Operational Guidelines
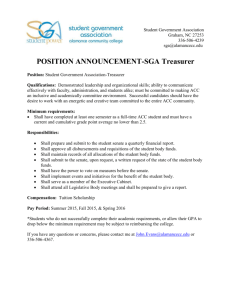
advertisement

Concussion Service Operational Guidelines July 2015 This is a living document and will be updated as required Concussion Service Operational Guidelines Contents Introduction to Concussion Services .................................................................................... 3 Purpose and philosophy ......................................................................................................... 3 Useful contact numbers ................................................................................................................ 4 Concussion Service Forms .......................................................................................................... 4 Responsibilities ........................................................................................................................ 4 Supplier responsibilities ................................................................................................................ 4 Client responsibilities .................................................................................................................... 5 ACC responsibilities ...................................................................................................................... 6 Communication protocols............................................................................................................. 7 Service Provision ..................................................................................................................... 8 Client eligibility ............................................................................................................................... 8 End to End Process Map ........................................................................................................... 10 Referral ......................................................................................................................................... 11 Investigation and Triage Process Map ..................................................................................... 13 Triage ............................................................................................................................................ 14 Service Administration .......................................................................................................... 18 Service location ........................................................................................................................... 18 Maximum duration ....................................................................................................................... 18 Timeframes................................................................................................................................... 19 Maximum funding limit ................................................................................................................ 19 Client non-attendance................................................................................................................. 20 Client exit ...................................................................................................................................... 21 Post-service client support ......................................................................................................... 21 Not included in the service ......................................................................................................... 21 Quality Management .............................................................................................................. 22 Supplier approval process ......................................................................................................... 22 Trainee health professionals ..................................................................................................... 22 Annual targets and best practice .............................................................................................. 23 Quarterly service monitoring ...................................................................................................... 23 Invoicing for travel ....................................................................................................................... 25 APPENDICES .......................................................................................................................... 28 Appendix 1: Bio-psycho-social model .......................................................................................... 28 Appendix 2: Continuum of care model......................................................................................... 30 Appendix 3: Risk assessment matrix ........................................................................................... 31 Appendix 4: Neuropsychological assessment guidelines ......................................................... 34 Adults with mild and moderate TBI ........................................................................................... 34 Children/adolescents with mild and moderate TBI ................................................................. 36 June 2014 Page 2 of 38 Concussion Service Operational Guidelines Introduction to Concussion Services The Concussion Service (CS) is an interdisciplinary traumatic brain injury (TBI) service consisting of assessments and therapies that support clients to recover and return to everyday life. It also aims to prevent long-term consequences such as post-concussion syndrome (PCS) by identifying clients at risk of PCS and giving them effective interventions and education. The Concussion Service is based on rehabilitation best practice and recognises the bio-psychosocial model. The service works holistically and adapts to provide services that best meet the rehabilitation needs of the client while recognising the legal responsibilities of ACC and the supplier. Purpose and philosophy Purpose The purpose of the service is to: provide early intervention rehabilitation to support recovery and prompt return to everyday life, including work or school identify clients likely to develop long-term consequences, such as post-concussion syndrome (PCS), and provide them with effective interventions and education. Philosophy The Concussion Service has three core philosophies. Individual needs Each person who sustains a brain injury responds differently, therefore rehabilitation needs can vary. ACC and suppliers will adapt services to get the best rehabilitation outcomes for the individual. Interdisciplinary team The Concussion Service is provided by an interdisciplinary team specialising in treating clients mild to moderate traumatic brain injuries. The service includes assessments and treatments that helps clients achieve a long-term recovery where they no longer need support from ACC. The full interdisciplinary team participates throughout. Regular group meetings are held to discuss the client’s rehabilitation progress and to identify their ongoing rehabilitation needs. Relationships ACC and suppliers work together to ensure client rehabilitation. This is achieved by maintaining close working ties through good communication, respecting each other’s areas of expertise, and fully engaging clients and their family/whānau in the recovery process to ensure the client gets the services they need in order to achieve independence. Service objectives ACC will measure the success of this service based on the following objectives: clients are returned to their usual activities of everyday life, including work or school, and no longer require any continued support from ACC for their brain injury June 2015 Page 3 of 39 Concussion Service Operational Guidelines services are provided in the shortest timeframe and at the lowest cost while maintaining clinical appropriateness clients report overall satisfaction with the services provided. Useful contact numbers Provider helpline Health Procurement Ph: 0800 222 070 Ph: 0800 400 503 providerhelp@acc.co.nz health.procurement@acc.co.nz The supplier helpline staff can answer queries relating to supplier numbers, Assessment Report and Treatment Plan (ARTP) updates and general enquiries. Health Procurement can advise on appropriate documentation in relation to applying for contracts. Concussion Service Forms All Concussion Service forms are available on the ACC website ww.acc.co.nz > Publications > Concussion page, or by searching the form number using the search box on the home page. ACC883 Concussion Service Referral Form ACC884 Concussion Service Client Summary Form ACC885 Concussion Services Did Not Attend report Responsibilities Supplier responsibilities The supplier is responsible: to… for… clients ensuring the education, assessment and therapy provided is appropriate to the diagnosis providing services promptly, for example: June 2015 o making the first appointment within 2 days of the referral being received o holding the first appointment within 5 days of the referral being received encouraging the client’s self-management and active participation in the rehabilitation process providing high quality assessments and treatment services ensuring the interdisciplinary team works together through all stages delivering services only when clinically necessary including the client’s family and whānau, where appropriate Page 4 of 39 Concussion Service Operational Guidelines to… for… ACC investigating when ACC requests clarification of the diagnosis nominating a key worker to have primary contact with ACC ensuring the client has a confirmed diagnosis prior to commencing therapy by o investigating prior clinical notes relating to the claim o conducting the appropriate clinical assessments to confirm the diagnosis as requested working within timeframes outlined in the service specification or as agreed with the case owner, including: o o conducting a client needs assessment submitting reports acting in a timely way to maximise the client’s rehabilitation outcome and keep weekly compensation costs down demonstrating commitment to the contracted outcome by completing section 12 of the ACC884 Client Summary o referrers (GPs) other service suppliers maintaining contact with the case owner (as agreed) to discuss changes or developments, e.g. change in symptoms or work readiness, or social, family, or financial issues etc., to help ACC support the client giving ACC a copy of any clinical information provided to or collected from the GP maintaining high quality clinical notes to: o support and verify any risk assessment or ACC884 Client Summary form information o aid decision-making for ACC and other suppliers as appropriate operating the service within the terms and principles of the Concussion Service contract and these Operational Guidelines providing timely and relevant clinical information to support the overall care of the client, such as: o assessment and treatment programmes including medication o rehabilitation plans for return to work recommending return to work time frames maintaining good working relationships based on respect for