Sarah Berglas - Canadian Agency for Drugs and Technologies in

Lecture Series acmts.ca │ @acmts_cadth
#CADTHTalks
Using Patient
Perspectives to
Frame HTAs
SARAH BERGLAS
PATIENT ENGAGEMENT OFFICER, CADTH
APRIL 2015
Canadian Drug Expert Committee (CDEC) reflects
What is the value of the new drug, as compared to existing options?
Patient important outcomes are included in CADTH’s protocol
Methodology
Patient Input
Summary
CADTH Review
Protocol
Clinical Trials
CDEC
Recommendation
& Reasons
❶ ❷ ❸
Repeated x30 sequential CDR reviews
❹
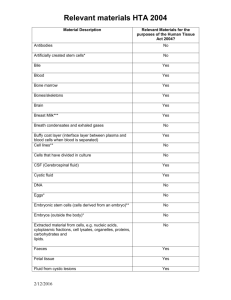
Drug Indication
Dificid
Xiaflex
C. difficile infection
Dupuytren's contracture
Eliquis Stroke prevention
Kalydeco Cystic fibrosis
Esbriet
Aloxi
Pulmonary fibrosis
Chemo nausea
Orencia RA
Seebri
Stribild
COPD
HIV
Soliris aHUS
Bystolic Hypertension
Humira Juvenile arthritis
Tecfidera MS
Sublinox Insomnia
Afinitor Tuberous sclerosis
Drug Indication
Fycompa
Edarbi
Epilepsy
Hypertension
Edarbyclor Hypertension
Fibristal Uterine fibroids
Picato
Latuda
Genotropin
Actinic keratosis
Schizophrenia
Growth hormone deficiency
Jetrea
Simponi
Inspra
Actemra
Vitromacular adhesion
Ulcerative colitis
Heart failure
Juvenile arthritis
Neupro
Botox
Parkinson's disease
Chronic migraine
Tudorza Genuair COPD
Galexos Hepatitis C
Final recommendations published March 2013 – June 2014
Results
Patient Input
Summaries
CADTH Review
Protocols
119 things that matter to patients
89 / 119 included
75%
Clinical Trials
61 / 119 included
50%
CDEC
Recommendation
& Reasons
67 / 119 included
56 %
FEAR
EMBARASSMENT
DEPENDENCY
GUILT
Lecture Series acmts.ca │ @acmts_cadth
#CADTHTalks
Involving patients in early stages of the HTA process: a participatory research project
Marie-Pierre Gagnon, 1,2 * Bernard Candas, 3 Marie Desmartis, 1 Marc
Rhainds, 4 Martin Coulombe, 4 Geneviève Asselin, 4,5 Daniel La Roche, 4
Johanne Gagnon, 1,2 France Légaré 1,5
1 Quebec University Hospital Research Centre, Québec, Canada
2 Faculty of Nursing, Laval University, Québec, Canada
3 National Institute of Public Health, Quebec, Canada.
4 HTA Unit, CHU de Québec-Université Laval, Québec, Canada
5 Faculty of Medicine, Laval University, Québec, Canada
Acknowledgements
This project is supported through a Knowledgeto-Action grant from the CIHR
We wish to thank all project participants, especially those involved in the prioritization process
We are grateful to Geneviève Asselin,Mylène
Tantchou Dipankui, Liette D’Amours and
Isabelle Ganache for their support
Background
The selection of HTA topics, which includes identifying and prioritizing HTA questions, is a constant challenge for decision-makers
Patient and public involvement (PPI) in the selection of HTA topics makes it possible to counterbalance the value judgments and preferences brought by variety of stakeholders
(e.g. scientists, health professionals)
More likely to be relevant to them and adapted to their needs
Background
The cancer field generates a vast array of questions and issues that encompass the full range of services and health policies, ranging from primary prevention, treatment, and expansive drug provision to palliative care.
Thus PPI in HTA in the cancer field appears particularly relevant.
