Chapter 38: Environmental Emergencies

Chapter 38
Environmental
Emergencies
National EMS Education
Standard Competencies
Trauma
Integrates assessment findings with principles of epidemiology and pathophysiology to formulate a field impression to implement a comprehensive treatment/disposition plan for an acutely injured patient.
National EMS Education
Standard Competencies
Environmental Emergencies
Recognition and management of
− Submersion incidents
− Temperature-related illness
National EMS Education
Standard Competencies
Environmental Emergencies
Pathophysiology, assessment and management of
− Near drowning
− Temperature-related illness
− Bites and envenomations
National EMS Education
Standard Competencies
Environmental Emergencies
Pathophysiology, assessment and management of
− Dysbarism
• High-altitude
• Diving injuries
− Electrical injury
− Radiation exposure
− High-altitude illness
Introduction
• Environmental emergencies: Medical conditions caused or worsened by weather, terrain, or unique atmospheric conditions at high altitude or underwater
Introduction
• EMS providers may be called to emergencies in:
− Endurance sports events
− Mass gatherings
− Acutely confused older patients
© Martin Pisek/ShutterStock, Inc.
Introduction
• Certain weather conditions affect ability to adapt to environment:
− Wind
− Rain
− Snow
− Temperature extremes
− Humidity
Introduction
• Emergency locations may affect:
− Learning about emergency
− Responding to scene
− Reaching patients in remote settings
Introduction
• Common risk factors predispose people to environmental emergencies.
− Younger and older people —harder to maintain thermoregulation
− Preexisting conditions (diabetes, cardiac disease)
− Dehydration
Homeostasis and Body
Temperature
• Body processes that balance supply and demand of body ’s needs
• Thermoregulation: Thermosensitive neurons in anterior hypothalamus balance heat production and dissipation.
Homeostasis and Body
Temperature
• Body tries to keep temperature of 98.6
° F.
• CBT: Temperature in part of body consisting of heart, lungs, brain, and abdominal viscera
• Starting temperature for:
− Hypothermia —95 ° F
− Heat stroke —104 ° F
Homeostasis and Body
Temperature
• Oral temperature used for measurement in general medical conditions
− Can vary dramatically from CBT if patient is:
• Breathing by mouth
• Drinking hot or cold liquids
• Axillary temperature (armpit) about 1 ° F cooler
• Rectal temperature about 1 ° F hotter
Homeostasis and Body
Temperature
• Rectal thermometers most accurate means of determining CBT, but CBT unlikely to affect treatment
Thermoregulatory Mechanisms
• Hypothalamus hosts main thermoregulatory center.
• Hypothalamus receives signals from:
− Thermoreceptors in skin and muscles
− Central receptors in core, triggered by blood temperature changes
Thermoregulatory Mechanisms
• At rest, the body:
− Produces heat by metabolism of nutrients, with liberation of water and carbon dioxide
• Basal metabolic rate (BMR): Heat energy produced at rest from normal body metabolic reactions
Thermoregulatory Mechanisms
• BMR of average 70-kg person is around
70 kcal/hour, based on factors including:
− Age
− Gender
− Stress
− Hormones
Thermoregulatory Mechanisms
• Heat loss to environment increases as ratio of body surface area to body volume increases.
− With two people of the same weight, the shorter will have a higher BMR.
− Exertion affects metabolic rate.
Thermoregulatory Mechanisms
• Heat generated by metabolism and glycogen breakdown warms the body.
− Excess dissipated by temperature gradient between body and outside environment
− If environmental temperature is higher, body heats by absorption of outside heat.
Thermoregulatory Mechanisms
• Skin plays vital role in body temperature regulation.
− Can both conserve and liberate heat energy through skin
• To liberate heat, blood flow to skin can include up to
8 L/min and 60% of cardiac output.
• In cold, blood flow can approach zero in certain areas.
Physiologic Reponses to Heat and Cold
• Thermolysis: Release of stored heat and energy of the body
− Increase in CBT causes vasodilation and sweating, which causes:
• Increased effective vascular system volume
• Increased heart output
• Increased pulse rate and stroke volume
Physiologic Reponses to Heat and Cold
• Cooling can be done by:
− Radiation —via electromagnetic waves
− Conduction —via direct physical contact
− Convection —moving air or liquids
− Evaporation —conversion of liquid to gas
Physiologic Reponses to Heat and Cold
• Thermogenesis: Production of heat and energy to deal with cold stressors
− Skin is body ’s thermostat in cold environment
− Shivers with cold skin, even if CBT not lowered
− Hypothalamus stimulates peripheral vasoconstriction to shunt blood to core.
− Heavier people are more insulated from cold.
Pathophysiology, Assessment, and Management of Heat Illness
• Heat illness: Increase in CBT due to inadequate thermolysis
− Inability to rid heat buildup from body because of:
• Hot and humid conditions, mobility
• General health/preexisting illness, age
Risk Factors for Heat Illness
• Older people are at particular risk
− Perspire less
− Acclimatize more slowly
− Feel thirst less readily
− Decreased mobility
− Chronic conditions
Risk Factors for Heat Illness
• Medications that affect temperature regulation ability include:
− Diuretics —dehydration and electrolyte disturbances
− Beta blockers —slow tachycardic response to heat stress
Risk Factors for Heat Illness
• Infants and young children are vulnerable.
− Proportionately higher metabolic heat production
− CBT rises faster during dehydration.
− Smaller organ and vascular systems do not dissipate heat as well.
• Military recruits and athletes also at increased risk
Heat Cramps
• Pathophysiology
− Acute, involuntary muscle spasms
− Occur from:
• Profuse sweating
• Sodium loss
− Most often afflict those in good physical condition
Heat Cramps
• Assessment
− Starts during strenuous or prolonged activity
− Usual presentation:
• Severe, incapacitating pain
• Hypotension and nausea
• Rapid pulse
• Pale and moist skin
• Normal temperature
Heat Cramps
• Management
− Treatment to eliminate exposure and restore lost salt and water:
• Move patient to cool environment.
