Click to
advertisement

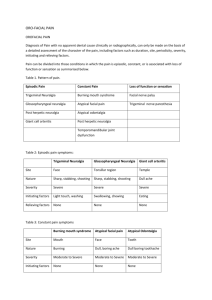
Oro-Facial Pain By Iain Macleod What is Pain? • “Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage” • “- pain is always subjective -” Int. Assoc. for the Study of Pain Oro-Facial Pain • The remit of the dentist? • Patients go to dentist to get problem fixed – Filling, extraction etc • Problem arises when dentist can’t fix it! • Patients don’t go to dentist for medical/psychological help! • Dentist under pressure to do something! • Poor inter-professional communication between medicine and dentistry • Dentists often isolated Oro-facial Pain • Oro-facial pain can be difficult to diagnose! • TMD can be a great mimic! • Beware of referred pain! Causes of facial pain • Many causes! • May be infectious, neurological, vascular oncological or psychogenic In the primary care setting how much do each of the following contribute to the diagnosis? • • • • • • • History taking >80% Physical examination <10% Investigations <10% So why do we do so many investigations? Why Do We Order So Many Tests? • "Defensive" medicine in an increasingly litigious environment • Loss of confidence in our abilities to extract meaningful information from the history and examination Consequences of Ordering So Many Tests – Time delay in diagnosis as one awaits the test results – The patient is exposed to the risk and side effects of tests that may not be necessary The pain history • Onset, location and duration of facial pain • Alleviating or aggravating factors • Medical, dental & social history KEY QUESTIONS • • • • IS THE PAIN PRESENT EVERY DAY ? WHAT IS A NORMAL DAY LIKE ? HOW SEVERE IS THE PAIN ? – (Score 0-10) Rules of Thumb! • Dental pain gets better or worse! • Chronic pain is rarely dental! • If an experienced dentist “feels” the pain is not dental they are most often right ! 5th & 7th Cranial Nerves 1. Sensory root of trigeminal nerve 2. Pons 3. Vestibulocochlear nerve 4. Facial nerve 5. Abducent nerve 6. Medulla oblongata 7. Motor root of trigeminal nerve 8. Basilar sulcus Nasopharyngeal Carcinoma (Trotter’s Syndrome) • Maxillary pain – With numbness!! • Unilateral nosebleeds Toothache Dental caries Dental Pain - radiation • Caries in mandibular molars can produce pain around the ear • Caries in maxillary teeth can produce maxillary, orbital, retro-orbital Dental Pain • Dental pain can be difficult to diagnose! – Tooth sleuth! – Hot water test! • TMD can be a great mimic! – Headaches, jaw pain, toothache etc.! • Beware of referred pain – sinuses, cervical spine, heart etc.! Acute Maxillary Sinusitis • Unilateral or bilateral pressure, fullness or burning pain over cheekbone, upper teeth and around eyes • Exacerbated by stooping • Usually follows an URTI • Most cases self limiting Chronic Maxillary Sinusitis • Feeling of pressure below the eyes or toothache • Computed Tomography • Endoscopy Sinusitis Management • • • • • • • • Decongestants Steam inhalations Antibiotics if indicated Local Heat Antihistamines if allergic component corticosteroids Sinus irrigation Endoscopic surgery TEMPOROMANDIBULAR JOINT DISORDERS • Common • More has been written about this topic than for any other joint ! • Various classifications • Many cases are self limiting • Surgery is indicated in very few BUT important exceptions Temporomandibular Dysfunction • Pain in the joint and/or surrounding muscles • Joint “clicking” • Periods of limitation of joint movement (trismus) EPIDEMIOLOGICAL DATA • Percentage of population with signs 50-75% • Percentage of population with symptoms 20-25% • Percentage of population who seek treatment 3-4% Temporomandibular Dysfunction • Causes • Parafunction – Bruxism – Clenching • Emotional stress • Predisposition (F>M) – Joint hypermobility • Occlusal factors – little evidence Bruxism • • • • • Tooth wear Painful teeth Cracked cusps Mouth ulcers due to trauma Jaws ache in the morning Temporomandibular Dysfunction • • • • • • • • Pain distribution Variable – a great mimic!! Joint pain Earache Toothache Facial pain Headache Can be associated with neck and shoulder pain Treatment of TMD Trigeminal Neuralgia - Description • A painful unilateral affliction of the face, characterized by brief electric shock-like (lancinating) pains limited to one or more divisions of the trigeminal nerve • Pain evoked by washing, shaving, smoking, talking, brushing, air blowing, or spontaneously occurring • Pain is abrupt in onset and may remit for varying periods Trigeminal Neuralgia • Subclassified into idiopathic and symptomatic • Idiopathic trigeminal neuralgia: due to an interaction between trigeminal nerve and vasculature • Symptomatic trigeminal neuralgia: caused by demonstrable structural lesion Trigeminal Neuralgia • Females > males • Usually elderly – (if < than 40 -?MS) • Restricted to Vth nerve – Similar can affect IXth nerve – glossopharyngeal neuralgia • Trigger point – may bear no anatomical relation to site of pain but on same side! • Sleep often not affected • May go into remission Trigeminal Neuralgia Diagnosis: • History • Examination • MRI – aberrant pontine blood vessel? – exclusion of other cause (neoplasm, MS) • (Response to trial of carbamazepine) Trigeminal Neuralgia Treatment: • Medical – anticonvulsants ( e.g. carbamazepine) – needs medical monitoring! • Use of additive drugs – e.g. baclofen • Damage to trigger point – alcohol injection, cryotherapy Trigeminal Neuralgia – Surgical Treatment • Radiofrequency ganglionolysis • Microvascular