each other’s area of focus providing and receiving information appropriate to the situation and need. Client responsibilities The client is responsible for: attending appointments or rescheduling them when they are unable to attend, with reasonable notice participating in the rehabilitation process discussing any problems that may hinder their recovery with their case owner and supplier. June 2015 Page 5 of 39 Concussion Service Operational Guidelines ACC responsibilities ACC is responsible: to… for… clients ensuring they have the correct diagnosis and cover decision ensuring they get the appropriate services and support to help them rehabilitate and return to everyday life, including work or school making timely, efficient, and effective decisions making prompt decisions based on the available information or, if the information is unavailable, investigating as appropriate working with the supplier to rehabilitate the client agreeing new timeframes where the client’s needs cannot be addressed within the existing timeframe keeping them up to date of suppliers o any other assigned service suppliers such as vocational services o who the lead supplier is where services need to be coordinated o any delays or issues that may impact on service provision following up with the supplier if they have not been in touch as agreed seeking clarification from the supplier if progress and outcomes are not being achieved confirming the acceptance or decline of the referral keeping the GP informed of the client’s progress employers keeping them up to date with the client’s rehabilitation process and encouraging them to keep the client’s job available for a successful return to employment other service suppliers, eg Stay at Work or other vocational programmes keeping them informed of any relevant information for coordinating the rehabilitation process. referrers (GPs) June 2015 Page 6 of 39 Concussion Service Operational Guidelines Communication protocols Relationship expectations The rehabilitation partnership between the supplier and the case owner is one of the most important tools for ensuring the recovery of the client. Having the supplier and case owner working and communicating collectively will help with the client’s rehabilitation. To be effective this relationship needs to be based on mutual respect, open communication, agreed timeliness and quality agreed client outcomes There is an expectation that: suppliers and ACC case owners will work together to assist in the client’s rehabilitation both parties will respect each other’s area of expertise suppliers are experts in the rehabilitation of brain-injured clients and are responsible for achieving the service outcome for the client within the context of the Concussion service (as defined in the service specification) ACC case owners are expert at managing the complex mix of rehabilitation, entitlements, and compliance relating to claims ACC is ultimately responsible for funding rehabilitation services. The supplier will nominate a key worker to have contact with ACC. The key worker will: keep ACC informed of any issues regarding the provision of assessments or treatment raise any issues with the service and suggest solutions ensure all services are carried out in accordance with the service schedule and this operational guideline. represent the supplier in service performance discussions inform ACC promptly when any contact details change. Communicating instead of reporting Formal written clinical reports are not purchased in this service. The assessments determine the client’s requirements for the Concussion Service and are not intended to determine cover or entitlement, although they may be used to confirm diagnosis. Instead, suppliers are asked to convey to ACC case owner information that supports appropriate fact-based decision-making. Suppliers may choose to provide further support information as their own discretion. Where a diagnosis is very complex and a separate report is required ACC may choose to purchase this separately. This does not form part of the CS spend. The reporting structure in the Concussion Service highlights the importance of effective communication between ACC case owners and the supplier. Phone calls and emails should cover the following topics: the client’s current status the potential recovery timeframe and plan the impact of other issues on the client any recommendations or needs the supplier may have June 2015 Page 7 of 39 Concussion Service Operational Guidelines Service Provision Client eligibility The client can access the Concussion Service if referred by a medical practitioner or an ACC case owner. The client cannot be referred if the injury was more than 12 months before the referral and any subsequent treatment. The client cannot self-refer. To be referred by a medical practitioner the client: must… and… and… have an accepted ACC claim, and have on-going signs and symptoms such as: have additional risk factors such as: be diagnosed with or be suspected of having mood changes memory problems fatigue difficulty concentrating loss of balance headaches visual disturbances nausea muscular aches dizziness mild TBI, moderate TBI or postconcussion syndrome the inability to work or attend school for more than one week second or subsequent MTBI within six months post traumatic amnesia lasting more than 12 hours a requirement to operate machinery or drive at work a pre-existing psychiatric disorder or substance abuse problem a high functioning job such as engineer, medical practitioner or lawyer currently attending secondary or tertiary education Clinical diagnosis - severity of injury Clients diagnosed with a mild or moderate traumatic brain injury (TBI) are suitable for the Concussion Service. The table below is used to categorise TBI at the acute stage. Severity of injury Glasgow Coma Scale (GCS) Duration of Post-traumatic Amnesia (PTA) Mild 13-15 less than 24 hours Moderate 9-12 1-6 days Severe 3-8 7 days or more (Source: Evidence best practice guideline – traumatic brain injury: diagnosis, acute management and rehabilitation 2006 (TBI Guidelines) Note: If the GCS and PTA do not correlate the client will be assigned to the greater of the two severity categories. Example: A client has a GCS score of 14 and also experiences PTA of 2 days. Based on the more severe indicator (PTA of 2 days) the client is considered to have a moderate TBI. June 2015 Page 8 of 39 Concussion Service Operational Guidelines If notification of a TBI has been delayed but is less than 12 months after the injury, the case owner will check the GCS and PTA where provided, and any other information such as clinical notes, to review the concussion symptoms and decide if it is appropriate for the client to access the Concussion Service. ACC may refer the client to the Concussion Service to have the diagnosis investigated by the medical specialist. June 2015 Page 9 of 39 Concussion Service Operational Guidelines End to End Process Map The key to the Concussion Service is the flexibility to adapt to the needs of the client while remaining efficient and effective. The sections shown here of referral, assessment and therapy are not rigid or inflexible. The discussion and agreement between the supplier and ACC determines the appropriate route for the client. Referral Referral from GPs or A&M Clinics Concussion Service Supplier Referral from Medical or Allied Health Staff at DHB ACC Referral generated by ACC Sends the referral to the Concussion Service Supplier Unconfirmed Diagnosis Supplier Confirms Diagnosis 1. Collect clinical notes and interview client 2. Identify what further assessments are required to confirm the diagnosis via IDT 3. Discus with ACC to agree purchase order 4. Conducted the approved consulations to confirm diagnosis such as - medical specialist and/or - clinical neuropsychologist and/or - allied health - other specialist 5. Provide a written confirmation of diagnosis Recovered or Cover Declined TBI Diagnosis Confirmed Diagnosis Reported End Assessment (if not already assessed) ACC884 Client Summary Supplier Recommendation End Recovered ACC Supplier Assess the Client’s Need 1. Collect clinical notes and interview client 2. Identify what further assessments are required to assess the Client’s rehabilitation need via IDT 3. Discus with ACC to agree purchase order 4. Conducted the approved assessments such as - medical specialist and/or - clinical neuropsychologist and/or - allied health - other specialist 5. Develop rehabilitation plan Not Recovered Stay in CSS Not Recovered Exit CSS Therapy Treatment Services - Psychological Counselling - Medical Consultation - Allied Health Services ACC884 Client Summary Supplier Recommendation Recommendation in Client Summary: Other Services: The case manager selects other ACC treatment and rehabilitation Services such as - Vocation Services June 2015 Recommendation in Client Summary: (Big brother services) - ACC manages Client services (More targeted ongoing service provision) The case manager (with advice from ACC clinical professionals) selects other ACC treatment and rehabilitation Services such as - Neuropsychological Assessment Service - Clinical Services contract - Training for Independence - Psychological Counselling Service - Physiotherapy contract Page 10 of 39 Concussion Service Operational Guidelines The following table is a guide to use service item codes for the different activities in the service. Once again these should not be seen as rigid stages. Case owner and the supplier should discuss the client’s needs regularly. Stage Activities Service Items Codes Referral Investigation TBI21, TBI29 Diagnosis TBI23^, TBI24, TBI25 Risk assessment TBI21 Assessment of therapy needs TBI22, TBI23, TBI24, TBI25 Rehabilitation planning TBI21 Education TBI21 Notification TBI21, TBI29 Therapy & review TBI26, TBI27, TBI28 Notification TBI29 Assessment Therapy ^Physiotherapists have a number of tests that can differentiate TBI from physical injuries such as neck and shoulder injuries, such as the Treadmill Stress Test Time Availability Service Item Hours Variations TBI21 – Education & Assessment 3 TBI22 – Allied Health Assessment 2 Hours for all service items maybe varied in agreement with the case owner but must meet the following principles TBI23 – Neuropsychological Screen 5 - TBI24 – Medical Assessment 2 Multi-disciplinary services are required (single discipline needs are met under other contracts) - Rehabilitation plan fully explains the need for services, goals and expected outcomes and timeframes - Services do not exceed the maximum funding of $3,000 for the total service cost TBI25 – Other Specialists At cost TBI26 – Allied Health or Nursing therapy 8 TBI27 – Psychological Consultation 5 TBI28 – Medical Consultation 2 TBI29 – Key worker 4 Referral The referrer must only refer clients who - need and will benefit from the Concussion Service - have signs and symptoms of mild to moderate TBI or PCS - was injured within 12 months of referral ACC will also comply with the above criteria. The supplier should decline any referral that does not meet the above conditions. The referral form June 2015 Page 11 of 39 Concussion Service