• Position supine if feeling faint.
Heat Cramps
• Management (cont ’d)
− If no nausea:
• Give one or two glasses of salt-containing solution.
− If nauseated:
• Rapidly infuse normal saline by IV.
Heat Syncope
• Pathophysiology
− Orthostatic syncopal episode in nonacclimated people under heat stress
− Can occur from:
• Prolonged standing
• Standing suddenly from a sitting or lying positions
Heat Syncope
• Assessment and management
− Place patient in supine position.
− Replace fluid deficits.
− If patient does not recover quickly, suspect:
• Heatstroke
• Heat exhaustion
• Cardiac syncope
• Atypical acute coronary syndromes
Heat Exhaustion
• Pathophysiology
− Milder form of heat illness, with:
• Volume depletion
• Heat stress
− Two types:
• Water depleted
• Sodium depleted
Heat Exhaustion
• Exercise-associated hyponatremia
− Prolonged exertion with excessive fluid intake
− Too much water in body in relation to sodium
− Arginine vasopressin (AVP) contributing factor
• Hormone that increases water absorption in kidneys
Heat Exhaustion
• Symptoms include:
− Headache
− Fatigue
− Weakness
− Dizziness
− Nausea
− Vomiting
− Abdominal cramping
• Other signs and symptoms:
− Profuse sweating
− Pale, clammy skin
− CBT normal or slightly elevated
− Tachycardia
− Orthostatic hypotension
Heat Exhaustion
• Management
− Move to cool environment.
− Remove excess clothes.
− Place supine with legs elevated.
− If temperature is elevated:
• Sponge, spray, or drip with tepid water and fan gently.
− Oral hydration with sports drinks
Heat Exhaustion
• If suspected exercise-associated hyponatremia, no fluids by mouth
− Check blood sodium level.
− IV normal saline or hypertonic saline
Heatstroke
• Pathophysiology
− Least common but most deadly
− Caused by severe disturbance in body ’s thermoregulation
− Findings to determine heatstroke:
• Core temperature of more than 104 ° F (40 ° C)
• Altered mental status
Heatstroke
• Consequences are related to effects of elevated temperatures on the body ’s cells.
• Two heatstroke syndromes:
− Classic heatstroke
− Exertional heatstroke
Heatstroke
• Assessment
− Signs include:
• Irritability, combativeness
• Signs of hallucination
• Dehydration
• Dry, red, hot skin (classic heatstroke)
• Pale and sweaty skin (exertional heatstroke)
Heatstroke
• Fever and conditions that mimic heatstroke
− Fever can signal a fight against infection.
− Anticholinergic poisoning
− Syndromes that cause hyperthermia
− Malignant hyperthermia
Heatstroke
• Management
− Evaluate ABCs.
− Move patient to a cool environment.
− Cool as rapidly as possible.
− Start an IV line, and monitor cardiac rhythm.
− Prepare to treat for seizures.
Prevention of Heat Illness
• Measures to protect from heat illness:
− Acclimatize when possible.
− Maintain personal fitness.
− Limit time spent in heavy activity, especially during hot periods.
− Maintain hydration, eat appropriately, and rest.
− Improve cardiovascular and muscular strength.
Prevention of Heat Illness
• Be alert for early heat illness symptoms:
− Headache
− Nausea
− Cramps
− Dizziness
Local Cold Injury/Frostbite
• Often localized to extremities or exposed areas
• Frostbite: Ischemic injury classified as superficial or deep
− Frostnip is a mild form of frostbite.
Local Cold Injury/Frostbite
• Deeper degrees of frostbite —tissue freezes.
• Risk factors:
− Cold exposure without adequate clothing
− Impeding circulation to extremities
− Fatigue, dehydration, or hunger
− Direct contact with cold objects
− Hypothermia
Local Cold Injury/Frostbite
• Superficial frostbite: Altered sensation of numbness, burning
− Skin is:
• Waxy and white
• Firm to palpation
− Thawing causes:
• Cyanotic skin
• Hot, stinging sensation
Courtesy of AAOS
Local Cold Injury/Frostbite
• Deep frostbite
− White, yellowwhite, or mottled blue-white skin
− Feels hard, cold, without sensation
− Major damage when tissues thaw
• May cause gangrene
Courtesy of Dr. Jack Poland/CDC
Local Cold Injury/Frostbite
• Management
− Difficult to determine depth of injury
− Reperfusion injury can be excruciating.
− Treatment is determined by distance to hospital and if partially or completely thawed.
Local Cold Injury/Frostbite
• General principles:
− Remove from cold, and remove wet clothing.
− Do not rub or massage area.
− Transport with injured area elevated.
− Give pain medication as needed.
− Cover blisters with dry, sterile dressing.
− Consider rewarming if no potential of refreezing.
Local Cold Injury/Frostbite
• Principles of rewarming:
− Rewarm before transport if medical control agrees.
• Water bath —ensure immersion without touching container.
• Temperature between 98 ° F and 100 ° F
• Administer IV analgesia.
Trench Foot and Chilblains
• Trench foot similar to frostbite but can occur at temperatures as high as 60 ° F
− From prolonged exposure to cool, wet conditions
− Prevention best treatment —keep feet warm and dry.
Trench Foot and Chilblains
• Chilblains –itchy reddish or purple lesions on face or extremities
− Long exposure to temperature just above freezing
− Treatment:
• Remove from cold environment.
• Room temperature rewarming
Hypothermia
• Decrease in CBT starting at 95 ° F due to:
− Inadequate thermogenesis
− Excess environmental cold stress
© Andy Barrand, The Herald Republican/AP Photos
Hypothermia
• Body regulates cold stress by:
− Increasing thermogenesis
− Decreasing thermolysis
− Adaptive behavioral changes
Hypothermia
• Risk factors:
− Increased thermolysis
− Decreased thermogenesis
− Impaired thermoregulation
Hypothermia
• Hypothermic condition results from:
− Cold temperatures
− Improper gear
− Wetness and dehydration
− Length of exposure
− Intensity of weather conditions
Hypothermia
• Alcohol is the most common cause of heat loss in urban settings.
