Hematopoietic and lymphoid systems
advertisement

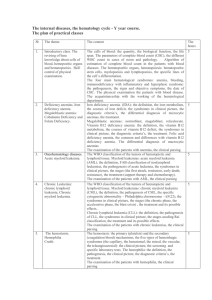
Hematopoietic and lymphoid systems • main entities - disorders • exam questions and very concise text - www.lfhk.cuni.cz/patanat Hematopoietic and lymphoid systems - exam questions • • • • • • • • • • • • • • • • Posthemorrhagic and hemolytic anemias Anemias of diminished erythropoiesis; pernicious anemia Polycythemia Bleeding disorders DIC Lymph node pathology - review Spleen pathology - review Thymus pathology - review Non-Hodgkin’s lymphomas Hodgkin’s disease Acute leukemias Chronic leukemias Myeloproliferative disorders Plasma cell dyscrasias Histiocytoses Storage diseases Anemia - causes • posthemorrhagic • hemolytic • impaired red cell production Blood loss posthemorrhagic anemias • acute - hypovolemia, shock, rapid hemodilution, slowly increasing hematopoesis (sufficient amount of iron) • chronic - GIT, female genital tract iron loss (increased hematopoesis) Hemolytic anemias - general features • • • • increased rate of RBCs destruction increased amount of iron hypercellular bone marrow reticulocytes in peripheral blood Hemolytic anemias - RBCs destruction • intracorpuscular (intrinsic) hereditary, acquired are rare • extracorpuscular (extrinsic) acquired, immunity, mechanical trauma, infections Intracorpuscular anemias • hereditary • acquired Hereditary • • • • spherocytosis sickle cell anemia thalassemia - T. maior, T. minor glucose-6-phosphate dehydrogenase deficiency Acquired • paroxysmal nocturnal hemoglobinuria Extracorpuscular anemias • immunity related • mechanical trauma • infections Immunity related • autoimmune anemias • Erythroblastosis fetalis (hemolytic disease of the newborn) - related mainly to Rh system (D- antigen), less to AB0 systém. Passage of fetal RBCs through the placenta during last trimester (no cytotrophoblast) or during childbirth. Mother antibodies cross the placenta. • Concurent AB0 incompatibility protects the mother against Rh immunization - RBCs removed from maternal circulation. The blood dose - 1 ml. IgG response - cross the placenta, IgM - does not cross, the response faster in 2nd or 3rd gravidity (faster IgG response). Mechanical trauma • prostethic valves - more in metallic or plastic prostheses than in bioprostheses • microangiopathic hemolytic anemia squeezed RBCs in narrowed vessels - DIC, SLE, malignant hypertension Infections • malaria - 4 subtypes of plasmodia, Asia, Africa - Anopheles (mosquito) • Plasmodium falciparum - malignant tertian malaria Anemias of diminished erythropoiesis • lack of – iron – folic acid – vitamin B12 – less frequently - pyridoxin, thiamin Iron deficiency anemia (sideropenic) • lack of iron in the food - veggies; malabsorption - sprue • increased demand - gravidity • chronic loss - GIT, menstrual bleeding • morphology - microcytosis, low RBCs volume, pallor, spoon-shaped nails Folic acid and vitamin B12 (Cobalamin) deficiency anemia (megaloblastic) • folic acid deficiency - gravidity, severe alcoholics, drug abusers. Sometimes celiakia, malabsorbtion. • B12 - like folic acid deficiency, in addition - peripheral nerves and spinal chord demyelinization Aplastic anemia • pancytopenia, erythrocytopenia, agranulocytosis, thrombocytopenia • in half number of cases - idiopatic • sometimes after irradiation, myelotoxic drugs Myelophtisis • bone marrow metastases - breast, lungs, prostate • multiple myeloma, TBC Bleeding disorders hemorrhagic diatheses • vascular fragility - vitamin C deficiency - scurvy • DIC, thrombocytopenia, coagulopathies DIC • Blood clotting - starts from soft tissue (tissue thromboplastin) or endothelial damage (factor XII.) • Causes: 1/ release of clotting factors amniotic fluid embolization, cytoplasmic granules - promyelocytic leukemia, mucus - Ca, Gram-negative sepsis 2/ extensive endothelial damage, burns, SLE DIC - morphology • fibrin microthrombi within capillaries - kindeys, brain, heart, lungs, adrenal gland (Waterhouse - Friderichsen sy), hypophysis (Sheehan sy) • acute DIC - bleeding, chronic thrombotic Thrombocytopenia • Idiopathic thrombocytopenic purpura (ITP) • Thrombotic thrombocytopenic purpura (TTP) (m. Moschowitz) microthrombi composed of platelets Coagulation disorders • acquired - prothrombin, f. VII., IX., and X. - hepatic damage • hereditary • hemophilia A • hemophilia B Leukemias • leukemic form • aleukemic form • leukemic infiltration of the liver, spleen, lymph nodes • primary site - bone marrow Leukemias - classification • maturation: • acute leukemias • chronic myeloproliferative disorders • cell types: • lymphatic • myeloid Acute leukemias • clinical course – sudden onset – anemia, fever, infections, hemorrhagic diathesis – bone pain (bone marrow expansion) – generalized lymphadenopathy (ALL), splenomegaly, hepatomegaly – CNS symptoms - headache, vomitus, paralysis ALL (acute lymphoblastic leukemia) • 80 % of childhood leukemias • 5 - 10 % Philadelphia chromosome (22 9) • prognosis - relatively good, 90 % remission, if translocation worse prognosis AML (acute myeloid leukemia) • adult middle age • prognosis bad, 5-year survival - 10 15 % • hiatus leukemicus • bone marrow transplantation Chronic myeloproliferative disorders • • • • • CML CLL polycytemia vera HCL myeloid metaplasia with myelofibrosis • essential thrombocytemia CML (chronic myeloid leukemia) • adults middle or younger age • “pyoid” bone marrow • Philadelphia chromosome - 90 % patients • bad prognosis CLL (chronic lymphatic leukemia) • older age • long asymptomatic period, noncharacteristic symptoms • course and prognosis variable • related to malignant lymphomas Polycytemia vera • proliferation of erythroid, myeloid and megakaryocytic line • increased blood viscosity, blood volume • borne marrow highly cellular • hypertension, thromboses, bleeding Hairy cell leukemia • chronic B-cell line leukemia • fine cytoplasmic projections immunohistochemistry, phase contrast, EM • hepatomegaly, splenomegaly • therapy - purine analogues Myeloid metaplasia with myelofibrosis • bone marrow fibrotic, hypocellular • neoplastic stem cells within the spleen • unknown ethiology of bone marrow fibrosis • splenomegaly, trilinear hematopoiesis in the spleen, prominent megakaryocytes Leukemias - general morphology • • • • • bone marrow soft - “pyoid” (CML) splenomegaly - CML lymph nodes enlargement - CLL hepatomegaly - CML, CLL sometimes other organs infiltrated Non-neoplastic white cells disordes • leukopenia - neutropenia (agranulocytosis) – impaired granulopoiesis - bone marrow failure – destruction of granulocytes - immunity, drugs • reactive leukocytosis - infections • infectious mononucleosis - EBV Plasma cell dyscrasias • • • • • • multiple myeloma localized plasmacytoma Waldenström’s macroglobulinemia heavy-chain disease primary amyloidosis monoclonal gammopathy of undetermined significance Multiple myeloma morphology • osteolytic lesions - prominent mainly in the scull • histologically - diffuse infiltration by neoplastic plasma cells • kidney - myeloma nephrosis neoplastic plasma cells, casts within distal tubules Histiocytoses X • acute disseminated Langerhans’ cell histiocytosis (Letterer - Siwe) • unifocal and multifocal - eosinophilic granuloma • multifocal histiocytosis (HandSchüller-Christian disease) Malignant lymphomas • non-Hodgkin’s lymphomas • Hodgkin’s lymphoma Non-Hodgkin’s lymphomas • nodular • diffuse • Working Formulation, Kiel Classification, REAL, WHO Malignant lymphomas some entities • • • • ML of CLL type follicular centre ML diffuse large cell ML Burkitt’s lymphoma Extranodal ML • mycosis fungoides • Sézary’s syndrome • MALToma Hodgkin’s ML • nodular lymphocyte predominance Hodgkin’s lymphoma • classical Hodgkin’s lymphoma – lymphocyte rich – nodular sclerosis – mixed cellularity – lymphocytic depletion Hodgkin’s ML - staging • I. Single lymph node region or single extralympatic organ. • II. Two or more lymph node regions or limited contiguous extralymphatic organ on the same side of diaphragm. • III. Two or more lymph node regions or limited contiguous extralymphatic organ on both sides of diaphragm. • IV. Multiple, disseminated foci of involvement, both sides of diaphragm + bone marrow. Lymph nodes -nonneoplastic diseases • reactive lymphadenitis – acute non-specific – chronic non-specific • speciphic lymphadenitis – TBC (BCG) – Cat Scratch Disease Spleen - overview • enlargement – massive – moderate – mild • rupture • necrosis Thymus - overview • thymic hyperplasia • tumors • thymoma » benign thymoma - 90 % » thymic carcinoma Thymomas • epithelial predominance • lymphocyte predominance • mixed • appendant disease - myasthenia gravis