Operational Guidelines The referrer should use the ACC883 Concussion Service Referral form on the ACC website. DHB referrers must use the ACC883 Referral form and send it to their appropriate ACC Short Term Claims Centre. The ACC883 is an acceptable notification of a concussion where the form is signed by a medical practitioner. Letters of referral Some referrers use other formats such as a letter of referral. ACC does not consider them to - have sufficient detail, unless they are accompanied by clinical notes outlining presenting symptoms, pre-injury health status and any other potential rehabilitation impact - be an update to the diagnosis on the ACC45 The supplier and ACC will contact the referrer at every occasion recommending the use of the ACC883 Referral form and to send it to ACC. Who can refer? A medical practitioner or Allied Health Professional at a DHB: can refer a client to the Concussion Service by sending the completed ACC883 form to their appropriate ACC Short Term Claims Centre for consideration. There must be a confirmed diagnosis by a qualified medical professional in the client’s DHB clinical notes. A GP or Accident & Medical (A&M) Centre: can refer a client by sending the completed ACC883 or letter of referral with clinical notes to ACC directly or to a Concussion Service supplier who must forward it to ACC for approval. A case owner: can refer a client to the Concussion Service if they consider that the client may have sustained a TBI. The case owner also completes the ACC883 form to ensure the supplier receives consistent information and provide any other information relevant. If there has been no diagnosis of TBI by a medical professional, the case owner will request a medical assessment to confirm the diagnosis. Accept or decline If the referral meets the criteria ACC will notify the client directly and send the ACC883 referral form to the supplier to start the service. If the claim does not meet the criteria and is declined ACC will notify the referrer and the client. The supplier will be notified if the referral came via the supplier. June 2015 Page 12 of 39 Concussion Service Operational Guidelines Who cannot refer? Other clinical professionals, such as a physiotherapist in the community, cannot refer a client to the Concussion Service. They may, however, refer a client to a registered medical practitioner for a medical assessment, after which the client may be referred to the Concussion Service. Investigation The service item TBI21 is designed to allow the supplier to investigate both clinical and the psychsocial background of the client. The following process map shows the comprehensive investigation required under TBI21. Investigation and Triage Process Map TBI29 – Key Worker Administration (max. 2 hours) Supplier receives a referral directly from the referrer. Clause 3.2.5 Send the referral to ACC immediately and wait for response ACC investigates cover & entitlement ACC notifies supplier and referrer of the entitlement decision within 2 working days ACC makes a decision Confirm Acceptance of the referral with 1 working day Clause 3.2.8 Follow up if you haven’t heard from ACC within 2 working days Supplier rreceives a referral from ACC Supplier contacts the client and make an appointment within 2 days Operational Guidelines TBI21 – Investigation, triage & education (max. 3 hours) Summarise findings and provide summary and notes to full interdisciplinary team. (Med Spec, Clin Neuropsych & OT minimum) Clause 6.1 Supplier interviews the client Explain Rehabilitation process including investigation and confirmation of diagnosis if required. Clause 5.10.2 Contact DHB if referral from ED or other DHB service to obtain clinical notes Clause 5.10.3 Get permission to access previous medical records. Clause 5.10.3 and Hold an IDT meeting to discuss information. Summarise IDT opinions & recommendations in clinical notes. Clause 5.10.4, 6.1.4 Meet with client to review findings and develop rehabilitation plan including SMART goals & inputs Clause 5.10.5 Contact the GP get pre-injury clinical notes Clause 5.10.3 With the client’s permission contact the employer or school (as appropriate) Get clinical history from client. Clause 5.10.1 and and Ask about social factors and life impacts. Clause 5.10.1 Ask about goals, expectations and commitment to rehabilitation. Clause 5.10.5 Provide advice on symptom management. Where diagnosis unconfirmed do NOT provide education on TBI. Provide education on TBI when the diagnosis is confirmed. Clause 5.10.2 - Education Contact ACC to discuss IDT recommendations Request further assessments where required ACC discusses requirements and where appropriate updates the Purchase order June 2015 Conduct clinical assessments as required Meet with client to review findings and discuss rehabilitation plan including SMART goals & inputs Draft ACC884 providing a summary of clinical history Clause 5.10.6 Page 13 of 39 Concussion Service Operational Guidelines It is important that the supplier collect all information about the client that may be relevant to their rehabilitation and recovery. The review of clinical notes by the medical specialist and the clinical neuropsychologist is at the cost of the supplier and is covered within the overhead component of all the service items. The specialists do not need to attend an actual meeting, although this is considered best practice. The information collected should include - GP clinical notes including pre-injury brain injuries and health issues (up to five year if relevant). Specifically pre-injury health issues such as depression, mental illness etc. This information can be provided to the specialists and will help in their diagnosis. - ED clinical notes if the client was diagnosed at the Emergency Department - Work or education information to help assess the cognitive demands that have been and could be on the client throughout the recovery - Family composition and responsibilities to help assess any stressors that may hinder recover and also where ACC may need to provide supports - Social background to identify any underlying social issues that may hinder recovery The supplier’s interdisciplinary team will develop a rehabilitation plan that describes client’s goals (expressed as SMART goals) and outlines the therapy required to meet those goals. The ACC case owner and the supplier will finalise and agree service composition and timeliness. The plan may be amended as additional information becomes available. Diagnosis A referral may be sent to a supplier with the clinical diagnosis accepted or still in question. Where the diagnosis is accepted the supplier can progress immediately to investigation, assessment and therapy. If the diagnosis is still in question then the case owner will direct the supplier to confirm the diagnosis. The medical assessment should take a neutral point of view until the appropriate tests and investigations have been taken to rule out other causes for the presenting signs and symptoms. Once the TBI diagnosis is confirmed the impact of the TBI should be assessed and advice provided on appropriate therapy and prognosis. Where the client’s diagnosis is not confirmed the suppliers should ensure the client understands that the diagnosis is being investigated and that they may or may not have a brain injury. This is to minimise the likelihood of the client becoming invested in the TBI diagnosis when, in fact, it maybe another injury such as neck strain. Interim advice on managing pain and other systems can be provided as required without the diagnosis. The supplier is responsible for ensuring there is a confirmed diagnosis before therapy services are provided. Triage The Concussion Service has a strong triage focus, and a full interdisciplinary team using all available information will determine the suitability of the service for the client. If the client… the supplier should has recovered and no longer needs the CS exit them from the CS immediately using the June 2015 Page 14 of 39 Concussion Service Operational Guidelines ACC884 to recommend has needs that can be meet within the limitations of CS, either by itself or in conjunction with other services continue in the CS has needs that are greater than can be provided in the CS exit them from the CS as soon as identified using the ACC884 to recommend Risk assessment The risk assessment is a key tool in the communication between the supplier and ACC. It seeks to describe the client within the four main categories - physical, psychological, work, and social. The 1-5 rating system identifies where there is little to no impact on the client’s rehabilitation (1) to where there is a significant impact in the client’s rehabilitation (5). See Appendix 3: Risk assessment matrix. The supplier interviews the client to identify and document their physical (including the current injury), psychological, work, and social history. This helps identify any barriers to a prompt and sustainable recovery. The risk assessment is based on all available information. If the supplier believes that the accuracy of the risk assessment is compromised by a lack of disclosure on the client’s part they may, with the client’s approval, contact the client’s family, friends, and employer and ask relevant questions. The supplier must take care to maintain client confidentiality. If risks cannot be identified due to non-disclosure then the assessment will be at the less complex rating (1-2). The request for services will reflect this assessment. The supplier should explain to the client that the amount of service available is based on the information they give. Note: While a supplier may choose to have this service provided by a doctor, psychologist or neuropsychologist, the risk assessment will only be paid at the contract TBI21 allied health rate as it is not a clinical assessment. The risk assessment is an important part of the triage process and can assist in determine whether the client’s needs can be met within Concussion Service limits. Assessment of Therapy Needs The client’s needs should be assessed throughout the rehabilitation. All clinical assessments will be completed by professionals operating within their scope of practice and within the interdisciplinary team. The clinical records maintained should meet or exceed the expectations of the professional bodies. For guidance on what to include in the Clinical Neuropsychologist see Appendix 4.If you have any questions please see ACC’s National Psychology Advisor. Rehabilitation Planning The interdisciplinary team will develop specific, measurable, achievable, realistic and timeframe goals with the client. These goals will consider the optimum recovery of the client. The supplier should either provide a copy of the rehabilitation plan to ACC or summarise the plan in the June 2015 Page 15 of 39 Concussion Service Operational Guidelines ACC884 Concussion Service Client Summary. Education The education given to the client and their family/whānau should be clear and easily understood. Where the diagnosis was not confirmed then the supplier will limit the education content to dealing with the symptoms. Once the diagnosis is confirmed