decompression Establishment of VZV Latency in Sensory-Nerve Ganglia. After a primary VZV infection (chickenpox), latent VZV infection is established in the dorsal-root ganglia, and zoster occurs with subsequent reactivation of the virus N Engl J Med Vol 356(13) P1338-1343 Zoster: Clinical Features • Usually limited to 1 or 2 adjacent, unilateral dermatomes • “Grape-like” lesions clustered on an erythematous base • Lesions usually heal within 4 weeks1 Post Herpetic Neuralgia • Burning, itching, prickly pain that worsens with contact or movement • Persists along any of the three trigeminal nerve distributions affected by shingles • Difficult to treat! • Importance of adequate treatment of shingles – especially the elderly • Carbamazepine, tricyclics Giant Cell Arteritis • Over 50yrs,women>men • recent onset headache,scalp tenderness • Jaw/tongue claudication (tired tongue/jawache) • anorexia • visual disturbances • Swollen disc usually GCA Diagnosis • ESR/CRP • BP, CXR • Biopsy of temporal artery Treatment of GCA • Give corticosteroids immediately in all suspected cases • Start with 1mg/Kg prednisolone daily with vitamin D and calcium supplements. • Refer for Ophthalmology Psychogenic Somatisation Disorders Somatisation has been defined as “the expression of personal and social distress in an idiom of bodily complaints with medical help seeking” Common ! “In general medical practice, somatisation associated with psychiatric illness accounts for 20 - 30% of all consultations” DEPRESSIVE ILLNESS Warning Signs • Persistent low mood (> 2weeks) • Feeling worthless, hopeless, suicidal • Loss of interest in usual activities – anhedonia • • • • Fatigue Poor concentration Reduced sleep Poor appetite Atypical Pain Conditions • • • • Atypical = poorly understood! Often regarded as purely “psychogenic”! But chronic pain will make you depressed! Other factors may be involved! – There may be a cause? – Patient may just be a poor historian! • Be careful of labels! • Keep an open mind! “Atypical” Facial Pain Conditions • Persistent idiopathic facial pain • Persistent dento-alveolar pain (atypical odontalgia) • Oral dysaesthesia • Phantom bite syndrome • (TMD) • Syndrome of bizarre oro-facial symptoms Persistent Idiopathic Facial Pain • • • • • • • • • Middle aged or older Mainly female Constant pain / discomfort Poorly localised May cross midline Does not waken patient from sleep Lack objective signs Investigations (-ve) Other symptoms (headaches,IBS,backache etc.) Persistent Idiopathic Facial Pain • Demand physical treatment • Often do not accept psychological explanation • May have seen several specialists/practitioners • May be obsessed with symptoms Psychogenic Toothache • Patient reports that multiple teeth are often painful with frequent change in character and location • A general departure from normal or physiological patterns of pain • Patient presents with chronic pain behaviour • Lack of response to reasonable dental treatment • Unusual or unexpected response to therapy • No other identifiable pain condition that can explain the toothache Non-Odontogenic Toothaches Warning Symptoms- Summary • Spontaneous multiple toothaches • Inadequate local dental cause for the pain • Stimulating, burning, non-pulsatile toothaches • Constant, unremitting, non-variable toothaches • Persistent, recurrent toothaches • Local anesthetic blocking of the offending tooth does not eliminate the pain • Failure of the toothache to respond to reasonable dental therapy Chronic Orofacial pain Burning mouth syndrome is characterized as a burning, tender, or annoying sensation in the mouth with no apparent mucosal lesion. Descriptive symptom Late middle age – elderly Female>Male Burning Mouth Syndrome (glossodynia, glossopyrosis) • Possible causes • Haematinic deficiency – Fe, B12, Folate • • • • • • Diabetes melitus Candidosis Dry mouth Denture problems Parafunctional Psychogenic – Anxiety • Cancerophobia+++ – Depression Management – What You Should Do! • History ( what’s the story in detail ) – Exacerbants, alleviation, associated features • Exclude organic disease • Be aware of emotional state – Depression / anxiety (HAD score) - Secondary gain – what benefits does the patient get from being unwell? • Life events – connections with onset etc. • Discuss with GMP (with patients consent) • Decide on need for medication / referral Management – What You Should Do! • Remember the patients pain is real even if a physical cause can not be found – tact! • Allow the patient to express themselves – What do you understand about your pain? – What do you feel it represents? – Cancer phobia? • It can take time • Remember most complaints are regarding communication – or lack of it! Management Strategies The Pain Clinic • Medical – drugs – alter the chemical soup! • Surgical – nerve ablation procedures e.g. for cancer pain • Physiotherapy – improving activity • Clinical Psychology – living with the problem – Cognitative, Behavioural Therapy (CBT) Pain Management is multidisciplinary! Liaise closely with the GMP Take-Home Points • • • • Oro-facial pain is common Most cases are dental Diagnosis can be very difficult Patients are frequently frustrated & very distressed by time they reach secondary care • Need a lot of listening too! Conclusions • Careful history taking is essential to correctly diagnose facial pain • Remember the anatomy of the trigeminal nerve • Many facial pain syndromes are wrongly attributed to disease of the teeth or sinuses