Paradoxical Vocal Cord Dysfunction

Exercise Induced
Paradoxical Vocal Cord Dysfunction
(EI-PVCD)
Dale R. Gregore
M.S., CCC-SLP
Speech Language Pathologist
Clinical Rehabilitation Specialist - Voice
NORMAL Respiration 101
On inhalation, the vocal cords (folds)
ABduct allowing air to flow into the trachea, bronchial tubes, lungs
On exhalation, the vocal folds may close slightly, however should and do remain ABducted
Normal Larynx
Vocal fold
ABDUCTION occurs during respiration
Vocal fold ADDUCTION
Occurs during swallowing, coughing, etc…
Strobe exam
Paradoxical Vocal Fold Movement
(PVFM)
The cord function is
reversed in that the vocal folds ADDuct on inspiration versus
ABduct
Leads to tightness or spasm in the larynx
Inspiratory wheeze evident
Definition of EI-VCD
“Inappropriate closure of the vocal folds upon inspiration resulting in stridor, dyspnea and shortness of breath (SOB) during strenuous activity”
– Matthers-Schmidt, 2001;
Sandage et al, 2004
Pseudonyms
Vocal Cord Dysfunction (VCD)
– Most common term
Munchausen’s Stridor
Emotional Laryngeal Wheezing
Pseudo-asthma
Fictitious Asthma
Episodic Laryngeal Dyskinesia
Patient description of VCD episodes
– “in the top of my throat I see a
McDonalds straw surrounded by darkness. The straw ends in a pool of thick, sticky liquid that is encased by a wall of rubber bands and outside of the rubber bands is air that I can’t access”.
– “The top part of my throat is complete darkness, at the back part of the darkness there are cotton balls. These are holding my fear”.
PVFM Visualized
Anterior portion of the vocal folds are
ADDucted
Only a small area of opening at the
Posterior aspect of the vocal folds
Diamond shaped
‘CHINK’
May be evident on both inhalation and exhalation
Essential Features
Vocal fold adduct (close) during respiration instead of abducting
(opening)
Laryngeal instability while patient is asymptomatic
– Treole,K. et. al. 1999
Episodic respiratory distress
Symptoms
Stridor
Difficulty with inspiratory phase
Throat tightening > bronchial/ chest
Dysphonia during/following an attack
Abrupt onset and resolution
Little or NO response to medical treatment (inhalers, bronchodilators)
Various Etiologies
Laryngo-Pharyngeal Reflux (LPR)
– Food/ liquid/ acid refluxes from the stomach up the esophagus into the pharynx (throat)
– Can spill over and into the larynx
– causes coughing, choking, breathing and voice changes, swelling, irritation,
– Can be SILENT or sensed when it happens
– WATERBRASH
LPR, continued
Clinical characteristics can be observed using videolaryngoscopic or stroboscopic visualization of the larynx
Ideally, diagnosed by a 24hour pH. Probe or EGD
LPR and Athletes
Well documented occurrence in weight lifting
Can be aggravated by bending, pushing/ resisting (tackling, etc…), tight clothing, even drinking water during a game/ meet/ match
Timing of meals before exercise is important
Type of foods/ liquids should be monitored
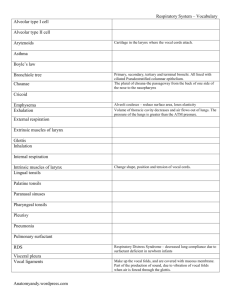
Laryngopharyngeal Reflux:
Clinical Signs
Interarytenoid Edema
Lx Erythema
Vocal Fold Edema
Other potential causes of
Paradoxical Vocal Cord
Dysfunction
Allergic rhinitis or reaction
Conversion disorder
Anxiety
Respiratory-type or druginduced laryngeal dystonia
Etiologies (cont.)
