Chapter 38: Environmental Emergencies
advertisement

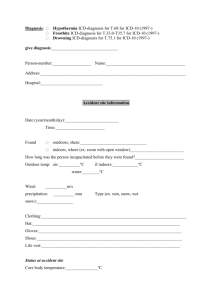
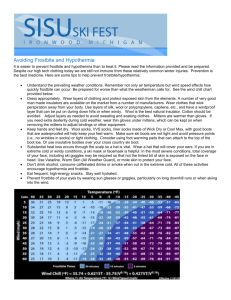
Chapter 38: Ready for Review Environmental emergencies are medical conditions caused or worsened by the weather, terrain, or unique atmospheric conditions such as high altitude or being underwater. Risk factors that predispose people to environmental emergencies include being very young, being elderly, being in a poor state of health, and taking certain medications. Thermoregulation is the body’s ability to ensure a balance between heat production and release. The hypothalamus is the organ involved in regulating this balance. The skin also has a major role. The body produces heat through metabolism. The basal metabolic rate (BMR) is the heat energy produced at rest from normal metabolic reactions. Metabolism can be increased through exertion, which also creates body heat. Absorption of heat from the environment can also occur. Thermolysis is the release of heat and energy from the body. Thermogenesis is the production of heat and energy for the body. The body has four main means of cooling itself: radiation— transfer of heat to the environment; conduction—transfer of heat to a cooler object through direct contact; convection—loss of heat to air moving across the skin; and evaporation— conversion of liquid to a gas (sweating). Heat illness is the increase in core body temperature (CBT) due to inadequate thermolysis; the body cannot get rid of a heat buildup. Heat cramps are acute, involuntary muscle pains in the abdomen or lower extremities resulting from profuse sweating and sodium loss. The patient’s pulse rate is usually rapid, the skin pale and moist, and the temperature normal. Treatment includes moving the patient to a cool environment, providing a salt-containing solution if the patient is not nauseated, or administering IV normal saline. Heat syncope can occur when an overheated patient suddenly changes position. Treatment includes placing the patient supine and replacing fluids. Heat exhaustion can result from dehydration and heat stress. Symptoms include headache, fatigue, dizziness, nausea, vomiting, and abdominal cramping. Skin is usually pale and clammy, and the pulse rate and respirations are rapid. Treatment consists of removing the patient from heat and providing fluids through sports drinks or an IV line. Heatstroke is defined as a core temperature above 104°F (40°C) and altered mental status. Signs include changes in behavior, nervous system disturbances (such as tremors), elevated temperature, tachycardia, hyperventilation, and skin that is dry and red or pale and sweaty. Treatment is to remove the patient from the heat, perform cooling measures, administer normal saline, and monitor the cardiac rhythm. Fever can mimic heatstroke. Obtain a thorough history, and treat for heatstroke if in doubt. To prevent heat illness, dress appropriately, stay hydrated, and stay in the shade or air conditioning. Community-based programs aimed at high-risk populations can provide valuable education. Frostbite is local freezing of a body part; it is classified as superficial or deep. Frostnip is a mild form of frostbite. Superficial frostbite is characterized by numbness, tingling, or burning. The skin is white, waxy, and firm to palpation. When thawed, the skin turns cyanotic and the patient feels a hot, stinging sensation. Treatment consists of getting the patient out of the cold; rewarming the injured part with body heat; covering with a warm, sterile dressing; and transporting the patient. In deep frostbite, the injured body part looks white, yellow-white, or mottled blue-white and is hard, cold, and without sensation. Major tissue damage can occur when the part thaws. Gangrene (permanent cell death) can result in the need for amputation. Treatment includes leaving the part frozen if it is found frozen, or rewarming the part if it is partially thawed. Trench foot is similar to frostbite but results from prolonged exposure to cool, wet conditions. Prevention is the best treatment. Hypothermia is a decrease in core body temperature. It can be mild, moderate, or severe. Mild hypothermia is a core body temperature of greater than 93°F (33.9°C). The patient shivers and may be confused, have slurred speech, or have impaired coordination. Treatment is passive rewarming such as removing wet clothing or drying the patient’s skin and possibly providing warm fluids. Moderate hypothermia is a core body temperature in the range of 86°F to 93°F (30°C to 33.9°C). Treatment is passive rewarming, active external rewarming of truncal areas, administering warmed IV fluids, and potentially using special rewarming devices. Severe hypothermia is a core body temperature of less than 86°F (30°C). Treatment is active internal rewarming, such as administering warm IV fluids, and in-hospital measures. Hypothermic patients who are not breathing or who do not have a pulse need resuscitation. Patients in cardiac arrest require high-quality CPR and possibly a single shock depending on the heart rhythm; follow local guidelines. Attempt to insert an advanced airway; deliver ventilation with warm, humidified oxygen; and provide IV fluids. Hypothermic patients with obvious lethal traumatic injuries or patients who are so frozen as to block the airway or chest compression efforts generally are dead. If the patient appears dead after prolonged exposure, hypothermia may protect the brain and organs. Resuscitation can be attempted in