Differentiating Trigeminal Neuropathy From Trigeminal Neuralgia
advertisement
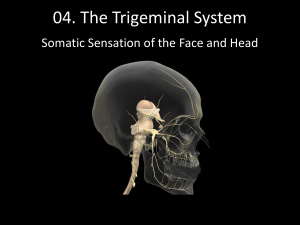
Differentiating Trigeminal Neuropathy From Trigeminal Neuralgia Does It Even Matter? Justin Sandall, D.O. Vanderbilt University Medical Center Department of Anesthesiology, CA-2 Case Presentation 26 y/o female w/a history of chronic migraine HA, depression and hypothyroidism presents for evaluation of L sided facial pain. She relates a history of migraines since the age of 11; occurred infrequently until beginning college in 2001 at which time they increased in frequency to 2-3x/month. ~1 year ago she had her typical migraine which "didn't go away." She now has a constant, throbbing/boring pain in her L periorbital/frontal area with occ. radiation to the L maxilla. She also has intermittent sharp, lancinating pains in those same areas. Her pain is worsened with anxiety, working out, loud noises, heat and alleviated with application of cold, migraine medications and Lyrica. Mother has noticed L sided facial swelling. There is no association with brushing teeth, putting on makeup or wind on the face. She denies changes in hearing, balance or coordination. She also denies sensory changes, tearing, conjunctival effusion and ataxia. No h/o trauma or HSV. Case Presentation MEDICATIONS: - Synthroid Oral Tablet 75 mcg 1 tablet by mouth daily - Betaxolol 10mg PO twice daily - Zoloft 150mg PO daily - Migrelief 2 tabs PO - Topamax 300mg OP daily - Ondansetron tab PO PRN - Indomethacin 25mg PO twice daily - Zomig Zmt 5mg PO twice daily - Lyrica 300mg - Kariva BC - Zyrtec 10mg Case Presentation Relevant PERRL, CN II-XII intact b/l, NTTP along trigeminal distribution w/o allodynia or hyperesthesia, no sensory deficits, TMJ NTTP b/l Relevant Physical Exam Imaging Previous work-up including CT and MRI unrevealing Trigeminal Neuralgia Most common pain syndrome referable to a cranial nerve.1 Most common in adults > 50 y/o, women slightly more than men2 Classically, pain is described as an electric shock–like, stabbing, unilateral pain with abrupt onset and termination in distribution of trigeminal nerve – usually V2/3.2,3 Intervals between attacks are pain free Minimal or no sensory loss in the region of pain Precipitation from trigger areas or by certain daily activities, such as eating, talking, washing the face, or cleaning the teeth3 Diagnosis is typically made by the history Imaging is often pursued to r/o other causes of facial pain &/or to evaluate for MS, vascular compression of the trigeminal nerve etc. Typically, 80% of patients respond to medical therapy3 1st line therapy is carbamazepine2,3,5 Trigeminal Neuralgia May target trigeminal nerve at various sites with nerve blocks if unresponsive to medical therapy Superficial V1/V2, gasserian ganglion If responsive to local anesthetic block, may pursue trigeminal neurolysis Most common target is the gasserian ganglion via the foramen ovale1 Studies have all used patients w/classic trigeminal neuralgia • Less premorbid depression/anxiety, more satisfied w/outcome, fewer side effect complaints, more willing to repeat procedure1 Study by Taha and Tew in 1996 evaluated RF rhizotomy w/curved electrode, RF rhizotomy, glycerol rhizotomy, balloon compression, and posterior fossa exploration (microvascular decompression, partial trigeminal rhizotomy)4 • Showed initial pain relief to be 91-98% with success of procedure in 85-98% and pain recurrence in 15-54% Glycerol rhizotomy had lowest initial pain relief, lowest procedure success and highest pain recurrence Complications of trigeminal neurolysis can be devastating and include anesthesia dolorosa, loss of corneal sensation, keratitis, dysesthesia1 Trigeminal Neuropathy (included atypical trigeminal neuralgia and atypical facial pain) Chronic or recurrent pain in the area of previous nerve