Asthma-associated laryngeal dysfunction
Brainstem dysfunction
CVA or injury
Chronic laryngeal instability, sensitivity & tension
Athlete Profile for EI-VCD
Onset between 11-18
Females have a greater incidence
(generally 3:1)
High achieving
“Type A” personalities
High personal standards and/or social pressures
Intolerant to personal failure
Athlete Profile, cont…
Competitive
Self demanding
Perceives family pressure to achieve a high level of success
“Choke” under pressure
May have recently graduated to higher level of competition within their sport (JV to Varsity: Rep to Travel team; college level sports, etc)
EI-VCD versus Asthma
Recalcitrant to asthma medications i.e. does not respond to
Individuals with “asthma” after long term steroid use might not truly have asthma, but VCD
Individuals with significant anxiety: is it LIVE OR MEMOREX? Which causes which?
Differential Diagnosis of EI-VCD
Includes a detailed Case History
Pulmonary function Studies
Lab Test
ENT/ Pulmonary/ Allergy evaluations
Flexible Laryngoscopy/ videostroboscopy
Speech-language pathology evaluation
Supplemental as needed: Psychological evaluation
Differential Diagnosis of VCD
Team Must Rule Out:
– Mass Obstruction
– Bilateral vocal fold paralysis
– Anaphylactic laryngeal edema
– Extrinsic airway compression
– Foreign body aspiration
– Infectious croup
– Laryngomalacia
– Exercise Induced Asthma/
Asthma
Diagnosis of EI-VCD
Often mistaken for asthma
Diagnosis of EI-PVCD is by
exclusion = when patient fails to respond to asthma or allergy medication, then
VCD is finally considered
EI-VCD and Asthma
Can exist independently
Can also coexist
– Patient may experience LPR which causes Asthma flare-up and then laryngospasm (VCD) from coughing
– May experience chest (asthma) and/or laryngeal (VCD) tightness
EI-PVCD versus
Exercise Induced Asthma
Feature
Female Preponderance
Chest Tightness
Throat Tightness
Stridor
Usual onset of symptoms after beginning exercise (min)
Recovery period (min)
Refractory period
Late-phase response
Response to beta-agonist
PVCM
+
+/-
+
+
<5
5-10
-
-
-
EIA
-
-
-
-
>5-10
15-60
+
+
+
Typical Spirometry Findings for
PVCD
Asymptomatic
– Flow-volume loops are normal
Symptomatic:
– Blunted inspiratory curve
– Inspiratory curves highly varied
– Expiratory portion may be blunted
– Ratio of forced expiratory to inspiratory flow at 50% VC can be greater than 1.0
Inspiratory cut-off, flattening of the inspiratory limb (curve)
NORMAL VCD
Case History Questions
– Do you have more trouble breathing in than out?
– Do you experience throat tightness?
– Do you have a sensation of choking or suffocation?
– Do you have hoarseness?
– Do you make a breathing-in noise
(stridor) when you are having symptoms?
Questions (cont.)
– How soon after exercise starts do your symptoms begin?
– How quickly do symptoms subside?
– Do symptoms recur to the same degree when you resume exercise?
– Do inhaled bronchodilators prevent or abort attacks?
– Do you experience numbness and/or tingling in your hands or feet or around your mouth with attacks
Questions (cont.)
– Do symptoms ever occur during sleep?
– Do you routinely experience nasal symptoms (postnasal drip, nasal congestion, runny nose, sneezing)?
– Do you experience reflux symptoms?