as a mild or moderate TBI then education on TBI can be provided. It must cover, but not be limited to, the following items: Item Details Symptoms describe the symptoms describe the recovery journey describe the treatments that will target the individual symptoms cover lifestyle responses and dealing with stress rehabilitation response how it’s different for everyone self-management help from family/whānau and friends supplier support via an interdisciplinary team getting back to normal functioning – having realistic expectations returning to work if appropriate structure of the brain mechanism of injury acute response other ACC services available working with the case owner working with the employer Rehabilitation process Brain injury Other support (where appropriate) The supplier should explain the partnership between the supplier and the ACC case owner in the client’s rehabilitation. Notification The supplier will keep in contact with the case owner throughout the rehabilitation programme and will notify ACC formally using the ACC884 Concussion Service Client Summary form when the rehabilitation plan has been agreed by the interdisciplinary team the rehabilitation is complete Therapy In line with rehabilitation best practice the client’s achievements and rehabilitation needs will be continually assessed to ensure the service is tailored to the client. Therapy services will be provided with specific outcomes in mind and no unnecessary therapy will be provided. Where it becomes clear that the client will need more services than those available in the Concussion Service the supplier will notify ACC immediately. June 2015 Page 16 of 39 Concussion Service Operational Guidelines Key worker The supplier will allocate a key worker for every accepted case. The key worker is responsible for ensuring the coordination between the interdisciplinary team maintaining contact with the client to remind them of appointments and assist in identifying their needs maintaining contact with ACC as agreed ensuring the clinical notes are kept up to date and are at a high standard Interdisciplinary Teams The supplier must have an interdisciplinary team (IDT) fully qualified in their profession with a minimum of two (full time) years’ experience in acquired or traumatic brain injury. The IDT is fully engaged throughout the service to assist in the rehabilitation planning. The IDT will meet on a regular and scheduled basis to discuss the client’s assessment and treatment rehabilitation needs. Notes of the meeting/s will be taken by the key worker who will summarise the individual clinical opinions. The notes will be kept in the client’s notes. The supplier’s team must include: medical specialists with qualifications in neurology or internal medicine with a particular focus in brain injury clinical neuropsychologists occupational therapists The supplier’s team of may also include: physiotherapists registered nurses, preferably with a rehabilitation speciality general practitioners speech language therapists social workers The supplier may refer the client to clinical specialists outside of the interdisciplinary team, on approval from the case owner, to obtain further advice on the client’s specific rehabilitation needs. This will be funded within the maximum funding limited of the Concussion Service on a cost recovery basis. In addition to the supplier’s interdisciplinary team, they must have access to: optometrists alcohol and drug addiction counsellors vocational counsellors anger management services driving assessment services cultural advisors, or services for Māori and Pacific Islanders and other ethnic groups if appropriate, which may include interpreting services consumer advocacy and support services. June 2015 Page 17 of 39 Concussion Service Operational Guidelines Clinical reporting Detailed clinical reporting is not purchased separately in this service but all suppliers are expected to maintain a high standard of clinical notes to evidence all therapies and recommendations. Those notes should be available on request. The supplier is responsible for achieving the rehabilitation outcome and ensuring the client’s healthcare suppliers have enough information to coordinate the client’s care. ACC requires sufficient summary information to support good decision-making and good communication between the supplier and the case owner. If a client does not achieve the expected rehabilitation outcome the supplier must provide ACC with a copy of the full clinical notes with the ACC884. ACC will then use this information to support the on-going planning of the client’s rehabilitation. Use of time The supplier will outline a treatment plan on the ACC884. The plan will be based on current best practice and will recommend the types of services and number of hours required. The supplier can determine how that time is to be used. Service Administration Service location ACC prefers suppliers to provide services in a location that best meets the rehabilitation needs of the client within current best practice guidelines. This may be: the client’s home, workplace, or other appropriate community location the supplier’s facility. Suppliers indicate the territorial authority (TA) areas they are available to provide services in. It is expected that any travel costs claimed will be within each of those TA areas and not between TA areas. In special circumstances the supplier may approach ACC to discuss other travel arrangements. Where the Case owner approves a special arrangement the appropriate travel codes available within the service can be used. Maximum duration While the maximum duration for services is 12 months from the date of the referral to the last treatment date, it is expected that suppliers will work to ensure the client achieves the service objectives within 16 weeks, as clients with more complex needs should not be in the Concussion Service. It’s expected that the supplier will be available for the client as needed over the 12 month period. The supplier should not retain therapy hours to provide a follow-up service as therapy hours are for face-to-face therapy. Client follow-up via phone is considered part of the overhead component of the fees paid. June 2015 Page 18 of 39 Concussion Service Operational Guidelines ACC will monitor client duration based on the length of time between the first date of service to the last date of service of services invoiced for. Service duration will be discussed regularly as part of the dialogue between supplier and case owner. Timeframes The Concussion Service adapts to the needs of the client so there may be situations where the timeframes outlined in the service specification are not appropriate. The supplier is responsible for ensuring that timeframes are discussed and agreed. Section 6 of the ACC884 should record a brief description of the client, their recovery needs and rehabilitation plan. Alternatively a separate rehabilitation plan can be included. The plan should outline expected timeframes for reviews and outcomes such as return to work etc. Maximum funding limit The Concussion Service has a maximum funding limit of $3000, excluding Goods and Services Tax, travel costs and the single payment for non-attendance by the client (Did-Not-Attend fee). ACC will approve services up to that limit based on the client’s diagnosis, clinical and risk assessments completed by the supplier. The risk assessment identifies factors that may affect the client’s ability to recover. For treatment within the Concussion Service to be approved: services must be requested on the ACC884 Concussion Service Client Summary form services must be provided within the maximum funding limit of $3000 The supplier is responsible for ensuring that the maximum funding limit is not exceeded. Should the supplier exceed the maximum funding limit, ACC may choose to recover the overpayment. The supplier and ACC determine the best service provision together. If the supplier and ACC do not agree, ACC is responsible for the final decision and for the client’s rehabilitation outcome. Purchase orders The supplier must hold a purchase order that approves the specific service items. The supplier may provide the services up to the approved maximum in the order determined by the interdisciplinary team and based on the identified clinical need. To provide services differently than those specified on the purchase order prior approval must be sought from ACC to amend the purchase order. ACC is not liable to pay for services not specified on the purchase order. Completing or extending the service After the investigation and planning the ACC884 Concussion Service Client Summary form must be submitted within: 2 working days, when further treatment service needs are requested. The 2-day requirement recognises that both the supplier and ACC want to respond promptly to ensure the client’s access to rehabilitation is not restricted. If this response time is not required the supplier can indicate a more appropriate timeframe on the form or in discussion with the case owner. 5 working days, when all services are complete, no further services are required and the client is exiting the Concussion Service. The 5-day requirement recognises that the client is no longer in need of services and therefore, while a timely response is required, there is no urgency. June 2015 Page 19 of 39 Concussion Service Operational Guidelines The supplier can request further services at any time by submitting an updated ACC884 to the ACC case owner. The case owner will use the same assessment parameters throughout. If further services are requested the ACC case owner will review the case, make a determination and, if approved, forward the purchase order within 2 working days. If the continuance is not approved, they will send decline letters to the client and the supplier. The supplier is not able to trade one service item for another. If the client’s service needs have changed, the supplier should contact ACC with an amended ACC884 Concussion Service Client Summary form and negotiate an amendment of the purchase order. Other ACC services The supplier may recommend that the client is given access to other ACC services, such as vocational services, when they believe it will improve the client’s recovery. The case owner is responsible for reviewing the recommendations and deciding if the client is entitled to the services recommended. The supplier will be notified accordingly. When the supplier believes the client needs more services than are available in the Concussion Service they must recommend that the client exit the Concussion Service. The supplier can then recommend that other services, such as neuropsychology assessment or psychological services, be considered by ACC. ACC may request clinical notes Suppliers will provide any clinical notes within 5 working days when requested by ACC, as there will be some situations where the summary information provided in the ACC884 will be insufficient. Suppliers are expected to have their client’s clinical notes maintained to a high standard, detailing the client’s status, rehabilitation needs, and all treatments provided to date. Client