Objective
To describe and evaluate the process and the results of interventions aiming to involve patient representatives alongside health professionals and managers in the identification and prioritization of HTA topics in the cancer field
Methods
A collaborative study with knowledge users from the HTA Unit of the CHU de Québec and the HTA Roundtable of the Integrated University
Health Network of Université Laval
Methods
Involvement strategies included
Consultation about potential HTA topics in the cancer field
Consensus meeting to reach agreement on top priorities
Evaluation of the prioritization activity
Based on a qualitative approach
• semi-structured interviews (11) and observation of the prioritization meeting
Analysis of prioritized topics
• at the end of the meeting vs. before the meeting
• according to the categories of stakeholders
Selection process and results
Suggestion of topics
• Email invitation to propose HTA topics sent to 75 clinicians and health managers + 25 community groups
• 30 proposals received from 20 different participants, some of them formulated after consulting other people
Filtering of topics and creation of vignettes
• 17 proposals that did not address the HTA program
• Honing of other proposals: 12 HTA questions
• Creation of vignettes for these 12 HTA topics
Prioritization exercice
• Pre-meeting survey (13 R)
• Consensus meeting (11 participants):
• First prioritization exercise in 2 groups: 4 topics selected
• Second exercise in 1 group: 6 topics selected
• Final individual exercise: 3 topics emerged
Results – Suggestion of HTA topics
30 proposals received (including 7 from community groups)
12 HTA topics developed (vignettes)
40% of topics were usable (12/30)
29% of topics suggested by patient representatives (2/7) were usable
Results – Pre-meeting survey
First priority topic :
"What is the best time to refer patients with advanced cancer to the palliative care team and to raise their awareness and the awareness of their family concerning this approach?"
Two topics in second position:
“Is early nutritional intervention recommended for cancer patients who need to receive chemotherapy and/or radiation therapy?”
“ What support interventions should be offered to caregivers of a cancer patient?
”
Prioritization meeting: process
Welcoming address and presentation of the study
Briefing session about HTA
Prioritization exercise in two groups: four topics selected in each group
Prioritization exercise in one group: six topics selected
Final individual prioritization exercise: use of chips equivalent to the number of topics selected. Participants distributed the chips among the six topics in such a way as to reflect their relative priority for them.
Results – HTA priorities emerging from the consensus meeting
1
2
3
4
5
6
Topics prioritized and individual votes Community group
Nb of votes (% )
What are the benefits of group meetings with an interdisciplinary team in oncology (including a community group representative) as regards providing support for new cancer patients?
16 (53%)
11 (37%)
What are the most effective strategies used to invite people to participate in cancer screening programs?
2 (7%)
Should teleconsultation be recommended for the preliminary evaluation and follow-up of cancer patients in rural and remote areas?
1 (3%)
Would offering patients in cancer remission a program to adopt healthy lifestyle habits reduce the risk of recurrence and improve their health and quality of life? And what form should this program take?
2 (6%)
What are the most effective ways to provide information prior to breast cancer surgical treatment concerning the treatment itself and its effects?
Which distress screening tool should be used for patients with cancer?
0
Health care professional and manager
Nb of votes (%)
9 (25%)
11 (31%)
12 (33%)
2 (6%)
2 (3%)
0
Total
Nb of votes
(%)
25 (38%)
22 (33%)
14 (21%)
3 (5%)
0
0
Results of interviews
Perceptions of the prioritization process
The diversity of participants (from the healthcare network and the community sphere) and of regions
provided complementary perspectives on patient trajectory and raised awareness of different regional realities
enabled rich exchanges that allowed participants to gain an overview on the topics to prioritize
But…
Various types of regions made it difficult to select topics relevant to all settings (5/11)
Results of interviews
Perceptions of prioritization process
Vignettes
Participants appreciated receiving them 10 days before the meeting to get ready for the meeting
Briefing session about HTA
enabled participants, especially participants from community groups, to learn the basics of HTA
provided a better understanding of the whole process, and the place of this prioritization activity
Consensus method for prioritization
allowed everyone to express his or her point of view, and hear the views of others while not preventing them from maintaining their positions
Results of interviews
Prioritization criteria
Criteria varied according to the type of participant
Community group representatives tended to favour topics related to patient support
(emotional, practical, etc.)
Clinicians and managers tended to favour topics linked to their clinical area or their management issues
Criteria were different because, as a manager, I had a certain vision concerning deficiencies, performance, and access, while they
[representatives of community groups] were more involved in patient support ... Interview # 2
Results of interviews
Criteria varied according to different regional realities:
Participants tended to favour an assessment that would lead to subsequent actions in a given context and thus have a real impact on patients in their regions (e.g. teleconsultation for remote regions)
Results of interviews
Input of patient organizations
Perspectives on the life of patients outside the hospital and on the support provided by the community and their families
Often represented the voice of vulnerable and isolated patients
Problem of “representativeness” of patients on such a committee = not easy to solve, as noted by one participant
Discussion
This study provides knowledge about the effects of involving various stakeholders in the selection of HTA topics and the impact of these strategies on the selection of HTA topics.