− Hinders body ’s attempt to insulate warm core
• Impairs shivering thermogenesis.
• Promotes cutaneous vasodilation.
• Inadequate glycogen stores from liver disease
• Subnormal nutritional status
• Impairs judgment.
Hypothermia
• Others at risk include:
− Those using:
• Sedative medications
• Tricyclic antidepressants
• Phenothiazines
− Older patients
− Trauma patients
Hypothermia
• Ensure ambulance is preheated.
− Conserve patient ’s body heat.
© Jim Cole/AP Photos
Hypothermia
• National Institutes of Health —focus on
“umbles” in early stages:
− Stumbles
− Mumbles
− Fumbles
− Grumbles
Hypothermia
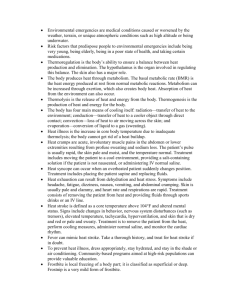
• 2010 American Heart Association ACLS guidelines define:
− Mild hypothermia —CBT greater than 93.2
° F
− Moderate hypothermia —CBT between 86 ° F to
93.2
° F
− Severe hypothermia —CBT below 86 ° F
Hypothermia
• Classifications:
− Acute
− Subacute
− Chronic
• Also classified as:
− Primary
− Secondary
Hypothermia
• No strong correlation between specific CBT and signs and symptoms.
− Most dramatically apparent in CNS, where everything slows
• Thinking and feeling
• Speaking slow and slurred
• Impaired reasoning ability and coordination
Hypothermia
• Signs and symptoms may resemble:
− Stroke
− Head injury
− Acute psychiatric disturbance
− Alcohol intoxication
Hypothermia
• Changes in cardiovascular system lead to:
− Increase in blood viscosity
− Impaired circulation and hypovolemic state
− State of hypovolemia
Hypothermia
• 2010 AHA guidelines suggest attempting defibrillation once.
− If persisting, treatment may include repeating attempts in conjunction with rewarming.
• Respiratory rate initially speeds up, then slows, with decreased minute volume:
− Tracheobronchial secretions increase
− Bronchospasm
− Pulmonary edema
Hypothermia
• Muscular system slows.
− Initial reaction is shivering.
− Shivering stops at around 91 ° F.
• Cold muscles become progressively weaker and stiffer.
Hypothermia
• Care aimed at preventing more heat loss and rewarming
− Strip patient of wet cloths.
− Insulate patient from further heat loss.
Hypothermia
• Breathing patients with pulse
− Mild hypothermia (93.2
° F)
• Passive rewarming
− Moderate hypothermia (86 ° F to 93.2
° F)
• If perfusing rhythm, active external rewarming
− Severe hypothermia (Less than 86 ° F)
• Active core rewarming sequence in-hospital
Hypothermia
• Patients with no pulse or not breathing
− 2010 BLS guidelines recommend CPR if no signs of life are present.
• Rapid rhythm identification
• One defibrillation attempt
• IV access and infuse warm normal saline
• Attempt advanced airway, and give warm, humid oxygen.
Hypothermia
• Patients are generally considered dead if:
− Obvious lethal traumatic injuries
− So solidly frozen as to block airway or chest compression efforts
• Resuscitation unlikely if submersion precedes arrest.
Drowning
• Process of experiencing respiratory impairment from submersion or immersion in liquid
• Outcomes include:
− Death
− Morbidity
− Near morbidity
Drowning
• Drowning continuum:
− Breath holding
− Laryngospasm
− Accumulation of carbon dioxide/inability to oxygenate lungs
− Respiratory and cardiac arrest from tissue hypoxia
Drowning
• Risk factors:
− Toddlers — bathtubs
− School-age children —pools
− Teens —lakes and rivers
− Comorbidities
Drowning
• Predictable sequences starting with inability to keep face out of liquid
− Length of breath holding depends on:
• State of health and fitness
• Level of panic
• Water temperature
Drowning
• Resuscitation is the same as for others in respiratory or cardiac arrest.
• Reaching victim — leave to those trained/experience d in water rescue
Drowning
• Treatment follows ABCs.
− Establish airway.
− Cervical spine precautions, especially if:
• History of diving or water slide
• Signs of injury
• Alcohol intoxication
Drowning
• Continue rescue breathing until on land.
• Once on solid surface:
− Start supplementary oxygen.
− Determine pulse.
− Continue to treat according to ABC guidelines.
Drowning
• Start chest compressions after two breaths.
− Establish IV access.
− Administer indicated medications.
− Perform cardiac monitoring.
− Defibrillate shockable rhythms.
− Do not perform manual abdominal thrusts.
− Suction to clear airway.
Drowning
• Most drowning victims receiving rescue breathing or compressions will vomit.
− Remove vomit from mouth via:
• Suction
• Finger swipes
• Other devices
− Consider placing on side.
Drowning
• Maintain some positive pressure at end of exhalation to:
− Keep alveoli open.
− Drive fluid accumulated in alveoli back into interstitium or capillaries.
Drowning
• Positive end-expiratory pressure (PEEP)
− Maintains some positive pressure at end of expiratory phase.
− Indicated for intubated patients with long transports
− Some devices allow PEEP via endotracheal tube.
− Portable ventilators usually have PEEP setting.
Drowning
• If ET tube inserted, insert nasogastric tube to decompress stomach.
• If pulse absent, implement ALS measures for cardiopulmonary arrest:
− IV access
− Epinephrine administration
− Cardiac monitoring, defibrillation if needed
Drowning
• Do not give up on submersion patient.