Videostroboscopic Examination
Instrumentation
– Flexible fiberoptic laryngeal endoscope with stroboscopic capability
Observations
– Movement of arytenoids during respiration at rest: Complete closure; Posterior diamond
– Signs of laryngopharyngeal reflux disorder
(LPR)
– Degree of laryngeal instability
Laryngeal Supraglottic
Hyperfunction
arytenoid compression ventricular compression
Limited airway for phonation
VCD appearance on direct examination
Laryngeal
Supraglottic
Hyperfunction
Abnormal ventricular compression during speech
Laryngeal Supraglottic
Hyperfunction
Sphincteric contraction of the supraglottis during speech production
PVCM Visualized
Posterior ‘chink’
Rounded arytenoids, but normal abduction
Diagnostic Features PVFM Asthma
Flow-volume loop Inspiratory cut-off, Reduced expiratory perhaps some expiratory limb only
limb reduction *
Bronchial provocation Negative test
Positive
Laryngoscopic Inspiratory adduction observations
Vocal folds may adduct during of anterior 2/3 of vocal exhalation folds; posterior diamondshaped chink; perhaps medialization of ventricular folds; inspiratory adduction may carry over to expiration
Diagnostic Features PVFM Asthma
Precipitators (triggers) Exercise, extreme Exercise, extreme temperatures, airway temperatures, irritants, emotional airway irritants, stressors emotional stressors, allergens
Number of triggers Usually one Usually multiple
Breathing obstruction Laryngeal area Chest area location
Timing of breathing Stridor on noises inspiration
Wheezing on exhalation
Pattern of dyspneic Sudden onset and More gradual onset event relatively rapid cessation longer recovery period
Almost always Nocturnal awakening Rarely with symptoms
Response to bronchodilators and/or systemic corticosteroids
No response Good response
Acute Management of EI-VCD in the field
Approach to the patient is important
It is generally agreed that patients do not consciously manipulate or control their upper airway obstruction
Acute Management of EI-VCD
During an episode, they usually feel helpless and terrified
Implying that it is “in their head” is incorrect and counterproductive to their recovery
Coach them through, help them out
Be positive
Acute Management of Attacks
– Offer reassurance and empathy
– Eliminate activity and people from environment
– Prompt for EASY BREATHING
– Elicit controlled ‘Panting’
Relaxed jaw
Tongue on floor of mouth behind bottom teeth
Acute Management in the Game
Visualize WIDE OPEN AIRWAY
6 lane highway with no roadblocks
Air goes in and circles around, goes out
Shoulders relaxed
Standing w/ open chest, hands on hips, or bent over/ hands on knees….which position works best?
Quick Sniff Technique
– Sniff then Blow….talk the athlete through this
– Sniff in with focal emphasis at the tip of the nose
Sniff = ABduction
– Then exhale with pursed lips on
“ssssss”
“shhhhhh”
“ffffffff”
“whhhhhhhh”
= Back pressure respiration
ACUTE treatment, cont…
– Breathing against pressure (hand on abdomen)
Resistance and focus on pressure against / in another body part
– Heliox
Administered by Paramedics or ER MDs
– Sedatives and psychotropic medications
Last resort
Calming effect
Eliminates tension/ constriction
Treatment: Speech Therapy
Patient counseling, education
Respiratory retraining
Focal and whole body relaxation
Phonatory retraining
Monitor reflux Sx or anxiety
Develop / outline a ‘Game Plan’ = practice when asymptomatic; implement at the onset of sx
Therapeutic goals and methods
Goal
– Ability to overcome fear and helplessness
– Reduced tension in- extrinsic laryngeal muscles
– Diversion of attention from larynx
Method
– Mastery of breathing techniques
– Open throat breathing; resonant voice technique
– Diaphragmatic breathing and active exhalation
Therapeutic goals and methods
Goal
– Reduced tension in neck, shoulders and chest
– Ability to use techniques to reduce severity and frequency of attacks
Method
– Movement, stretching, progressive relaxation
– Increase awareness of early warning symptoms;
Rehearse action plan
Speech Therapy
Patient Counseling & Education
– Description of laryngeal events
– Viewing of laryngoscopy tape
– Relate parallels to other stress induced disorders: migraine, irritable colon, muscle tension dysphonia, GEReflux
– Flexible endoscopic biofeedback
– Sensory biofeedback (sEMG)
Speech Therapy
Respiratory training
– Low “diaphragmatic” breathing versus
“high” clavicular thoracic
– Rhythmic respiratory cycles
– Use resistance exhale (draw attention away from larynx and extend exhale)
– Prevention and coping strategies during episodes = Action Plan
Back Pressure Breathing
Nasal Sniff = OPEN cords
Prolonged exhalation /w/, /f/, /sh/,
/s/
Shoulders relaxed
Throat open
Implement when laying, sitting, standing, walking, jogging, running, playing sports, etc
Relaxation Training
Goal
– Teach the patient to relax focal areas then the entire body during an episode of respiratory distress
Methods
– Use progressive relaxation with guided imagery
– Explore the patient’s visual concept of their disorder and alter
ST Duration: The CCHS Approach
2-8 sessions
Average 4 sessions
Followed by clinical observation during sport/ game
Followup phone / email contact: tell me how it is going?
