Skeletal System - Castle High School
advertisement

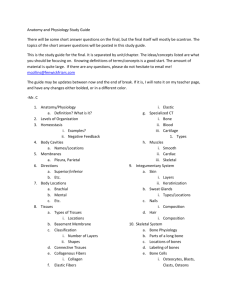
link Skeletal System Chapter 5 link Skeletal System • Two divisions: • Axial Skeleton (“axis”) • Head & trunk • Appendicular Skeleton (“appendages”) • limbs & their attachments to trunk • Also includes: • Joints • Cartilages • Ligaments 1. Support Functions of Bones • Internal framework, cradles soft organs 2. Protection • i.e. skull, vertebrae, rib cage 3. Movement • Used as levers by muscles 4. Storage • Fat is stored in yellow marrow (internal cavities) • Minerals stored in bone (calcium & phosphorus) 5. Blood Cell Formation • Hematopoiesis occurs in red marrow Classification of Bone • 206 bones in adult skeleton • Two types of osseous tissue: • Compact bone – dense, looks smooth & homogenous • Spongy bone – small needlelike pieces of bone & lots of open space Spongy & Compact Bone Bone Classification of Bones • Classified according to shape • Long bones – longer than they are wide; contain mostly compact bone • i.e. Bones of the limbs • Short bones – cube-shaped, contain mostly spongy bone • i.e. Bones of wrist and ankle, patella, sesamoid bones (within tendons) • Flat bones – thin, flattened, usually curved; compact bone sandwiches layer of spongy bones • i.e. Bones of the skull, ribs, sternum • Irregular bones – do not fit into one of the preceding categories • i.e. Vertebrae and hip bones Gross Anatomy of a Long Bone (Hyaline) metaphysis (disc) (DCT) Microscopic Anatomy of the Bone • Osteocytes (mature bone cells) • Lacunae (cavities in matrix) • Lemellae (concentric circles around central canal) • Central (Haversian) canal (carry blood vessels and nerves to all areas of the bone) • Osteon (Haversian System) • Canaliculi (radiate outward from central canal to all lacunae) • Volkmann’s canal (communication from exterior to interior of bone) Bone Tissue • Connective Tissue: calcified matrix with abundant collagen fibers • Four types of cells: • Osteogenic cells: unspecialized from stem cells; found along periosteum and endosteum • Make osteoblasts • Osteoblast: bone-building cells – synthesize and secrete collagen fibers • Osteocyte: mature cells – maintain metabolism • Osteoclasts: huge collection of white blood cells found in endosteum • release acids and enzymes that digest bone matrix (resorption) Bone Formation • Ossification (osteogenesis): formation of bone • Begins in 6th week of pregnancy • Two patterns: • Intramembraneous ossification: flat bones • i.e. skull & clavicles • Endochondral ossification: most bones • i.e. long bones Intramembraneous Ossification • Flat bones form on fibrous membranes • Mesenchymal cells cluster and form osteoblasts which harden • Form ossification center in membrane • Osteoblasts secrete bone matrix which mineralizes and traps cells in bones (become osteocytes) • Trabeculae then form followed by the periosteum forming around bone • Trabeculae then thicken to form bone collar and deeper remain distinct as spongy bone and eventually red marrow Endochondral Bone Development • Most bones develop using a hyaline cartilage model • Fetal skeleton = hyaline cartilage (formed from mesenchyme) • Two phases (Fig 5.5, page 140): 1. hyaline cartilage model covered with bone matrix (bone “collar”) by osteoblasts •Primary ossification: develops inward from outer surface & forms spongy bone (eventually compact bone) •Secondary ossification: develops outward (from center of epiphysis) 2. enclosed hyaline cartilage model digested away, opening up medullary cavity within newly formed bone •Osteoclasts break down center to form medullary cavity •By birth or shortly after, all cartilage converted to bone except articular cartilages (cover bone ends) and epiphyseal plates •Adult skeleton = cartilage exists in nose, parts of ribs, and joints Bone Growth • Bones increase in length (interstitial growth) & width (appositional growth) • Epiphyseal plate: layer of hyaline cartilage in metaphysis of growing bone; new bone forms on diaphysis side • Interstitial growth (length): from epiphyseal plate • Four zones; close around 18-21 (18-females, 21-males) 1. 2. 3. 