− Successful resuscitation with complete neurologic recover in more than 1 hour of submersion in icy water
• Hypothermia protects body and brain from hypoxia
• Hypothermia more often dangerous than protective
Drowning
• Search for comorbidities:
− Trauma
− Hypoglycemia
− Acute coronary syndrome
− Cerebrovascular accident
Drowning
• Major predictors of outcome:
− Length of submersion
− Response to field resuscitation
− If awake upon hospital arrival, likely a better outcome
Drowning
• Postresuscitation complications
− Occur hours to days after submersion:
• Adult respiratory distress syndrome
• Hypoxic brain injury
• Multiorgan failure
• Sepsis syndrome
Diving Injuries
• Four modes of diving
− Scuba
− Breath-hold
− Surface-tended
− Saturation
General Pathophysiology: Physical
Principles of Pressure Effects
• Pressure —a force per unit area
− Different ways to express; for example, weight of air at sea level:
• 14.7 pounds per square inch
• 760 mm Hg
• 1 atmosphere absolute (ATA) (most common)
General Pathophysiology: Physical
Principles of Pressure Effects
• Water much denser than air.
− For every 33 feet of seawater (fsw), pressure increases 1 ATA
• Sea level —pressure is 1 ATA
• 33 fsw —pressure is 2 ATA
• 66 fsw —pressure is 3 ATA
− Majority of scuba diving is at depths between 60 and 120 fsw (3 to 5 ATA).
General Pathophysiology: Physical
Principles of Pressure Effects
• Liquid volume does not change with pressure.
− Body/tissues primarily water —not so affected by pressure changes in descent or ascent
− Gas-filled organs are compressible and follow several physical laws.
General Pathophysiology: Physical
Principles of Pressure Effects
• Boyle ’s law—at a constant temperature, volume of a gas is inversely proportional to its pressure:
− Double pressure on gas, halve volume ( PV = K )
General Pathophysiology: Physical
Principles of Pressure Effects
• Effect is most extreme near surface.
• Explains barotraumas that occur in gas-filled body areas
General Pathophysiology: Physical
Principles of Pressure Effects
• Dalton ’s law—each gas in mixture exerts same partial pressure it would exert if it were alone in the same volume
− The total pressure of a mixture of gases is the sum of the partial pressures of all gasses in the mixture.
• Fresh air —P total
= PO
2
+ PCO
2
+ PN
2
General Pathophysiology: Physical
Principles of Pressure Effects
• Henry ’s law—the amount of gas dissolved in a liquid is directly proportional to the partial pressure of the gas above the liquid
− P – kC
General Pathophysiology: Physical
Principles of Pressure Effects
• Commercial divers use a decompression schedule.
− Recreational divers —no-decompression limit to keep from decompressing
− Enriched Nitrox gas decreases risk of nitrogen narcosis.
General Assessment:
Diving History
• When did symptoms start?
• Type of diving and equipment?
• Type of tank?
• Diving site and water temperature?
General Assessment:
Diving History
• Number of dives in the last 72 hours, and:
− Depth?
− Bottom time?
− Surface interval?
• Dive computer used?
• Safety stops used?
General Assessment:
Diving History
• Any attempts at in-water decompression?
• Any dive complications?
• What were predive and postdive activities?
Injuries at Depth
• Nitrogen narcosis: Altered mental status from breathing compressed nitrogencontaining air at depth
Injuries at Depth
• Signs and symptoms:
− Euphoria
− Inappropriate and dangers behavior
− Tingling of lips, gums, and legs
− May panic and surface too quickly.
Injuries at Depth
• Management
− Lower nitrogen partial pressure through:
• Controlled ascent
• Use of a mixed gas for diving with a decreased nitrogen percentage
Barotrauma
• Result of pressure imbalance between gasfilled spaces in the body and external atmosphere
− Can affect any gas-filled space in the body
− Scuba divers generally protected by breathing compressed air
Barotrauma
• Pressure in middle ear cannot be equalized with outside water pressure if:
− Blockage of eustachian tube
− Valsalva maneuver does not equalize pressure.
• “Middle ear squeeze” syndrome causes severe pain.
• If tympanic membrane ruptures
− Nausea/vomiting
− Vertigo
− Panic/rapid ascent
Barotrauma
• Treatment:
− Loose dressing for bleeding ear
− IV antiemetics or sedatives
− Possible decompression symptoms:
• Hearing loss
• Vertigo
Pulmonary Overpressurization
Syndrome (POPS)
• If divers fail to exhale during ascent, pressure in lungs increases.
• POPS ( “burst lung”) causes:
− Pneumothorax
− Mediastinal/subcutaneous emphysema
− Alveolar hemorrhage
− Lethal arterial gas embolism (AGE)
Pulmonary Overpressurization
Syndrome (POPS)
• Relative pressure and volume changes greatest near surface of water.
− Small overpressurization can rupture alveoli.
− Diving students trained to exhale constantly during ascent to vent air from lungs.
− COPD and asthma patients have slightly higher risk
Pulmonary Overpressurization
Syndrome (POPS)
• Signs and symptoms depend on where escaping air ends up; most often into mediastinum and beneath skin, causing:
− Full sensation in throat
− Pain on swelling
− Dyspnea
− Substernal chest pain
Pulmonary Overpressurization
Syndrome (POPS)
• Physical examination may show:
− Palpable subcutaneous air above clavicles
− Crunching noise synchronous with heartbeat audible by auscultation (Hamman ’s crunch)
Pulmonary Overpressurization
Syndrome (POPS)
• Prehospital treatment depends on if arterial gas embolism is present
• In the field, provide 100% oxygen by nonrebreathing mask.
Arterial Gas Embolism
• Air bubbles from ruptured alveoli enter pulmonary capillaries and travel back to left side of heart.
− Bubbles may enter coronary arteries and produce effects of MI.
− Majority rise to head, causing strokelike symptoms.
