Ch 18 Psychiatric Disorders
advertisement

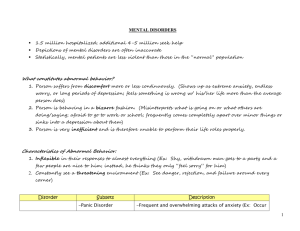
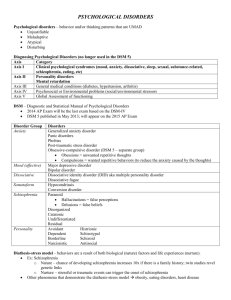
Ch 18 Psychiatric Disorders Psychiatric Disorders Disorders of psychological function sufficiently severe to require treatment Diagnosis can be difficult Patients with the same disorder can display different symptoms Patients with different disorders can display many of the same symptoms Diagnosis based on info from the DSM (Diagnostic & Statistical Manual of the American Psychiatric Association) Psychiatric Disorders Schizophrenia Affective Disorders: Depression & Mania Anxiety Disorders Tourette Syndrome Schizophrenia Means “splitting of psychic functions” The disorder most commonly associated with madness Affects 1% of the population Typically begins in adolescence or early adulthood Complex & diverse symptoms that overlap with those of other disorders Symptoms frequently change during progression of the disorder No single symptom appears in all cases Schizophrenia Symptoms split into 2 categories: 1. Positive: Symptoms that seem to represent an excess or distortion of normal function 2. Negative: Symptoms that seem to represent a reduction or loss of normal function Positive Symptoms of Schizophrenia Delusions Delusions of being controlled, persecution, or grandeur Hallucinations Imaginary voices making critical comments or telling the individual what to do Inappropriate affect Failure to react with the appropriate emotion to events Incoherent speech or thought Illogical thinking, echolalia (vocalized repetition of some or all of what was heard), peculiar associations among ideas, belief in supernatural forces Odd behavior Difficulty performing everyday tasks, lack of personal hygiene, talking in rhymes, catatonia (remaining motionless, often in awkward positions) Negative Symptoms of Schizophrenia Affective flattening Reduction or absence of emotional expression Alogia Reduction of absence of speech Avolition Reduction or absence of motivation Anhedonia Inability to experience pleasure Causal Factors in Schizophrenia Genetic component But experience also plays a role Some people inherit a potential for the disorder & it may or may not be activated based on experience Factors that can contribute to the development of schizophrenia Birth complications, early infections, autoimmune reactions, toxins, traumatic injury & stress Dopamine Theory of Schizophrenia First suggested by the fact that early antipsychotic drugs (chlopromazine & reserpine) caused motor effects like those of Parkinson’s Theory that schizophrenia is caused by the presence of too much dopamine Amphetamine & cocaine, which increase dopamine, can cause schizophrenic episodes in healthy people Dopamine Theory of Schizophrenia Discovery that there are 5 subtypes of dopamine receptors (D1-D5) Drugs worked in different ways because they acted on different receptor subtypes Schizophrenia is caused by hyperactivity specifically at D2 receptors Widely accepted, but still doesn’t explain the whole picture Neuroleptics: antischizophrenic drugs Higher affinity for D2 correlates to effectiveness Limitations of the Dopamine Theory 4 key discoveries that cannot by explained by the D2 version of the theory: 1. Receptors other than D2 are involved Glutamate, GABA & 5-HT Atypical neuroleptics developed to act on these non-D2 receptors (ex: clozapine) 2. It takes weeks of neuroleptic therapy to alleviate symptoms Despite the fact that neuroleptics can block activity at D2 receptors within hours Limitations of the Dopamine Theory 3. Schizophrenia is associated with widespread brain damage Not just limited to dopaminergic circuits 4. Neuroleptics are only marginally effective Not effective in all cases When they do have an effect, it is generally only on some of the symptoms More effective in treating the positive symptoms Affective Disorders: Depression & Mania Affective Disorders: Any psychiatric disorder characterized by disturbances of mood or emotion Aka mood disorders Depression Experiencing periodic depression is a normal reaction to loss However, some people have an increased tendency toward depression They repeatedly fall into deep despair & experience anhedonia (inability to experience pleasure), often for no apparent reason Depression Depression can be so extreme that it is almost impossible for them to complete necessary daily tasks (keep a job, relationships, eating, personal hygiene) Often have sleep issues & thoughts of suicide When this condition lasts over 2 weeks, it is classified as clinical depression or major depressive disorder Mania Mania: Characterized by overconfidence, impulsivity, distractibility & high energy Generally the opposite of depression During mild mania: Talkative, energetic, impulsive, positive & very confident Can be great at a job and/or very fun Full-blown mania: Unbridled enthusiasm, incessant talking that jumps topics, grandiosity, high energy, distractability, impulsiveness Often leads to disaster, failed relationships, unfinished projects Major Categories of Affective Disorders Bipolar affective disorder: Depressive patients who experience periods of mania Unipolar affective disorder: Depressive patients who do not experience mania Reactive depression: Depression triggered by a negative experience (a death, job loss) Endogenous depression: Depression with no apparent cause Probability of suffering from clinical depression during a lifetime is 10% Women 2x more unipolar affective disorder than men (bipolar equal) Risk of suicide in clinically depressed individuals is 5% Affects all ages Affective disorders associate with heart disease And bone loss in women Causal Factors in Affective Disorders Genetic factors Seasonal affective disorder (SAD): Attacks of depression & lethargy recur every winter Triggered by reduction of sunlight Light therapy can reduce symptoms Postpartum depression: Depression experienced by some women after giving birth Antidepressant Drugs 4 major classes of drugs for the treatment of affective disorders: 1. Monoamine oxidase inhibitors 2. Tricyclic antidepressants 3. Selective monoamine-reuptake inhibitors 4. Mood stabilizers Monoamine