non-attendance Clients who keep their appointments generally take less time to recover and achieve better recovery outcomes than those who do not. ACC will pay one non-attendance (DNA) fee per client, no matter how many times they failed to attend an appointment. The service item code for nonattendance is TBIDNA.. The Concussion Service purchase order is updated for a single DNA fee by the case owner when the supplier: sends the case owner an ACC885 Concussion Service - Did-Not-Attend report within 1 working day of the missed appointment and explains why the client did not attend, and has made all reasonable efforts to remind the client of the appointment, such as an appointment card, a reminder letter, a phone call the day before and finally a text message on the day to the client’s and a contact person’s mobile phone. If the above criteria are met ACC will confirm funding within 2 working days of receiving the form. Invoicing the client for non-attendance ACC plays no part in scheduling appointments. Therefore after the first incidence of nonattendance where ACC has already paid a non-attendance fee, the supplier may choose to invoice the client directly where the client continues to not attend appointments. June 2015 Page 20 of 39 Concussion Service Operational Guidelines The supplier should alert the client and their supporting family and whānau both verbally and in writing at the start of the service about the possibility of being charged for non-attendance. ACC expects that the supplier will: not charge more than the agreed ACC fee that would have been payable take into consideration the client’s financial situation. Service exit due to non-attendance The supplier must notify ACC on each occasion of non-attendance. If the DNA fee is not being paid, notification can be by phone or email. If clients repeatedly do not attend appointments they can be exited from the service. This may result in all services and entitlements ceasing, including weekly compensation payments. Client exit A client exits the service when they have achieved the identified outcomes that enable them to return to work or school, and/or normal daily living. The client is considered to be discharged six weeks after the last service in the Concussion Service. Note: If the client has not achieved these outcomes within the specified timeframe the supplier must make a full comment on the ACC884 Concussion Service Client Summary form and record whether this is for non-compliance or a non-injury related factor, e.g. mental health issues. Post-service client support On going support will be provided to the client throughout the rehabilitation programme and the supplier will act as a point of contact for the 12 months from the date the referral was received. The supplier will contact ACC and refer the client to their ACC case owner if the client reports new symptoms. Not included in the service The following services are not included under Concussion Services: transporting the client to and from the clinic transport from the supplier’s place of residence to the base of operation transport from the base of operation to another base of operation inpatient services for TBI elective surgical treatment arising out of any initial assessment social rehabilitation assessments vocational rehabilitation services radiological and other clinical investigations, for example: - computerised tomography (CT) - magnetic resonance imaging (MRI) - electro-encephalogram (EEG) sleep studies. June 2015 Page 21 of 39 Concussion Service Operational Guidelines Quality Management Supplier approval process ACC reserves the right to verify that individually service providers meet the qualifications and experience outlined in the Concussion Service contract. The supplier is required to submit a copy of the interdisciplinary team’s current annual practicing certificate a full curriculum vitae and, if required, evidence of educational qualifications. ACC will review the documentation and advise the supplier of their decision about the supplier via letter and email, within seven days. Where the supplier intends to provide specialist paediatric rehabilitation (16 years and under) all service suppliers must have at least two years experience providing brain injury therapy services to this age group. On application, or any time thereafter, the supplier should notify ACC of their ability to provide paediatric services to ensure ACC can refer appropriately. The supplier will notify ACC immediately regarding any changes in their ability to provide services. Additional suppliers Services are intended to be provided on the basis of one provider to one client (family included). Should a supplier decide that two fully qualified and experienced providers will consult and treat the client at the same time, ACC would expect to be consulted in order to confirm the clinical efficacy of the treatment programme and ensure that sufficient hours have been allocated. If ACC does not approve, the supplier may still choose to have two professionals per contact hour but ACC will only pay for one supplier. Trainee health professionals Health professionals who do not have the required experience in the rehabilitation of clients with brain injuries (traumatic or acquired) may gain that experience with the contracted supplier only on written approval of ACC and with agreement of the client. Qualified Trainees Where the trainee is qualified in their chosen profession but does not have the required brain injury experience to operate independently they can gain that experience by Participating in learning opportunities provided by the experienced supplier that includes o An introduction to the operation of the Concussion Service o Case studies of clients with mild and moderate TBI o Key readings about the impact, rehabilitation and recovery of traumatic brain injury Undertaking extra study about traumatic brain injury considered appropriate by their clinical supervisor Providing professional services under the supervision of a fully qualified supplier who reviews their work within a collegial relationship and who is competent to train and supervise others. Their work can be invoiced as appropriate within the Concussion Service. Unqualified Trainees June 2015 Page 22 of 39 Concussion Service Operational Guidelines Where the trainee is unqualified and in a formal university training programme the supplier can provide clinical experience opportunities where they consider appropriate. The trainee cannot provide services alone and must be under the direct supervision of a fully qualified and approved supplier. The trainee’s time cannot be invoiced for. The supervising supplier remains responsible for ensuring client safety and for providing quality services. Annual targets and best practice Annual targets will be based on results for the previous year. In the first year of operation the service will have nominated targets. The targets help understand best practice service provision. Annual targets are set with an expectation that the majority of the clients will recover and the supplier will achieve the required outcome. They also recognise that some clients may not experience a full recovery but this does not automatically mean that the supplier has failed. Overall, ACC and suppliers will identify and improve best practice by monitoring performance through the submission and analysis of client data. ACC will issue a report at least annually providing national averages that will show a comparison of supplier performance. Suppliers with the best outcomes at the lowest cost will be studied to identify their clinical best practice. This information will be shared so other suppliers can improve their practice. Quarterly service monitoring Measuring the overall success of the service is done quarterly via a reporting template. Each supplier is required to submit data on all Concussion Service clients who were discharged from the service in the previous three months. This will form the basis of ACC’s monitoring and reporting for this service as the outcome measures. Once the information has been compiled, data will be extracted from ACC’s systems, in conjunction with the supplier’s data, analysed and reported on. When sufficient data has been collected ACC will produce reports that will be available to both internal (named) and external (anonymous) parties. The following table describes the reporting periods and due dates. Period start Period finish Submitted by 1 July 30 September 31 October 1 October 31 December 31 January 1 January 31 March 30 April 1 April 30 June 31 July Summarised by ACC will produce summarised reports when the data is sufficient for robust analysis. Completing the quarterly reporting The quarterly report is completed using information from clinical notes. The report is completed mostly using pre-selected drop down fields. This ensures that the information is categorised to allow better analysis. The supplier provides information that is not easily available to ACC such as risk assessment, pre-injury employment and the client’s employment and recovery status at exit. Once all the spreadsheets have been collated payment data is extracted from ACC’s systems. Analysis and reporting June 2015 Page 23 of 39 Concussion Service Operational Guidelines ACC’s analysis of performance will focus on: average cost per service excluding travel and DNA service length service outcomes in relation to client complexity service inputs in relation to client complexity client recovery client exits for more comprehensive services including ‘big brother’ services any other information ACC considers relevant. Client satisfaction survey The supplier will survey their clients and submit the responses annually as an independent report. The customer satisfaction survey is an opportunity for clients to provide their views on the service they received. The survey must include An opportunity for the client to indicate their overall satisfaction with the supplier, using the following question: Overall thinking of the service you received from <Supplier Name> how satisfied are you? 1. Completely satisfied 2. Mostly satisfied 3. Neither satisfied nor dissatisfied 4. Mostly dissatisfied 5. Completely dissatisfied. An opportunity for the client to comment on their ability to participate fully any barriers to their recover. could include any topics about service or quality that would allow opportunities for improvement Supplier outcome results The table below describes the Supplier/Suppliers Outcome Result fields in the reporting template. Status Description Achieved - Exit The client has or will return to the same functional level as prior to the injury within six weeks of the last Concussion Service date. The client will be no longer requiring any support services from ACC. This can include a client who has fully recovered but no longer has a job to go to so long as they are no longer receiving ACC support, ie: Partial Achieved June 2015 no weekly compensation no rehabilitation services including vocational service The client no longer needs CSS but continues with other ACC supports. This can include a client who has fully recovered