus bisferiens, a sign where, on palpation of the pulse, a double peak per cardiac cycle can be appreciated. Bisferious means striking twice. Classically, it is detected when aortic prolapse with regurgitation exists in association with aortic stenosis, but may also be found in isolated but severe aortic regurgitation , and hypertrophic obstructive cardiomyopathy (idiopathic hypertrophy of heart muscle). 4. Pulsus tardus et parvus, (slow-rising pulse) a sign where, upon palpation, the pulse is weak/small (parvus), and late (tardus) relative to its usually expected character. It is seen in aortic valve stenosis. 5. Pulsus paradoxus is an exaggeration of the normal variation during the inspiratory phase of respiration, in which the blood pressure declines as one inhales and increases as one exhales. It is a sign that is indicative of several conditions including cardiac tamponade, pericarditis, chronic sleep apnea, and obstructive lung disease (e.g. asthma, COPD). Blood Pressure Control See Blood Pressure Control PowerPoint TAKING A BLOOD PRESSURE See the PowerPoint Blood Pressure Determination Shock See Shock PowerPoint Hypertension See Hypertension PowerPoint Serum Lipid Transfer See PowerPoint on Serum Lipid Transport Anatomy of the Circulatory System Figure 19.18a Figure 19.18b Figure 19.19 Figure 19.20a Figure 19.20b Figure 19.21a Figure 19.21b Figure 19.21c, d Figure 19.21d Figure 19.22a Figure 19.22b Figure 19.23a Figure 19.23b Figure 19.23c Figure 19.23d Figure 19.24a Figure 19.24b, c Figure 19.25a Figure 19.25b Figure 19.26a Figure 19.26b, c Figure 19.26b Figure 19.26c Figure 19.27a Figure 19.27b Figure 19.28a Figure 19.28b Figure 19.28c Figure 19.29a Figure 19.29b, c