injury, numbness, dysesthesias, and chronic burning sensations. Diagnostic evaluations rule out any other cause of pain.2 Doesn’t meet White and Sweet criteria:2 The pain is paroxysmal. The pain is confined to the trigeminal distribution. The pain is unilateral. The bedside clinical sensory examination is normal. The pain may be provoked by light touch to the face (trigger zones) Significant clinical challenge because the symptoms of PTN respond poorly, if at all, to AED or surgical therapies commonly used in TN.1,2 More likely to have sensory loss or allodynia5 Neurolytic treatment may actually worsen pain in this subgroup More often associated with young, middle aged women and feelings of depression Motor cortex stimulation for trigeminal neuralgia seems promising – 70% success rate compared to 50% for central pain5 Classic trigeminal neuralgia Rare Intraoral or extraoral in trigeminal region Each episode of pain lasts for seconds to minutes; refractory periods, and long periods of no pain Sharp, shooting, moderate to very severe Light touch provoked (e.g., eating, washing, talking) Discrete trigger zones Atypical trigeminal neuralgia Rare Intraoral or extraoral in trigeminal region Sharp attacks lasting seconds to minutes, more continuoustype background pain, less likely to have complete pain remission Sharp, shooting, moderate to severe but also dull, burning, continuous mild background pain Light touch provoked, but continuoustype pain not so clearly provoked May have small trigger areas, variable pattern Trigeminal neuropathy Very rare Trigeminal area, but may radiate beyond Continuous Dull with Areas of sharp allodynia, exacerbation light touch Sensory loss, subjectiveobjective, progressive, vasodilation and swelling may occur Adapted from Essentials of physical medicine and rehabilitation: musculoskeletal disorders, pain, and rehabilitation/ [edited by] Walter R. Frontera, Julie K. Silver, Thomas D. Rizzo Jr.—2nd ed. Chapter 90. Case Resolution 26 y/o female with L sided facial pain in the setting of chronic migraine HA, h/o depression and hypothyroidism. Given the nature of her pain, her history of depression and migraine HA, her pain triggers or lack thereof and physical exam findings, this most likely is atypical facial pain secondary to trigeminal neuropathic pain in the V1/V2 distribution rather than classic trigeminal neuralgia. It is important to make this distinction given that definitive treatment of trigeminal neuralgia (i.e. neurolytic tx) can actually worsen the pain of trigeminal neuropathy. In addition, she almost certainly has a component of transformed migraine HA that is contributory thus one of our long-term goals will be to decrease the number of medicines she is on. 1. Atypical facial pain 2. Trigeminal neuropathic pain in the V1V2 distribution 3. Transformed migraine headache 4. H/o depression 5. Hypothyroidism Will schedule for superficial V1/V2 block and TPI and assess response. Needs to be off indomethacin x7 days prior to procedure. May benefit from Gasserian ganglion block and/or Stellate ganglion block down the road if not responsive to more conservative measures. If responds well to the peripheral n. blocks, will use Botox for long-term control. Meanwhile References Jackson T, Gaeta R: Neurolytic blocks revisited. Current Pain and Headache Reports. 2008, 12:7-13. Raj's practical management of pain/editors, Honorio T. Benzon…[et al.].—4th ed. Chapter 25. Essentials of physical medicine and rehabilitation: musculoskeletal disorders, pain, and rehabilitation/ [edited by] Walter R. Frontera, Julie K. Silver, Thomas D. Rizzo Jr.—2nd ed. Chapter 90. Taha JM, Tew JM: Comparison of surgical treatments for trigeminal neuralgia: reevaluation of radiofrequency rhizotomy. Neurosurgery 1996, 38:865-871 McMahon: Wall and Melzack's Textbook of Pain, 5th ed. Chapter 37