Discussion
Difficulties in recruiting enough participants for the prioritization committees as originally planned
Preparatory activities appreciated and perceived as useful
Distribution of vignettes 10 days before the meeting allowed participants to be well prepared
HTA briefing session: a prerequisite for participating in such an activity
Discussion
Impact of the consensus meeting
Allowed participants from diverse sectors and regions to share their knowledge and experience
Provided a better understanding of the topics to prioritize
Feasibility of the follow-up of recommendations = important criterion influencing priority of HTA topics
Input of representatives of community groups
provided perspectives on the life of patients outside the hospital and on the support provided by community and family
could give voice to the most vulnerable patients
Conclusion
Involving patient representatives in early steps of HTA is feasible
Patient representatives and caregivers have different perspectives from managers on topics to prioritize but could reach a consensus
Involving patient representatives in the selection process of HTA topics could modify the topics prioritized
Thank you!
Contact:
marie-pierre.gagnon@fsi.ulaval.ca
Lecture Series acmts.ca │ @acmts_cadth
#CADTHTalks
Moving Beyond Good
Intentions: Experience of a Saskatchewan
P
atient Family Advisory
C
ouncil
What does the evidence say?
Relationships with Commercial Interest: None
Grant/Research Support for initiatives being discussed: None
Speaker Bureau/Honoraria or external funding for initiatives being discussed: None
Consulting fees utilized: None
Memberships on advisory committees, boards: None
DISCLOSURES
Saskatchewan Cancer Agency:
Who We Are
The Saskatchewan
Cancer Agency is a provincial healthcare organization serving more than 1.1 million people.
SCA operates prevention and early detection programs, provides safe quality cancer treatment and conducts innovative research.
39
Saskatchewan Cancer Agency
We provide chemotherapy and radiation treatment as well as stem cell transplants:
6,413 new patient appointments in 2013-14
45,083 review patient appointments
22 allogeneic transplants and 44 autologous
16 COPS centers located in
10 health regions treating
1713 patients closer to home
40
SCA Patient Family Advisory
Council
Patient and Family Advisory Council
Partnership of Care
We Listen, We Care
At the Saskatchewan Cancer Agency, clients, patients and their families are at the very heart of our work. To ensure we are truly focused on meeting the needs of patients and families, we established the Patient and
Family Advisory Council. The Council helps us to blend the voices of patients and families with physicians and staff to provide excellent care and services.
What is Patient and Family - Centred Health Care
It is an approach to planning and delivering health care that recognizes and respects the patient and family as partners in the health care process.
It redefines the relationships that traditionally exist in health care. Patient and family – centred care is the kind of care you and a family member will receive at the Saskatchewan Cancer Agency.
It is based on:
Respect and dignity: Doctors and nurses listen to patient and family perspectives and choices.
Sharing information: Communicating and sharing information with patients and families in ways that are supportive and useful to allow patients to actively participate in their care.
Participation: Patients and families are encouraged and supported in participating in care and decision making at the level they choose.
Collaboration: Health care leaders work together with patients and families to improve their experience and care.
41
What does the evidence say?
Patient First 2009
That the health system make patient and family centred care the foundation and principal aim of the
Saskatchewan health system, through a broad policy framework to be adopted system-wide.
Developed in collaboration with patients, families, providers and health system leaders, this policy framework should serve as an overarching guide for health care organizations, professional groups and others to make the Patient First philosophy a reality in all work places.
42
What does the evidence say?
Person-and Family-Centered Care –
Putting the patient and the family at the heart of every decision and empowering them to be genuine partners in their care
Site visit and consultation:
43
What does the evidence say:
Canadian Partnership Against Cancer
Cancerview.ca
is a knowledge hub and online community that offers trusted, evidence-based content from more than 30 partner organizations in Canada. It also offers a wide array of tools and resources developed by the Partnership.
44
Involvement in the beginning
Engagement was about forming as a council learning about who we are as a
council.
Accomplishments:
Wireless internet in clinics
It was about getting things done and having concrete items to say we have achievements.
Involvement and presence in 35 activities, events, committees
Instituted comment boxes
Developing trust credibility.