Arterial Gas Embolism
• Dramatic clinical picture, with symptoms:
− Involving most cerebral functions
− Appearing within seconds to minutes after surfacing
• History of panic or uncontrolled ascent, but can occur in shallow water
Arterial Gas Embolism
• Patient can experience:
− Weakness or paralysis of extremities
− Seizure activity
− Unresponsiveness
− Parasthesias
− Visual disturbances
− Deafness
− Changes in mental status
Arterial Gas Embolism
• Transport to a hyperbaric chamber facility as soon as possible.
Courtesy of Perry Baromedical Corporation
Arterial Gas Embolism
• Treatment includes:
− Ensure adequate airway.
− Administer 100% supplemental oxygen.
− Transport in supine position by ground.
− Establish IV access, and administer normal saline.
− Monitor cardiac rhythm.
Decompression Sickness
• Nitrogen bubbles in blood and tissues come out of solution during ascent.
− Bubbles cause damage by:
• Interfering mechanically with tissue perfusion
• Triggering chemical changes in body
− Multisystem disorder —can potentially affect every organ in the body
Decompression Sickness
• Nitrogen and oxygen are carried to tissues; oxygen is metabolized, but nitrogen remains.
− If ascent slow enough, enough nitrogen will escape with each breath.
− If ascent more rapid than nitrogen can be removed, diver ’s tissues will begin to bubble.
Decompression Sickness
• Other risk factors include:
− Obesity
− Dehydration
− Fatigue
− Flying within 12 to14 hours of diving
Decompression Sickness
• Risk of severe neurologic DCS if patient has a patent foramen ovale
− Congenital defect in which foramen ovale between atria fails to close at birth
− May allow nitrogen bubbles to travel from pulmonary circulation into systemic circulation
− Increased damage to CNS and proximal spinal cord
Decompression Sickness
• Type I —mild form that involves only:
− Skin
− Lymphatic system
− Musculoskeletal system
• Symptoms:
− Joint pain
− Mottled and pruritic skin
− Fatigue and weakness
− Lymph dysfunction leading to edema
(rare)
Decompression Sickness
• Type II —symptoms in all other organ systems:
− Pulmonary
− Cardiovascular
− Nervous
Decompression Sickness
• Management :
− Administer 100% oxygen.
− Manage acute problems.
− Transport to hyperbaric facility, even if symptoms appear to resolve.
Hyperbaric Oxygen Therapy
• Intermittent inhalation of pure oxygen under pressure greater than 1 ATA
− Mechanically reduces bubble size.
− Reduces nitrogen content.
− Increases oxygen delivery to ischemic tissues.
• Treatment pressures and times from established tables
Hyperbaric Oxygen Therapy
• Indicated in patients with:
− AGE
− DCS
− Carbon monoxide poisoning
− Other subacute or chronic medical conditions
− Routine decompression of industrial divers
Hyperbaric Oxygen Therapy
• Risks:
− May convert a pneumothorax into a tension pneumothorax if no chest tube
− Seizures from oxygen toxicity
− Barotrauma
Hyperbaric Oxygen Therapy
• Care recommended in patients who:
− Are pregnant
− Have lung disease
− Have fever
− Have seizure disorders
• In patients with possible AGE or DCS, benefits may outweigh risks.
Other Gas-Related Problems
• Most recreational divers use compressed air.
− Tanks with various mixtures of nitrogen/oxygen allow divers to be underwater longer.
− Less nitrogen —less likely to develop DCS
− More oxygen —prone to oxygen toxicity (CNS emergency)
Other Gas-Related Problems
• Signs and symptoms include:
− Dizziness
− Lack of coordination
− Confusion
− Twitching or paresthesia
− Underwater seizures
Other Gas-Related Problems
• Evacuation from water:
− Controlled ascent
− Ensure diver maintains airway and has air access during ascent.
• AGE risk does not increase when seizing or postictal patient is brought to surface.
− DCS may be a concern.
Other Gas-Related Problems
• Once back in boat or on shore, treatment includes:
− 100% oxygen
− Supportive therapy
− Hyperbaric oxygen therapy in pregnant patients or those with significant exposure
Shallow Water Blackout
• Frequently seen in teenage boys competing in remaining the longest underwater
− May hyperventilate just before going under to extend endurance
• Decreases PaCO
2
, causing cerebral vasoconstriction
• PaO
2 increases as swimmer descends.
Shallow Water Blackout
• Because PaCO
2 drive suppressed is relatively low, respiratory
− Diver can remain underwater longer, but oxygen continues to be removed from alveoli
− Cerebral function maintained at depth by increased PaO
2
Shallow Water Blackout
• On surfacing:
− Ambient pressure rapidly decreases.
− PaO
2 plummets.
− Hypoxia and cerebral vasoconstriction together cause blackout just before reaching surface.
Shallow Water Blackout
• Treat as for any other case of drowning.
• When patient regains consciousness, explain seriousness of injury.
Shallow Water Blackout
• DAN —24-hour consultation service
− (919) 684-8111
− Connect with physician experienced in diving medicine who can:
• Assist with diagnosis.
• Provide advice for early management.
• Supervise referral to recompression chamber.
Altitude Illness
• Altitude: Terrestrial elevation above 1,500 m
(5,000 ft)
− Level where physiologic changes from hypobaric hypoxia begin
− Altitude illness: Low partial pressure of oxygen leads to hypoxia
Altitude Illness
• Barometric pressure varies according to:
− How far from the equator
− Season –typically lower in winter
− Local changes in barometric pressure, can alter
“relative altitude” by 500 to 2,500 ft.
Altitude Illness
• Types:
− Acute mountain sickness (AMS)
− High-altitude cerebral edema (HACE)
− High-altitude pulmonary edema (HAPE)
Altitude Illness
• Typically occurs in those rapidly ascending to above 8,000 ft, but can occur as low as
6,500 ft.
− Symptoms usually within 6 to 10 hours.