cases of cardiac arrest and hypothermia. Drowning is the process of experiencing respiratory impairment from submersion or immersion in liquid. Drowning progresses from breath holding, to laryngospasm, to respiratory and cardiac arrest. Caring for a patient who drowned starts with reaching the patient, a task that should be undertaken by specially trained rescuers. Treatment includes caring for the ABCs and taking cervical spine precautions. Positive end-expiratory pressure may be used to keep the alveoli open and drive fluid out. A nasogastric tube may be inserted to decompress the stomach if the patient is intubated. Submersion patients may develop bronchospasm and may require administration of a beta-2 adrenergic drug. In diving injuries, obtain as many details as possible about the patient, including the type of diving, type of tank, number of dives in the past 72 hours, and pre-dive and post-dive activities. Barotrauma can result during dive descent, owing to a pressure imbalance between the inside of the body and the outside atmosphere. It may result in ear pain. Treatment is a loose dressing for ear bleeding, and possibly IV antiemetics or sedatives. Nitrogen narcosis is a state of altered mental status caused by breathing compressed air at depth. Signs and symptoms include feeling euphoric; exhibiting inappropriate, foolish behavior; and tingling of the lips, gums, and legs. When a diver ascends too quickly, pulmonary overpressurization syndrome (POPS, also known as burst lung) can occur. Signs and symptoms include mediastinal and subcutaneous emphysema, a sense of fullness in the throat, pain on swallowing, dyspnea, and substernal chest pain. Arterial gas embolism is a dangerous consequence of pulmonary overpressurization syndrome. Air bubbles may travel to the coronary arteries, causing cardiac arrest. Symptoms include weakness or paralysis of the extremities, seizure activity, unresponsiveness, and other neurologic symptoms. Treatment of barotrauma depends on whether an air embolism is present. A pneumothorax may require needle decompression. With an air embolism, the patient must receive treatment in a hyperbaric chamber. Decompression sickness encompasses a broad range of signs and symptoms caused by nitrogen bubbles in blood and tissues coming out of solution on dive ascent. Symptoms include itchy skin, subcutaneous emphysema, swelling, rashes, joint and muscle pain, sensory and motor disturbances, incoordination, paralysis, chest pain, and dyspnea. Treatment is 100% oxygen, IV normal saline, and transport to a hyperbaric facility. Shallow water blackout occurs when a person hyperventilates just before diving underwater and passes out before resurfacing. Treatment is the same as for any other submersion. The Divers Alert Network is a valuable resource for divingrelated injuries. Callers are immediately connected to a physician experienced in diving medicine who can provide advice regarding specific management. Altitude illness occurs when unacclimatized people ascend to altitude. Types of altitude illness include acute mountain sickness (AMS), high-altitude cerebral edema (HACE), and high-altitude pulmonary edema (HAPE). Symptoms of acute mountain sickness include headache plus fatigue, weakness, gastrointestinal symptoms, dizziness, light-headedness, and difficulty sleeping. Symptoms of high-altitude cerebral edema include a change in mental status and/or ataxia in a person with acute mountain sickness or the presence of both in a person without acute mountain sickness. Symptoms of high-altitude pulmonary edema include at least two of the following: dyspnea at rest, cough, weakness, or chest tightness or congestion and at least two of the following: central cyanosis, audible rales, wheezing, tachypnea, or tachycardia. Treatment of altitude illnesses includes descending or using a portable hyperbaric chamber, providing oxygen, and administering certain IV medications. Cardiopulmonary resuscitation should be started promptly for lightning strike victims. Lightning strike victims should be evaluated using “reverse triage,” meaning that those people who appear to be dead should be treated first. Anaphylactic reaction is the most frequent cause of mortality from all insect bites and envenomations. Prompt removal of hymenoptera stingers or venom sacs can decrease toxin exposure. Fire ant stings often result in infection. Pit vipers (crotalids) are responsible for the greatest number of snake bites in the United States. With a crotalid bite, if there are visible fang marks with no bleeding, this indicates that a “dry bite” (with no venom) has occurred. In terms of scene safety, it is important to make sure the snake is dead, gone, or trapped in cases of envenomation. All significant snake envenomations require treatment with antivenin; transport promptly. The time between the occurrence of the bite and the time of treatment is crucial. The female black widow, the brown recluse, and the hobo spider produce the most concerning spider bites. A small subset of patients with brown recluse spider bites may develop loxoscelism. Scorpion stings produce a neurotoxic reaction that causes autonomic excitation. Treatment of scorpion stings is largely supportive, with protection of the airway. Tick bites can transmit a variety of serious illnesses, and in rare cases, can cause lifethreatening paralysis. Principal treatment is careful removal of the tick, and washing the area around the bite. Transport all patients with any neurologic symptoms.