Oxidase Inhibitors (MAOIs) Monoamine agonist that increases the levels of monoamines by inhibiting the activity of monoamine oxidase (MAO), the enzyme that breaks down monoamine NTs MAO inhibitors have several side effects, including the cheese effect Consuming foods high in tyramine (cheese, wine, pickles) have risk of stroke from surges in blood pressure Tricyclic Antidepressants Named for the 3 rings of their chemical structure Work by blocking the reuptake of serotonin & norepinephrine Safer than MAOIs Selective Monoamine-Reuptake Inhibitors Selective serotonin-reuptake inhibitors (SSRIs): Serotonin agonists that block the reuptake of serotonin from the synapse Prozac, Paxil, Zoloft, etc. Few side effects Act against a wide range of psychological disorders in addition to depression Selective norepinephrine-reuptake inhibitors (SNRIs) Mood Stabilizers Developed because other antidepressants often triggered mania Mechanism of action is unknown Ex: Lithium (a metallic ion) Brain Pathology & Affective Disorders MRI studies have shown reductions in overall brain size & in many different brain structures in bipolar patients However, lots of variation 2 structures are often abnormal: Amygdala Anterior cingulate cortex (and often the connections between them) Monoamine Theory of Depression Depression is associated with underactivity at serotonergic & noradrenergic synapses Largely based on the fact that many of the drugs found to alleviate depression work as agonists of 5HT, NE or both Up-regulation: A compensatory increase in # of receptors for a NT when there is an insufficient amount of that NT released at a synapse Autopsies of clinically depressed individuals often have more 5-HT & NE receptors than normal Diathesis-Stress Model of Depression Some people inherit a diathesis (genetic susceptibility) & stress exposure in early life causes them to be permanently sensitized, causing them to overreact to mild stressors for the rest of their lives The diathesis alone cannot initiate the disorder Indirect evidence Depressed individuals release more stress hormones Treatment of Depression with Brain Stimulation Significant therapeutic effects of chronic brain stimulation through an implanted electrode Stimulates the anterior cingulate gyrus Permanently embedded under the skin to give continual pulses Extreme measure given to those who do not respond to conventional treatments Anxiety Disorders Anxiety: Chronic fear that persists in the absence of any direct threat Psychological correlate of stress Adaptive when it motivates effective coping behaviors Maladaptive when it is so severe it disrupts normal functioning (anxiety disorders) Anxiolytic: anxiety reducing Anxiogenic: anxiety provoking Anxiety Disorders All anxiety disorders associated with feelings of anxiety (fear, worry, despondency) & variety of physiological stress reactions (tachycardia, hypertension, nausea, breathing difficulty, sleep disturbances, high glucocorticoid levels) Most prevalent psychiatric disorder 17% of people have one at some point in their lives Women 2x 5 Classes of Anxiety Disorders 1. Generalized Anxiety Disorders: Characterized by stress responses & extreme feelings of anxiety that occur in the absence of any obvious reason 2. Phobic Anxiety Disorders: Similar to GAD but triggered by a specific object (ex: spiders, dogs) or situation (ex: flying, darkness) Agoraphobia: pathological fear of public places & open spaces 3. Panic Disorders: Characterized by rapid-onset attacks of extreme fear & severe symptoms of stress (choking, heart palpitations, shortness of breath) 5 Classes of Anxiety Disorders 4. Obsessive-Compulsive Disorders: Characterized by frequently recurring, uncontrollable, anxiety-provoking thoughts (obsessions) & impulses (compulsions) The compulsive behavior is done to alleviate the anxiety associated with the obsessions 5. Posttraumatic Stress Disorder: Persistent pattern of psychological distress following exposure to extreme stress (ex: war, sexual assault) Etiology of Anxiety Disorders Genetic component Large experiential component Because the anxiety often has an identifiable trigger, it is easier to assess the influence of experience in these types of disorders Pharmacological Treatment of Anxiety Disorders 3 categories of drugs 1. Benzodiazepines Most widely prescribed psychoactive drugs Ex: Valium Several adverse side effects Highly addictive; so only for short-term use Thought to work by agonizing GABA receptors 2. Serotonin Agonists Advantage of specificity; doesn’t cause the side effects associated with benzos But does have its own side effects 3. Antidepressant Drugs Common comorbidity (tendency to occur together in the same individual) of depression & anxiety Neural Bases of Anxiety Disorders Substantial overlap in brain areas involved in anxiety & affective disorders Amygdala, anterior cingulate cortex But with anxiety disorders, there is no gross damage (as opposed to shrinkage with affective) Increased activity in the amygdala of a phobic patient when shown a picture of ex: a spider Tourette Syndrome A disorder of tics Involuntary, repetitive, stereotyped movements of vocalizations Many people with this disorder have no symptoms other than tics Typically begins in childhood with simple motor tics (blinking), with symptoms growing more complex & severe with age (hitting, hopping, lewd gestures) Verbal tics can include barking, grunting, cursing (coprolalia), echolalia Symptoms usually reach a peak after a few years & often subside as the patient matures Tourette Syndrome 0.7% of the population 3x more frequent in males Major genetic component Some patients also have ADD/ADHD and/or OCD Although tics are involuntary, they can be temporarily be suppressed with great effort from the patient Neuropathology of Tourette Syndrome Very difficult to study People with this disorder often have smaller caudate nuclei Some evidence of thinning in sensorimotor cortex areas that control the face, mouth & voice box Treatment of Tourette Syndrome Tics usually treated with neuroleptics Can reduce tics by about 70% However, often patients won’t take them because of the adverse side effects