− Directly related to how high and how quickly arrived
Altitude Illness
• Body adjusts by defending amount of oxygen available for delivery to tissues.
− First response is hyperventilation.
− Quickly leads to respiratory alkalosis
− Kidneys secrete bicarbonate in urine.
− Causes compensatory metabolic acidosis
Altitude Illness
• Hypoxia main problem but mechanism poorly understood
− Initiates series of reactions that cause overperfusion to brain and lungs, increasing:
• Capillary pressures
• Leakage
• Cerebral and pulmonary edema
Altitude Illness
• HAPE results from marked vasospasm of pulmonary arteries.
− Results in high pressure driving fluid from pulmonary vasculature into lungs
− Does not result from volume overload state
• Nitroglycerin and furosemide not used for HAPE
Altitude Illness
• Risk factors
− History of AMS
− Normal residence below 3,000 ft
− Obesity
− Rapid or high ascents
© Alan Heartfield/ShutterStock, Inc.
Altitude Illness
• Acute mountain sickness (AMS) symptoms include headache plus:
− Fatigue or weakness
− GI symptoms
− Dizziness or light-headedness
− Difficulty sleeping
Altitude Illness
• High-altitude pulmonary edema (HAPE)
− Two of the following:
• Dyspnea at rest
• Cough
• Weakness
• Chest tightness or congestion
− Two of the following:
• Central cyanosis
• Audible rales or wheezing
• Tachypnea
• Tachycardia
Altitude Illness
• High-altitude cerebral edema (HACE)
− Presence of change in mental status or ataxia in a person with AMS
− Presence of mental status changes and ataxia in a person without AMS
Altitude Illness
• Signs of possible causes other than AMS:
− Symptoms develop 4 or more days after higher elevations
− Lack of headache
− Failure of descent to improve signs or symptoms
Altitude Illness
• Management of all altitude illnesses includes
− Oxygen
− Descent
− Evacuation
− Various treatments specific to illness
Altitude Illness
• Prevention by:
− Acclimatization
− Use of acetazolamide for most susceptible
Altitude Illness
• AMS treatment :
− Acetaminophen or aspirin for headaches
− Antiemetics for nausea
− Acetazolamide for AMS and acclimatization
− Oxygen
− Do not ascend until symptoms resolve.
Altitude Illness
• HAPE treatment:
− Immediate descent
− Oxygen
− Medication as adjunctive treatment limited to patients where:
• Descent and oxygen are not easily available.
• Descent and oxygen do not rapidly help patient.
Altitude Illness
• HACE treatment:
− Oxygen
− Mandatory descent
− Dexamethasone given as soon as possible
• 8 mg by any accessible route, followed by 4 mg every 6 hours during descent/evacuation
Portable Hyperbaric Chambers
• Useful when descent cannot be carried out
• Patient placed inside bag and pressurized air pumped in
− Provides equivalent of descent of several hundred to several thousand feet
Lightning Strike
• Leading cause of environmental death in
United States
• Different than industrial electrical injuries:
− Not AC or DC current
− Massive unidirectional flow, voltages in millions
− Duration miniscule
− Energy flows over victim.
Lightning Strike
• Most common injury is side splash injury
• Bolt ’s energy may act as a giant depolarizing charge to body.
− Can cause asystole and respiratory arrest:
• Diaphragm depolarization
• Brainstem-induced central apnea
Lightning Strike
• After depolarization:
− Heart usually spontaneously resumes sinus rhythm.
− Respiratory effort does not restart.
− If apnea remains, heart will go into secondary hypoxic arrest.
Lightning Strike
• Morbidity high
− As many as 75% have long-term complications
− May have
“Lichtenberg figure ”
− Evaluate for trauma.
Lightning Strike
• “Reverse triage”
− Attend those who appear dead first.
− Strikes induce cardiac and respiratory arrest.
− CPR/rescue breathing
• All lightning strike victims should be evaluated at a medical facility.
Envenomation: Bites and
Stings
• Most common venomous creatures
− Bees, wasps, hornets, fire ants
− Snakes
− Black widow, brown recluse, hobo spiders
− Scorpions
Envenomation: Bites and
Stings
• Most frequent cause of mortality — anaphylactic reaction
− Most common and most deaths from hymenoptera bites
− Treatment is same as in other cases of anaphylaxis
Envenomation: Bites and
Stings
• Treatment includes:
− ABCs management
− Transport
− Obtain vascular access.
− Ensure scene is safe from venomous creatures.
Hymenoptera
• Most common cause of deaths:
− European honey bees (Aphidae)
− Yellow jackets, wasps, hornets
(Vespidae)
− Fire ants
(Formicidae)
© Stuart Elflett/ShutterStock, Inc.
Hymenoptera
• Venom is a mixture of proteins causing local reactions:
− Erythema
− Swelling
− Pruritus
• Melittin —protein that causes immediate pain
Hymenoptera
• Local reaction in ¼ of stings.
− Reaction can be extensive.
• Anaphylaxis occurs rapidly, typically within
10 minutes (within 60 minutes 95% of time).
Hymenoptera
• If no history of allergic reaction and no systemic reaction, transport is not necessary.
− Advise patient of anaphylaxis signs.
− Wound should be checked if no improvement in
24 hours
− Infection likely from fire ant stings
Hymenoptera
• Treatment focuses on pain and minimization of infection risk.
− Determine if stinger and venom sac are still attached.
• If so, remove as rapidly as possible.
• Clean wound thoroughly.
• Cool compresses and elevation for reaction
• Antihistamines for symptomatic treatment
Hymenoptera
• Additional treatment for fire ant stings include:
− Moving patient and crew away from site.
− Brushing off ants.
− Providing supportive care as needed.