Developed recruitment processes
45
Patients as part of the improvement team
46
“True” engagement?
Good Intentions: Making assumptions
We assumed that because we espoused PFCC everything would be PFCC and it would be smooth sailing…… What’s the issue?
Who’s not going to get it when patient voice is being expressed through a council?
When a staff member comes to council they will agree with us.
Engagement meant we invited patients and families into the room for discussion.
Staff : we can use acronyms and lingo with our patients and family members.
We are getting along well because we are accomplishing tangible changes that we can see.
Do patients and families have any role in policy changes?
We had representation from patients and families… they were in the room when we talked and didn’t disagree.
48
Growing and learning….
As PFAC matured, and we had built trust with each other so we felt comfortable to challenge and question each other.
We asked staff to come as guests to present to us on areas of their expertise.
Staff were unclear on the role of PFAC when it came to change and implementation of ideas.
Some of the challenges were uncomfortable, unpleasant and PFAC was unsure what to do next.
We saw differences in how issues were being discussed, resolved or not resolved as we had worked with the easy stuff and now….
Good intentions?
Magazines and puzzles in waiting room areas
What does the evidence say?
51
Tuckman slide
Dr. Bruce Tuckman - 1965
52
Evidence from others
We learned from others across Canada and stole shamelessly such as Capital
Health, Alberta and Kingston, Ontario.
Conference attendance from our Council members.
Evidence on collaborative work and partnerships CPAC.
Our own PFCC forum in Saskatchewan.
53
Moving to engagement, collaboration and partnership
Conscious and thoughtful approach to ensure that involvement and engagement is appropriate and effective for each interaction.
For some, increased numbers of patient family members on a group or committee.
Clarification of roles PFAC member: working with leaders to know why patient family member involved: information, advice, decision making, and what does collaboration mean.
Started an annual interview process with our Council one by one and now moving to a more objective interview process with objective third party.
Orientation to events and SCA: phone call and letter about the engagement required.
Mentoring of members.
Surveys on engagement from patient perspective so we can continually improve.
54
Continuous Improvement: Taking stock – Interviews with members
Policy stakeholder
PFAC Policy/Procedure Review Process
Notification of Policy/procedure review which materially influences patient experience submitted to
PFAC Coordinator for inclusion on
PFAC meeting agenda
Draft policy/
Procedure included on PFAC meeting package
Content expert for the policy/ procedure makes presentation at PFAC meeting
Time period for review and feedback
YES
PFAC members send individual feedback to
PFAC Coordinator
PFAC Coordinator &
PFAC Chair summarize comments and submit to content expert
Content expert reviews
PFAC comments as well as those from other SCA stakeholders
Major edits/ changes required?
NO
Edits made and next draft of document re-submitted to
PFAC for subsequent review
PFAC Chair signs
Review and Sign
Off sheet on behalf of PFAC
56
Partnership for Patients and Families
57
Success isn’t easy
58
New frontiers
Patient charter
Surveys and interviews
Experience Based Design
Objective surveys for improvement with PFAC members
SCA strategic plan 201520: “ How is this plan informed by the principles of Patient and
Family Centered Care, and how are patients, families, and other stakeholders being engaged in the work?
”
59
Sources of evidence
Quantitative Data:
Published research
IHI, Patient First,
AOPSS,CPAC,
IPFCC, Cancer Care
Ontario. CMA, PRO
Qualitative Data
PFAC comments,
Interviews, Feedback,
Surveys, comment boxes, QCC, staff and physicians
Qualitative Data:
Conferences
EBD
Advocacy groups:
CCAN, STEM, SSCN
PFAC
Collaborative
Voice for change
60
Moving from good intentions
Moving from representation to engagement.
Listening for what is not being said.
Development of processes for collaborative work together.
Determine a reasonable approach for SCA and our work together that moves from “ask” and request to collaboration.
Defining collaboration and engagement together and roles of each other as we work forward for engagement.
Leveraging the great work from others.
We invite you to work WITH us as partners as we shape and improve our health system through true engagement with patients and families
Saskatchewan Cancer Agency
Patient and Family Advisory Council
62
Questions and Comments
Susan Bazylewski, Vice President Care Services
Saskatchewan Cancer Agency susan.bazylewski@saskcancer.ca
Louise Frederick, Chair – Patient & Family Advisory
Council pfac@saskcancer.ca
63
Lecture Series acmts.ca │ @acmts_cadth
#CADTHTalks