but no longer has a job to go to Page 24 of 39 Concussion Service Operational Guidelines Status Description so long as they are continuing to receive ACC support at the time the outcome result form is submitted Not Achieved The client has been triaged out of CSS as too complex Not Achieved The client has not returned to pre-injury function and continues to require services or supports that are more than those provided in the Concussion Service Not Achieved DNA The client either did not participate or did not complete the rehabilitation programme Unknown No therapy provided as ACC did not approve. ACC may also assess the supplier’s performance by using ACC’s payment data. The key point of measure would be the client’s utilisation of ACC’s supports six weeks after the last service within the concussion service. If the client is no longer receiving any services the client is considered to be recovered. Invoicing for travel and services Invoicing for travel The service item codes for travel are TBITT5, TBITT1, and TBITD10 depending on the type of fee. The codes are used throughout the service. If the services are provided in a place other than the supplier’s facility and the supplier needs to travel to the client, travel should be managed to maximise coverage and service time and minimise the distance travelled. Territorial Local Authorities (TLA) During the application process suppliers indicate the TLAs they can provide services in. The expectation is that the supplier has staff available in every area applied for. Therefore the suppliers will not invoice ACC for travel where the travel is between one TLA and another or across multiple TLAs unless approved by ACC. Maximise coverage All attempts should be made to ensure that the supplier is fully occupied throughout the day of travel, therefore, multiple appointments should be made and the maximum number of clients scheduled. Service time The scheduled service time will be appropriate to clinical need and best practice and will only be as long as required. If the time with the client is less than required the supplier should fill in the time up to the scheduled time with client-related activities such as updating client notes, phone calls etc. Distance travelled Appointments will be arranged to ensure the shortest distance between clients, thereby minimising the time and distance travelled. The supplier cannot claim travel time or distance when a supplier June 2015 Page 25 of 39 Concussion Service Operational Guidelines travels from one base of operation to another or from their private residence to the base of operation. ûTravel Not Covered Home or Base Base üTravel Covered Client Location No Travel Clinic Based Service Travel distance TBID10 ACC expects that suppliers and their staff work to minimise travel costs. Travel from a base of operation should be for services to a number of clients. As represented in this loop ü rather than this star û 2 2 25 kms 18 kms 26 kms 26 kms 3 3 25 kms 1 1 20 kms 15 kms 20 kms 18 kms 20 kms Base Base 4 4 28 kms 18 kms In the case of the loop the supplier would recognise a single incidence of 20km, whereas the star would recognise four incidences of 20km. In many instances clients may not all be ACC clients. Allocation of travel costs between the ACC and non ACC clients should be done in a fair and reasonable way that is reflective of the true costs to the funders. This example assumes one of the clients is not being funded by ACC. ü Total Travel (km) Client 1 – Other Tot. Incl Return Travel (km) 27 ACC Clients (km) Less 20 km deduction Invoiced 20 Return Travel (km) 7 Client 2 – ACC 18 7 25 25 7 18 Client 3 – ACC 25 7 32 32 7 25 Client 4 – ACC 15 7 22 22 6 16 Return Travel Total km 28 106 28 106 79 20 59 June 2015 Page 26 of 39 Concussion Service Operational Guidelines û Total Travel (km) Return Travel (km) Total Travel Client 1 – Other 20 20 40 Client 2 – ACC 26 26 Client 3 – ACC 25 Client 4 – ACC Total ACC Clients (km) Less 20 km deduction Invoiced to ACC 52 52 20 32 25 50 50 20 30 18 18 36 36 20 16 89 89 178 138 60 78 Travel time TBITT5 If it takes 15 minutes to travel the first 20km and the overall time spent travelling for the day is 140 minutes, then the supplier can invoice for 125 minutes of travel time if all the travel time relates to ACC clients. Invoicing an hourly rate The invoice should present the time in hours and minutes. Each separate service should be listed by service date. Information Example Client name John Smith Client number 123456789 Purchase order number 1234567 Service date DD/MM/YY Service code TBI21 Time/ Quantity 1 hour 15 mins Amount claimed $133.85 (GST Exc) Service date DD/MM/YY Service code TBI22 Time/ Quantity 30 mins Amount claimed $53.54 (GST Exc) Total amount of invoice $187.39 GST $28.10 Total $215.50 June 2015 Minutes 5 10 15 20 25 30 35 40 45 50 55 60 % 8.3 16.7 25.0 33.3 41.7 50.0 58.3 66.7 75.0 83.3 91.7 100.0 Divide the hourly rate with the appropriate percentage to calculate the portion of the hourly rate. 1 hour $107.08 15 mins = 25% $ 26.77 Total $133.85 Page 27 of 39 Concussion Service Operational Guidelines APPENDICES Appendix 1: Bio-psycho-social model This model was sourced from The Brain Injury magazine January 2005; 19(1): 39-53 and based on the article called Continuum of care model for managing mild traumatic brain injury in a workers’ compensation context: a description of the model and its development by Jeremy M. Rose of Millard Health, Edmonton, Alberta Canada. Its source reference was the World Health Organisation. The following extract from that paper describes the bio-psycho-social model: “The model is not exhaustive but represents some of the common variables thought to influence outcomes following mild Traumatic Brain Injury (TBI). The model is broken down into pre-, periand post-injury variables. Four key points are: recovery following mild TBI can be influenced by a complex interaction of a variety of variables some people appear to be at risk for developing more chronic post-concussion symptoms after mild TBI post-concussion-type symptoms can potentially develop in the absence of any permanent structural damage to the brain following mild TBI differential diagnoses must be assessed in order to provide appropriate treatment. “In relation to interventions following a mild TBI, the bio-psycho-social model highlighted the need to: assess risk factors for a protracted recovery educate the injured worker and his/her support system (eg family) in order to counter any tendency to catastrophize about symptoms or misattribute normally occurring symptoms (such as memory slips) to the head injury assess for differential diagnoses address co-morbid physical injuries develop and implement a treatment and case management plan before the symptoms become chronic.” The paper presented the WCB Continuum of Care model developed by Millard Health. ACC’s model, which is based on the WCB model, is presented Appendix 2. ACC recognises the bio-psycho-social impacts and requires suppliers within this contract to identify and assess the degree of risk to recovery using risk assessment matrix in Appendix 3. June 2015 Page 28 of 39 Concussion Service Operational Guidelines June 2015 Page 29 of 39 Concussion Service Operational Guidelines Appendix 2: Continuum of care model This continuum of care model for concussion rehabilitation management is based on the model developed by the Workers Compensation Board of Alberta, Canada. The model recognises that all clients’ rehabilitation needs will vary significantly, even for similar accidents, therefore: set protocols cannot address the needs of every client consistently, and services must be able to adapt to the needs of the individual. The Concussion Service was designed to enable the supplier to, as soon as possible: identify the client’s needs, and develop a rehabilitation programme that will deliver as rapid and full a recovery as possible. The diagram below is a representative example of the Concussion Service in action and the approximate timeline indicates that treatments do not need to be sequential. Instead suppliers can choose to give treatment therapies when it best meets the needs of the client. Day 15 Week 3 4 5 6 7 8 9 10 11 12 13 14 15 Treatment Phase Assessment Phase Natural Healthing Investigation Planning 16 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52 OSA Med Spec IDT Input Med Spec Assessment MSC Clin Psych IDT Input Clin Psych Screen CPC AH IDT Input Allied Health Assessments AHT MSC CPC AHT CPC AHT CPC AHT AHT CPC AHT CPC AHT AHT Maintain / Obtain Employment Investigation, Diagnosis, Risk Assessment, Assessment and Rehabilitation Planning, Education AHT MSC Medical Specialist Consultation OSA Other Specialist Assessment CPC Clinical Psychologist Consultation Allied Health Therapy The rehabilitation time for each client will vary and only a small percentage of clients are likely to need all the service items shown. Many will require just the investigation and planning, whereas others may need a combination of services. June 2015 Page 30 of 38 Time & Cost Limited Services Day 1 – 10 Concussion Service Operational Guidelines Appendix 3: Risk assessment matrix The purpose of the risk assessment is to measure the biopsychosocial factors that may impact on the client’s rehabilitation outcome and help to determine the amount and type of services needed for rehabilitation. The risk assessment is not a clinical report and can only be used as an indicator of risk to the rehabilitation outcome. It is not be used to determine cover or entitlement to services. There are four areas of client rehabilitation risk: Physical Psychological Work (employment) Life and social. The highest rating from each of the four risk assessments will be recorded on the ACC884 Concussion Service Client Summary form for the case owner’s consideration. Low Low – Medium Medium Medium – High High Physical 1 2 3 4 5 Psychological 1 2 3 4 5 Work 1 2 3 4 5 Life and Social 1 2 3 4 5 Illustration of ACC884 section 8: 8. Risk assessment Please indicate the level of risk that may impact the client’s recovery: 1 = Low, 2 = Low/Medium, 3 = Medium, 4 = Medium/High, 5 = High. Risk Level Briefly describe the impacts on rehabilitation (attach clinical notes for details) Physical Psychologica l Employment Life - social June 2015 Page 31 of 38 Concussion Service Operational Guidelines Note: These pages are sized A3 and may not be printable Areas / Flags Meaning or interpretation of risk levels 1 - Low Risk The client does not appear to have obvious or identifiable risk to their recovery. 2 - Low / Medium Risk The client appears to have some identifiable risk factors that are not so severe as to cause significant risk to their recovery. 3 - Medium Risk The client appears to have some identifiable risk factors but they are either: not so severe as to cause significant risk to their recovery, or they can be managed within the services requested. 