4. Resting cartilage: nearest epiphysis, anchor plate to bone (not part of growing bone) Proliferating cartilage: cells divide & replace dying cells Hypertrophic cartilage: matruing chondrocytes; arranged in columns Calcified cartilage: cells harden & die; replaced by bone tissue • Osteoclasts dissolve and osteoblasts and blood vessels enter area Interstitial Bone Growth Appositional Bone Growth • Growth in thickness of the bone • Cells in periosteum differentiate into osteoblasts while osteoclasts increase medullary cavity • Osteoblasts in periosteum add bone tissue to external face of diaphysis as osteoclasts in endosteum remove bone from inner surface • Occur at about the same rate Skull or lady in the mirror? Bone Remodeling • Bone resorption & deposition used to renew and replace injured bone • Affected by minerals, vitamins, and hormones • Resorption: removal of minerals and collagen fibers by osteoclasts • Deposition: addition of minerals and collagen fibers by osteoblasts Bone Remodeling • Bones are remodeled continually in response to changes in two factors: 1. Calcium levels in the blood • • • Parathyroid gland releases PTH when blood calcium levels drop PTH activates osteoclasts to break down bone matrix and release Ca2+ into blood Hypercalcemia: Ca2+ is deposited into bone matrix as hard calcium salts 2. Pull of gravity and muscles on the skeleton • • • • • Shape of bone altered for stress Osteoblasts lay down new matrix & become trapped within it (become osteocytes) where bulky muscles attach (due to stress) Bedridden/inactive: lose mass & atrophy (no stress) Ongoing replacement of old bone tissue by new bone tissue PTH determines when/if bone broken down or formed in response to need for more or fewer Ca2+ ions in the blood; stress determines where bone matrix is to be broken down or formed • Helps maintain skeletal strength Bone Fracture Repair • Repair involves four major events: 1. Hematoma forms • From ruptured blood vessels, cells die that are deprived of oxygen 2. Fibrocartilage callus forms • • growth of new capillaries (granulation tissue) into clotted blood at site of damage and disposal of dead tissue by phagocytes. CT cells form mass of repair tissue which splints broken bone and closes gap (made up of bony matrix, collagen, collagen matrix) Bone Fracture Repair 3. Bony callus forms • Fibrocartilage callus is gradually replaced by the bony callus (made of spongy bone) as more osteoblasts and osteoclasts migrate to area and multiply 4. Bone remodeling occurs • Bony callus is remodeled in response to mechanical stresses placed on it Skeletal System Anatomy Bone Markings Can you see the hidden skull? Skeletal System Anatomy 206 total bones Axial Skeleton • Three parts: • Skull • Vertebral column • Thoracic cage Skull: 22 bones • Cranial (8), Facial (13), Mandible (1) • Protects brain • Many paired bones • Page 148-149 • Teeth: 32 in adult (not part of 206 total)considered part of digestive system Skull • Infants have fontanels (soft spots) • Bones of the skull are not fused yet • Adults: skull bones fused with sutures • Immoveable joints • Mandible: freely moving joint link link Middle Ear: 6 bones • Three in each ear • Stapes (stirrup) • Incus (anvil) • Malleus (hammer) Hyoid Bone • Does not articulate with any other bone • Often broken during strangulation • CT attaches to larynx & trachea Vertebral Column: 26 bones • Strong, flexible, rotates • Protects spinal cord & supports head • Intervertebral discs between made of fibrocartilage • Shock absorption & spine flexibility • High in water content when young (spongy, compressible); discs harden with age Vertebral Column: 26 bones • Born with 33 - fuse to 26 • 7 cervical (neck)- smaller, bifed clef • C1: atlas (articulates with occipital condyle) • C2: axis • 12 thoracic (chest)- stronger, long spine • 5 lumbar (lower back)- strongest, short spine • Sacrum (5 fused by mid 20s) • Coccyx (4 fused by 30)- tail bone Vertebral Column: Figure 5-1 Curvatures of the Spine • Four normal curvatures • Fetus has 2 primary curvatures (thoracic and sacral) • Secondary curvatures develop after birth • Cervical (3 months) and lumbar (6 months) • Cervical: concave (anterior) • Thoracic: convex (posterior) • Lumbar: concave (anterior) • Sacrum: convex (posterior) • Exaggeration of the thoracic curve • Tuberculosis of spine• vertebral bodies partially collapse • Degeneration of discs • Rickets (lack of vitamin C) • Poor posture • Advanced osteoporosis • Exaggeration of the lumbar curve •Exaggerated lumbar curve • Result of increased weight gain • Pregnancy or