Snake Bites
• Two snake families of concern in United
States:
− Viperidae
− Elapidae
• Most common in southeastern United
States
Snake Bites
• Pit viper venom has both hemolytic and proteolytic enzymes, causing extensive local tissue damage and systemic effects:
− Soft-tissue swelling and necrosis
− Local, then systemic bleeding
− Clotting problems
Snake Bites
• Coral snakes have potent neurotoxic venom:
− Paresthesias
− Fasciculations
− Weakness
− Respiratory difficulty
− Strokelike symptoms
Snake Bites
• Pit vipers
− Heat-sensing pits between the eye and the nostril
− Main types:
• Rattlesnakes
• Cottonmouths
• Copperheads
Snake Bites
• Coral snakes
− Small fangs
− Snakes need to stay attached for envonemation.
− Several hours for symptoms to show
− Transport if possible bite
Courtesy of Luther C. Goldman/U.S. Fish & Wildlife Service
Snake Bites
• Be certain snake is no longer a danger.
• Note time of bite.
• Determine type of snake.
− Remember —dead snakes can still bite.
Snake Bites
• Crotalid venom
− Promotes tissue destruction through:
• Proteolysis
• Hemolysis
•
Thrombogenesis
• Elapid venom
− Neurotoxin causing respiratory failure and death
Snake Bites
• Crotalid bite symptoms include:
− Swelling, bleeding
− Weakness
− Unconsciousness
− Tachycardia
− Coagulopathies
− Shock, cardiovascular collapse
Courtesy of AAOS
Snake Bites
• Degree of envenomation determined by symptoms:
− Mild —minimal local swelling with no systemic symptoms
− Moderate —swelling extending up extremity, systemic symptoms; no significant bleeding
− Severe —extensive soft-tissue swelling and severe systemic effects and bleeding
Snake Bites
• Treatment —provide antivenin (at hospital).
− Monitor ABCs.
− Clean wound with antimicrobials.
− Draw blood for hospital use (if protocols allow).
− Immobilize involved extremity in neutral position below heart level.
− Do not use excessive constriction.
− Remove constricting jewelry.
Spider Bites
• Estimated 34,000 species worldwide
• Most carnivores and can bite
• Three species of concern in US:
− Black widow
− Brown recluse
− Hobo spiders
Spider Bites
• Black widow —only female dangerous
− Glossy black with
½-inch oval body
− Orange or reddish hourglass mark
− Lives in sheds, basements, woodpiles
− Most bites on hands or forearms
© Crystal Kirk/ShutterStock, Inc.
Spider Bites
• Brown recluse
(fiddleback) spider:
− Southern Midwest to Southeast
− Not aggressive, bites only when accidently encountered
Courtesy of Kenneth Cramer, Monmouth College
Spider Bites
• Hobo spiders
− Found in Northwest
− Bite clinically similar to brown recluse
− Slightly more aggressive
Spider Bites
• History of spider bite not always confirmed.
− Patient may report:
• Sudden, sharp prick followed by cramping
• Numbing pain beginning at bite area and gradually spreading
• Extreme restlessness (in case of black widow bite)
Spider Bites
• Black widow one of most venomous North
American spiders
− Local pain with rapid onset within 30 to 60 min
− Local muscle spasm and localized diaphoresis
− Diffuse and more muscle spasms
− If diaphragm affected, may have respiratory difficulty
Spider Bites
• Brown recluse bites usually painless
• Small percentage develop local and/or systemic symptoms
• Some may develop loxoscelism.
Courtesy of Department of Entomology, University of Nebraska
Courtesy of Department of Entomology, University of Nebraska
Spider Bites
• Black widow spider bite treatment:
− Intermittent ice use
− Antimicrobial cleansing of wound
− Pain and muscle spasm relief
− Prompt transport
• Further treatment:
− Monitor ABCs.
− IV access, oxygen
− Narcotics, muscle relaxants/sedatives
− Antivenin reserved for young and old with severe envenomation
Spider Bites
• Brown recluse/hobo spider bite treatment:
− Antivenin not routinely available
− Previous treatments (dapsone, steroids) shown to have no benefit
Scorpion Stings
• Only the bark scorpion is a potential threat to humans.
− Most result in a painful local reaction.
− Venom located in stinger ’s glands © Visual&Written SL/Alamy Images
Scorpion Stings
• Local sting symptoms within minutes, last several hours:
− Erythema
− Pruritis
− Urticaria
− Sharp, burning pain
− Paresthesia
Scorpion Stings
• A sting from the more neurotoxic bark scorpion causes few local symptoms.
− Systemic symptoms begin within minutes
− Peak at 4 to 6 hours
− Resolve within 24 to 72 hours
Scorpion Stings
• Symptoms
− Sympathetic stimulation:
• Tachycardia
• Hypertension
•
Palpitations
• Dry mouth
• High temperature
− Parasympathetic stimulation:
• Bradycardia
•
Hypotension
• Salivation
• Defecation
• Cranial nerve findings
Scorpion Stings
• Symptoms (cont ’d)
− Somatic stimulation
• Muscle contractions
• Myoclonic jerking
• Fasciculations
Scorpion Stings
• Prehospital treatment:
− ABCs
− Monitoring
− Transport
− Intubation if necessary
− IV for volumes needed for blood pressure
Scorpion Stings
• Prehospital treatment (cont ’d):
− Ice pack for local swelling
− Immobilize extremity
− Constricting band
− Treat seizures per protocol
Scorpion Stings
• In-hospital treatment includes care for
ABCs:
− Alpha and beta blockers
− Atropine
− Vasoactive drugs
− Antivenin if available
Tick Bites
• Blood-sucking arthropods found in rural, wooded areas
− Bites a concern because of disease transmission
• Lyme disease
• Rocky Mountain spotted fever
© Joao Estevao A. Freitas (jefras)/ShutterStock, Inc.
Tick Bites
• Treatment
− Remove tick:
• Use curved forceps to grab head as close to skin as possible.
• Pull straight up using even pressure.
• Do not twist or jerk.
• Dispose of it in container of alcohol.
Tick Bites
• Once tick is removed:
− Wash bite with soap and water.