4 - Medium / High Risk 5 - High Risk The client appears to have identifiable risk factors that are likely to impact on their recovery that may or may not be manageable within the services requested. The client appears to have significant risk factors that will impact on their recovery. The options are to access a more complete range of services in this service in order to gain full recovery, or to refer the client to other ACC services. Physical The client has (and/or): The client has (and/or): The client has (and/or): The client has (and/or): The client has (and/or): Frequency of TBI injuries never had a previous head injury had a mild TBI over 5 years previously had a mild TBI 2–5 years ago Severity of TBI injury had a knock to the head, eg fallen onto hard surface Presence and severity of other physical injuries received a high speed impact such as a fall from a moving horse, bike, cycle or MVA no other physical injuries had repeated knocks to the head during contact sports in the last 12 months, or received a high speed impact such as a fall from a moving horse, bike, cycle or MVA had a moderate TBI within the last 12 months or a severe TBI within the last 10 years had a minor knock to the head, eg fall forward with an injury to face or side of head no reported loss of consciousness or PTA had several TBIs within the last 2 years Physical disabilities no physical disability or any other health issues received multiple physical injuries that required a long stay in hospital a severe physical disability with high support and/or equipment needs had a minor knock to head, eg hit by cupboard door etc a minor physical injury that did not require any significant medical intervention a minor physical disability or health issues sustained other injuries that required treatment but not hospitalisation and/or a minor physical injury that required some medical intervention moderate physical disability/health issues received moderate physical injuries that required hospitalisation a severe physical disability and has good support/equipment Psychological The client has (and/or): The client has: The client has (and/or): The client has (and/or): The client has (and/or): Pre-injury mental health diagnosis no pre-injury mental health condition said that they do not drink or take drugs severe mental health issue(s) with high support/medication needs Post-injury alteration in mood a mild use of recreational drugs or alcohol a moderate use of recreational drugs or alcohol significant mental health issue(s) that are under control with good support and medication diagnosed mental health needs that may affect their rehabilitation diagnosed mild mental health issue(s) or has had diagnosed mental health needs that are now fully resolved full dependency on hardcore drugs or alcohol a mild alteration in mood post-injury, eg anxiety, tearfulness, irritability, frustration mild alteration in mood post-injury, eg anxiety, tearfulness, irritability, frustration a high use of recreational drugs or alcohol a moderate alteration in mood postinjury, eg anxiety, tearfulness, irritability, frustration a severe alteration in mood post-injury, eg suicidal, anger, anxiety, depression self/family/friends who are placing unrealistic expectations on them to function at the pre-injury level but have been receptive to information to change self/family/friends who are placing very unrealistic expectations on them to function at the pre-injury level and are not receptive to information to change experienced several aspects of the accident or subsequent treatment as traumatic in nature and is highly anxious, eg MVA with fatality, unprovoked assault, assault by a family member Reaction of family Personality and coping skills Beliefs about the injury Life stressors June 2015 reported no alteration in mood postinjury supportive family and friends who display a positive attitude, have realistic expectations and a good understanding of the impact of the injury and the recovery pathway said that the accident was not traumatic in any way a positive personality with good coping skills no stressors that will impact on their recovery family and friends whose expectations are reasonably good but have some minor anxiety regarding the effects of TBI and the recovery pathway limited support from family and/or friends due to their commitments, eg they work full time good coping skills but there are some minor stressors that may impact on their rehabilitation family and friends whose expectations are somewhat unreasonable and have some minor anxiety regarding the effects of TBI and the recovery pathway little or no identified support to assist them in their rehabilitation experienced several aspects of the accident or subsequent treatment as traumatic in nature experienced several aspects of the accident or subsequent treatment as traumatic in nature and is anxious few or inadequate coping skills and does not appear to cope with the injury or requirements for rehabilitation, and will need support a highly dependant personality with no real coping skills and a very poor ability to plan for the resolution of problems or barriers has moderate to high life stressors that are impacting on their rehabilitation significant family and social stress that is likely to impact on their recovery moderate coping skills and there are some stressors that may impact on their rehabilitation Page 32 of 39 Concussion Service Operational Guidelines Areas / Flags Meaning or interpretation of risk levels 1 - Low Risk The client does not appear to have obvious or identifiable risk to their recovery. 2 - Low / Medium Risk The client appears to have some identifiable risk factors that are not so severe as to cause significant risk to their recovery. 3 - Medium Risk The client appears to have some identifiable risk factors but they are either: not so severe as to cause significant risk to their recovery, or they can be managed within the services requested. 4 - Medium / High Risk 5 - High Risk The client appears to have identifiable risk factors that are likely to impact on their recovery that may or may not be manageable within the services requested. The client appears to have significant risk factors that will impact on their recovery. The options are to either access a more complete range of services in this service to gain full recovery, or to refer the client to other ACC services. Work The client (and/or): The client (and/or): The client (and/or): The client (and/or): The client (and/or): Work demands is unable to work due to the injury enjoys their workplace and is either back at work or is keen to return as soon as they can and believes the workplace achievement requirements are good/fair is anxious about their workplace and is either back at work or is somewhat resistant to return to work. They believe the workplace achievement requirements are realistic normally but will now be challenging is unable to work due to the severity of their injury but is keen to return to work due to the positive work environment and good job satisfaction Workplace perception is managing reduced hours at work with support of employers is maintaining pre-injury work status with low level of stress believes work achievement requirements in the workplace are excessive/unrealistic/unfair is very anxious about their workplace and is resistant to return to work. They believe the workplace requirements will now be too challenging and unfair has severe anxiety about returning to work due to a lack of workplace support. They believe the workplace requirements are unfair tried to return to work but failed and now has severe anxiety around returning to work has no friends in the workplace and people there are unsatisfactory to work with is employed in a job where they are responsive to the needs of others and they have no ability to manage their own workload demands, or where lapses in concentration and memory will put self and others at risk, eg surgeon, pilot etc dislikes the work tasks they do and never achieves job satisfaction has a work organisation that is not interested in participating in the client’s return to work. They believe the client will not be able to return Social support at work Nature of work Job satisfaction Work organisation has a strong network of supportive colleagues in the workplace is employed in a job in which they can manage their own workload demands, or which lapses in concentration and memory will not be risky or dangerous has excellent job satisfaction has a supportive work organisation that is keen to participate in the immediate or gradual return to work is managing pre-injury work hours but is struggling due to symptoms and/or a stressful work situation is OK with their workplace and is either back at work or is unexcited to return to work. They believe the workplace achievement requirements are realistic normally but may now be challenging has a network of colleagues in the workplace is employed in a job where they have some ability to manage their own workload demands, or where lapses in concentration and memory will not be risky or dangerous, eg office worker enjoys the work tasks they do most of the time and has good job satisfaction has a fairly supportive work organisation that will provide opportunity to participate in the immediate or gradual return to work has one or two work colleagues in the workplace. There are a number of people there who are unsatisfactory to work with has one or no work colleagues in the workplace. There are a lot of people there who are unsatisfactory to work with is employed in a job where they have little ability to manage their own workload demands, but where lapses in concentration and memory will not be risky or dangerous, eg teacher, receptionist, student etc is employed in a job where they are responsive to the needs of others and they have no ability to manage their own workload demands, or where lapses in concentration and memory will put self and others at risk, eg machine operator, commercial driver etc sometimes enjoys the work tasks they do and has fair job satisfaction has a work organisation that will provide some opportunity to participate in the immediate or gradual return to work, although they don’t seem overly keen seldom enjoys the work tasks they do and does not often achieve job satisfaction has a work organisation that requires considerable education about TBI if the client is to make a successful graduated return to work Life-Social The client (and/or): The client (and/or): The client (and/or): The client (and/or): The client (and/or): Life stressors has severe financial stress with no readily available options or support Social lives in a stable quiet environment and is managing minimal social roles satisfactorily. has severe financial stress but has readily available options or support for improving their situation has moderate financial stress with no available options or support for improving their situation Financial has moderate financial stress with available options or support for improving their situation has no financial stress and is financially stable lives in a busy but structured household and has minimal social responsibilities. lives in a busy but structured household and has responsibility for extended family/whānau as well as several social responsibilities. lives in a busy unstructured household and has minimal social