extreme obesity • Poor posture • Rickets • Tuberculosis of spine link • Lateral bending of the vertebral column • Lateral curvature • Congenital malformed vertebrae (birth defect) • Chronic sciatica (pain down leg) • Paralysis of muscles on one side of backbone • Poor posture • One leg shorter than other Thoracic Cage: 25 Bones • Sternum: fusion of 3 bones, attached to first 7 ribs • 12 pairs of ribs (1-7 increase in size, 8-12 decrease in size) • Attached by costal cartilage • True ribs (1-7)- direct attachment • False ribs (8-12)- no anterior attachment • Floating ribs (11-12)- no anterior attachment • All have posterior attachment to vertebrae link Appendicular Skeleton 126 bones: limbs, pectoral & pelvic girdles (attach limbs to axial skeleton) Pectoral Girdle: 4 bones • Attach arms; two of each • Clavicle: collar bones • s-shaped- weak juncture • Attaches to manubrium and sternum medially and scapula posteriorly to form shoulder joint • Prevents dislocation • Scapula: shoulder bones link Upper Limbs: 60 bones • 8 carpals each • 5 metacarpals • 14 phalanges • 2 in thumb • Radius (thumb side) • Ulna (pinky side) 1. Clavicle 1a. Sternal end 1b. Acromial end 2. scapula 2a. Coracoid process 2b. Acromion 2c. Subscapular fossa 2d. Infraspinous fossa 2e. Spine of scapula 2f. Supraspious fossa 2g. Glenoid cavity 3. Acromioclavicular 4. Glenohumeral joint 5. Humerus 5b. Deltoid tuberosity 5c. Head 5d. Surgical neck 5e. Anatomical neck 5f. Greater tubercle 5g. Lateral epicondyle 5h. Medial epicondyle 5i. Capitulum 5j. Trochlea 5k. Coronoid fossa 6. Ulna 6a. Olecranon 7. Radius 1. Phalanges 1a. Distal 1b. Medial 1c. Proximal 1d. Base 1e. Head 2 Interphalangeal joints 3 Sesamoid bone 4 Metacarpophalangeal joints 5 Intermetacarpal joints 6. Metacarpals 6a. Base 6b. shaft 6c. Head 7. Carpometacarpal joint 8. Trapezium 9. Trapezoid 10. Capitate 11. Hamate 12. Pisiform 13. Triquetrum 14. Lunate 15. Scaphoid 16. Midcarpal join • median nerve which runs through wrist to hand becomes compressed • involves narrow bony passage in wrist called carpal tunnel, through which nine tendons and median nerve must pass Pelvic Girdle: 2 bones • Function: bearing weight (total weight of upper body) & protects reproductive and urinary systems • United at pubic symphysis (fibrocartilage; some flexibility) • Attached to axial skeleton via sacral attachment to lower lumbar vertebrae • Three parts fuse at birth • Ilium • Pubis • Ischium •Femur, tibia, fibula, patella •7 tarsals, 5 metatarsals, 14 phalanges •Carry our total body weight when erect •much thicker/stronger than upper limbs Lower Limbs: 60 bones 1. Hip joint 2.Femur 2a. Head 2b. Neck 2c. Greater trochanter 2d Lesse trochanter 2e. Lateral epicondyle 2f. Medial epicondyle 2g. Adductor tubercle 2h. Medial condyle 2i. Lateral condyle 2j. Intercondylar fossa 2k. Linea aspera 3. Patella 4. Knee joint 5. Tibia 5a. Lateral condyle 5b. Medial condyle 5c. Tibial tuberosity 5d. Medial malleolus 6. Fibula 6a. Head 6b. Crest 6c. Lateral malleolus 7. Ankle joint 8 Talus 9. Calconeus • Bones composing arch of foot held by ligaments and tendons • Weakened ligaments and tendons causes arch to “fall” • Caused by excessive weight, postural abnormalities, weakened tissue, and genetic disposition Name those bones Male vs. Female • Males bones larger and heavier • Angle of pubic symphysis less for men • Page 163 lists differences Fetal Skeleton • Arises from mesenchymal cells (derived from mesoderm) • Intramembraneous and endochondral ossification • 1st long bones = hyaline cartilage • 1st flat bones of skull = fibrous membranes • 20 million people suffer from it (250,000 hip fractures a year) • Decreased bone mass • Increased susceptibility to fracture • Hormones effect osteoblast production • Afflicts entire skeletal system • Body build (shorter females at greater risk) • Weight (adipose produces estrone) • Smoking (decreases estrogen levels) • Calcium deficiency or malabsorption • Vitamin D deficiency • Exercise (sedentary more at risk) • Certain drugs (alcohol, diuretics, cortisone, tetracycline) • Premature menopause • Family history • Accelerated remodeling of bone tissue • Osteoclast resorption massive • Osteoblast formation extensive • Irregular thickening and softening of bones • Greatly increased vascularity, especially in skull, pelvis, and extremities Testicular tumor “face”