− May be no reason to transport if patient is asymptomatic (check with local protocol).
− Advise patient to see a physician.
Summary
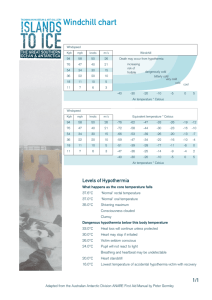
• Environmental emergencies: Medical conditions caused or worsened by weather, terrain, or unique atmospheric conditions such as underwater or high altitude
• Predisposing risk factors include very young, elderly, poor state of health, and certain medications.
Summary
• Thermoregulation: Body ’s ability to ensure a balance between heat production and release, with the hypothalamus and skin playing major roles
• Body produces heat through metabolism; basal metabolic rate is the heat energy produced at rest from normal metabolic reactions.
Summary
• Thermolysis: Release of heat and energy from the body
• Thermogenesis: Production of heat and energy for the body
• The body has four main means of cooling itself —radiation, conduction, convection, and evaporation.
Summary
• Heat illness: Increase in core body temperature from inadequate thermolysis
• Heat cramps: Acute, involuntary muscle pains in abdomen or lower extremities from profuse sweating and sodium loss
• Heat syncope occurs when overheated patient suddenly moves. Place patient supine and replace fluids.
Summary
• Heat exhaustion can result from dehydration and heat stress.
• Heatstroke: Core temperature above 104 F
(40oC) and altered mental status
• Fever can mimic heatstroke.
• Dress appropriately, stay hydrated, and stay in shade or air conditioning to prevent heat illness.
Summary
• Frostbite: Local freezing of a body part and is classified as superficial or deep
• Superficial frostbite is characterized by numbness, tingling, or burning. The skin is white, waxy, and firm to palpation.
• Deep frostbite is characterized by white, yellow-white, or mottled blue-white injured body part and is hard, cold, and without sensation.
Summary
• Trench foot results from prolonged exposure to cool, wet conditions.
• Hypothermia: Decrease in core body temperature; can be mild, moderate, or severe
• Mild hypothermia: Core body temperature of greater than 93 ° F (33.9
° C)
Summary
• Moderate hypothermia: Core body temperature from 86 ° F to 93 ° F (30 ° C to
33.9
° C)
• Severe hypothermia: Core body temperature of less than 86 ° F (30 ° F).
• Resuscitate hypothermic patients who are not breathing or without a pulse.
• Resuscitation can be attempted in cases of cardiac arrest and hypothermia.
Summary
• Drowning: Process of experiencing respiratory impairment from submersion or immersion in liquid
• Rescuing a patient who has drowned should be undertaken by specially trained rescuers.
• For diving injuries, obtain details such as type of diving, type of tank, number of dives in the past 72 hours, and predive and postdive activities.
Summary
• Barotrauma can happen during dive descent from the pressure imbalance between the inside of the body and the outside atmosphere.
• Nitrogen narcosis: Altered mental status from breathing compressed air at depth
• Pulmonary overpressurization syndrome
(POPS, burst lung) can occur if a diver ascends too quickly.
Summary
• Pulmonary overpressurization syndrome may lead to arterial gas embolism.
• Barotrauma treatment depends on whether there is an air embolism. A pneumothorax may require needle decompression. With an air embolism, the patient must receive treatment in a hyperbaric chamber.
• In decompression sickness, nitrogen bubbles in blood and tissues during dive ascent.
Summary
• Shallow water blackout occurs when a person hyperventilates just before diving and passes out before resurfacing.
• The Divers Alert Network is a resource for diving-related injuries.
• Altitude illness occurs when unacclimatized people ascend to altitude, with types including AMS, HACE, and HAPE.
Summary
• Symptoms of AMS include headache and fatigue, weakness, gastrointestinal symptoms, dizziness, light-headedness, and difficulty sleeping.
• Symptoms of HACE include mental status changes and/or ataxia in a person with acute mountain sickness or the presence of both in a person without acute mountain sickness.
Summary
• Symptoms of HAPE include at least two of the following: dyspnea at rest, cough, weakness, or chest tightness or congestion, and at least two of the following: central cyanosis, audible rales, wheezing, tachypnea, or tachycardia.
• Treatment of altitude illness includes descending or use of a portable hyperbaric chamber, providing oxygen, and administering IV medications.
Summary
• Cardiopulmonary resuscitation should be started promptly for lightning strike victims.
• In lightning strike cases, victims who appear to be dead should be treated first.
• Anaphylactic reaction is the most frequent mortality cause from insect bites and envenomations.
Summary
• To decrease toxin exposure, promptly remove hymenoptera stingers or venom sacs.
• Fire ant stings may result in infection.
• Most snake bites in the United States are from pit vipers.
• If there are visible fang marks with no bleeding with a crotalid bite, it is likely a “dry bite ” with no venom.
Summary
• For scene safety, ensure the snake is dead, gone, or trapped in cases of envenomation.
• All significant snake envenomations require antivenin treatment.
• The most concerning spider bites are from the female black widow, the brown recluse, and the hobo spider.
• A small subset of patients with brown recluse spider bites may develop loxoscelism.
Summary
• Scorpion stings produce a neurotoxic reaction causing autonomic excitation.
• Scorpion sting treatment is largely supportive and includes airway protection.
• Tick bites can transmit serious illnesses and rarely cause life-threatening paralysis.
Credits
• Chapter opener : Courtesy of BM1 Kevin
Erwin/U.S. Coast Guard
• Backgrounds : Red – © Margo Harrison/
ShutterStock, Inc.; Green – Jones & Bartlett
Learning; Purple – Courtesy of Rhonda Beck;
Blue – Courtesy of Rhonda Beck.
• Unless otherwise indicated, all photographs and illustrations are under copyright of Jones & Bartlett
Learning, courtesy of Maryland Institute for
Emergency Medical Services Systems, or have been provided by the American Academy of
Orthopaedic Surgeons.