Re-evaluation as necessary, if symptoms reoccur (rarely)
CASE DISCUSSION
14 year old female
Sports: field hockey, soccer
Travel soccer U-17 team/ midfiled
Initial symptoms: ‘throat closes’ ~5 minutes in to game; hand on throat; signals coach; pulled from game; 20 minute recovery: lying on sideline
Therapy Focus and Outcome
5 sessions
Breathing 101
Training from static to active movement/ running
Full coaching then observation of strategy implemetation in therapy and during game
Outcome: (-) sx during mile run; cool down routine implemented; 20-30 minute game play/ no EI-VCD w/ ‘game plan’
Case Discussion #2
14 year old female
Sports: cross country; basketball
Initial Symptoms: ‘throat closed’ during CC trials; had to ‘drop out’
Secondary Symptoms: inspiratory stridor when wearing mouth guard/ basketball; felt ‘faint’
Therapy Focus and Outcome
5 sessions
Goals: establish ‘low’ AD breathing/ eliminate shoulder elevation and CT respiration pattern; train in back pressure breathing w/ and w/out mouthguard during activities of progressive effort including walk; jog; stairs, treadmill; suicide drills;
BB drills; sprints, etc
Outcome
Successful resolution of PVFM during
20 minute runs and when playing BB
Increased awareness of AD versus
CT respiration
Habituated alternate use of sniff/ pant – blow, etc.
Increased perceived ‘control’ over breathing and performance
Spring Sport pending: soccer
REFERENCES
Brugman, S. M., & Newman, K. (1993). Vocal cord dysfunction. Medical/Scientific Update. 11. 5. 1-5.
Christopher, K. L., WoodII, R. P., Eckert, R. C., Blager,
F. B., Raney, R. A., & Souhrada, J. F. (1983). Vocalcord dysfunction presenting as asthma. The New England
Journal of Medicine. 308. 1556-1570.
Gavin, L. A., Wamboldt, M., Brugman, S., Roesler, T.
A., & Wamboldt, F. (1998). Psychological and family characteristics of adolescents with vocal cord dysfunction.
Journal of Asthma. 35. 409-417.
Martin, R. J., Blager, F. B., Gay, M. L., & WoodII, R. P.
(1987). Paradoxic vocal cord motion in presumed asthmatics. Seminars in Respiratory Medicine. 8. 332-337.
Matthers-Schmidt B.A Paradoxical Vocal Fold Motion: A
Tutorial on a Complex Disorder and the Speech Language
Pathologist’s Role. American Journal of Speech-Language
Pathology 2001; 10:111-25.
Sandage et. al. Paradoxical vocal fold motion in children and adolescents. Lang. Speech Hear. Serv. Sch. 2004: 35
(4) 353-62
Vlahakis NE, Patel AM, Maragos NE, Beck KC.
Diagnosis of Vocal Cord Dysfunction: The Utility of
Spirometry and Plethysmography. Chest 2002; 122: 2246-
2249.
Nastasi, K. J., Howard, D. A., Raby, R. B., Lew, D. B.,
& Blaiss, M. S. (1997). Airway fluoroscopic diagnosis of vocal cord dysfunction syndrome. Annals of Allergy,
Asthma, Immunology. 78. 586-588.
Powell DM, Karanfilov BI, Beechler KB, Treole K,
Trudeau MD, Forrest L. Paradoxical vocal cord dysfunction in Juveniles.Arch. Otolaryngol Head Neck Surg.
2000 Jan; 126 (1): 29-34
Morris MJ, Deal LE, Bean DR, Grbach VX, Morgan JA.
Vocal Cord Dysfunction in Patients with Exertional Dyspnea.
Chest 1999; 116: 1676-1682.