responsibilities. has responsibility for earning money within a business, which is now failing due to the injury lives in a busy unstructured household and has responsibility for extended family/whānau as well as several social responsibilities. June 2015 Page 33 of 39 Concussion Service Operational Guidelines Appendix 4: Neuropsychological assessment guidelines Adults with mild and moderate TBI Five hours has been allocated for the neuropsychological component of the Concussion Service. As no report is required, other than a summary and recommendations, this can be seen as equivalent to a standard neuropsychological assessment in terms of time allocation. This means that a comprehensive interview should be able to be carried out as well as a reasonable amount of psychometric assessment. This assessment requires more depth than the cognitive screening in the previous Concussion Clinic contract. Information required Qualitative information required Accident history/presenting problems If this information has not accompanied the referral it should be obtained from the GP or hospital and checked to determine the nature of the injuries sustained, the client’s presentation and any investigations and interventions carried out. Personal background and current information Family History and social history Family of origin - parents’ ethnicity and culture, language(s) spoken at home, family makeup, quality of family environment and relationships Client - current living situation, marital status (past and present), current relationship, children from present or past relationships and impact of client problems on family functioning and relationships Social relationships – quality of friendships, sibling relationships and other social support Clients view of self – self-concept, strengths, difficulties, hobbies and interests. Educational History – level of schooling achieved, age on leaving school, qualifications achieved, attendance record, number of changes in schools, problems and successes, relationships with teachers, attitude towards school and any special educational interventions etc. Occupational History – past and present employment, periods of unemployment, satisfaction with past and current jobs, relationship with work colleagues/supervisors, volunteer work etc. Medical History – vision, hearing, illnesses, injuries, hospitalisations, previous history of TBI, drug/alcohol use (current/past), eating habits and sleeping habits etc. Psychological history – current or previous problems/diagnoses, therapy (past/present), drug or alcohol rehabilitation, efficacy of past treatment/therapy etc. Forensic history (if relevant) Behavioural observations in assessment June 2015 Physical appearance and characteristics, ease of establishing and maintaining rapport with client, language style, response to failures and successes, response to encouragement, attention span, distractibility, Page 34 of 39 Concussion Service Operational Guidelines activity level, anxiety level, mood, impulsivity/reflectivity, problem solving strategy, attitude towards the assessment process, attitude toward the examiner, attitude toward self, unusual mannerisms or habits, validity of test results in view of behaviour. Quantitative information required Estimate the client’s… pre-accident level of behavioural, emotional, and cognitive functioning and relate to the qualitative information Assess the client’s… current behavioural and emotional functioning in relation to their significant others effort, using at least one forced choice measure of symptom validity along with embedded measures. It’s important not to identify the symptom validity measures used in the report so as to protect the test materials attention, ie sustained, selective, alternating/divided immediate and working memory rate of information processing learning and memory abilities, ie verbal and visual learning and recall. Test the client’s… Executive functioning Executive functioning is likely to be assessed in more detail when a client has had a moderate rather than mild TBI. Use of everyday measures such as the Behavioural Rating Inventory of Executive Function (BRIEF) Self and Other Versions is recommended, along with formal assessment. When time constraints are present, using the BRIEF rather than formal measures of executive functioning is recommended. Formulation/Summary Pulling all the sources of data together and integrating them into a coherent whole requires: building on the descriptions of the presenting problems summarising the performance on psychometric tests of cognitive abilities combining this information with data from other sources and mapping all this onto the client’s day to day functioning. It’s expected that pre-accident functioning in behavioural, cognitive, emotional and social domains will be taken into account when determining whether and in what ways the TBI has impacted on the client in terms of everyday functioning. Practical recommendations should result from the neuropsychological assessment which will facilitate the rehabilitation of the client. It’s important to identify the range of factors which may be impacting on and influencing a client’s cognitive profile rather than attributing all to TBI. A neuropsychological assessment is not, in itself, diagnostic of TBI. Pain, depression, post-traumatic stress disorder and alcohol/drug abuse can all produce cognitive deficits which are similar to those seen in mild/moderate TBI. What is required is a consideration and analysis of all possible contributing factors and then coming to a reasoned conclusion. June 2015 Page 35 of 39 Concussion Service Operational Guidelines Children/adolescents with mild and moderate TBI Information required Qualitative information required Accident history/presenting problems If this information has not accompanied the referral it should be obtained from the GP or hospital and checked to determine the nature of the injuries sustained, the child’s presentation and any investigations and interventions carried out. Sources of information Information should be gathered from initial interviews with the child and parents. It’s important to also obtain relevant collateral information from teachers and/or rehabilitation workers. Personal background and current information Developmental history relevant prenatal/perinatal history developmental milestones existence of developmental disorders. Family and Social History Family of origin - parents’ ethnicity and culture, language/s spoken at home, family makeup, quality of home environment and family relationships Social relationships – quality of friendships, sibling relationships and other social support. Child’s view of self – self-concept, strengths, difficulties, hobbies and interests. Educational History – level of schooling achieved, academic progress, qualifications achieved, attendance record, number of changes in schools, problems and successes, relationships with teachers, attitude towards school and any special educational/behavioural interventions. Medical History – vision, hearing, illnesses, injuries, hospitalisations, medications, previous history of traumatic brain injuries, cigarette use, drug/alcohol use (current/past), eating habits, sleeping habits. Psychological history – current or previous behavioural/emotional problems/diagnoses, therapy (past/present), efficacy of past treatment/therapy. Forensic history (if relevant) Behavioural observations during assessment and in various settings (school, playground, home) Physical appearance and characteristics, ease of establishing and maintaining rapport with client, language style, response to failures and successes, response to encouragement, attention span, distractibility, activity level, anxiety level, mood, impulsivity/reflectivity, problem solving strategy, attitude towards the assessment process, attitude toward the examiner, attitude toward self, unusual mannerisms or habits, validity of test results in view of behaviour. Quantitative information required Estimate the June 2015 pre-accident level of behavioural, emotional, and cognitive functioning Page 36 of 39 Concussion Service Operational Guidelines child/adolescent’s… and relate to the qualitative information Assess the child/adolescent’s … current behavioural and emotional functioning in relation to their teacher/parents/other children effort, using at least one forced choice measure of symptom validity along with embedded measures. It’s important not to identify the symptom validity measures used in the report so as to protect the test materials attention, ie sustained, selective, alternating/divided immediate and working memory rate of information processing learning and memory abilities, ie verbal and visual learning and recall. Test the child/adolescent’s … Executive Functioning Executive functioning is likely to be assessed in more detail when a client has had a moderate rather than mild TBI. Use of everyday measures such as the Behavioural Rating Inventory of Executive Function (BRIEF) Parent and Teacher Versions is recommended, along with formal assessment. When time constraints are present, using the BRIEF rather than formal measures of executive functioning is recommended. Test interpretation requires an awareness of factors that might impact on the child’s test performance, eg family stressors (separation or other), anxiety and mood issues, distrust, sleep deprivation, lack of engagement. It’s important to identify strengths and weaknesses of the child. Formulation/Summary Pulling all the sources of data together and integrating them into a coherent whole requires: building on the descriptions of the presenting problems summarising the performance on psychometric tests of cognitive abilities combining this information with data from other sources mapping all this onto the child’s day to day functioning. It’s expected that pre-accident functioning in behavioural, academic, cognitive, emotional and social domains and awareness of the child’s developmental stage, ie normal age variations and variability in development, will be taken into account when determining whether and in what ways the TBI has impacted on the child and their family in terms of everyday functioning. Practical recommendations should result from the neuropsychological assessment which will facilitate the rehabilitation of the child/adolescent. General Recommendations It’s important to identify the range of factors which may be impacting on and influencing a child’s cognitive profile rather than attributing all pathology to TBI. A neuropsychological assessment is not, in itself, diagnostic of TBI. Pain, depression, ADHD, in-utero alcohol/drug exposure, can all produce cognitive deficits which are similar to those seen in mild/moderate TBI. What’s required is a consideration and analysis of all possible contributing factors and then coming to a reasoned conclusion. June 2015 Page 37 of 39 Concussion Service Operational Guidelines The child’s strengths and weaknesses need to be highlighted and a discussion held about how parents, teachers and the child can utilise his/her strengths to compensate for identified weaknesses. June 2015 Page 38 of 39