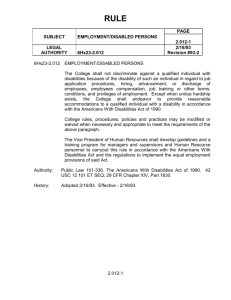
original PowerPoint - Community Rehabilitation and
advertisement

Ethics of Working with Individuals with Disabilities and their Families in Maintaining Health Dick Sobsey University of Alberta 1 A Father’s Perspective • MECP2 Duplication Syndrome • Diagnosis at Age 18 • In general, our family’s experience has been positive and supportive. 2 • ER, University Hospital, Edmonton • ER, Rockyview Hospital, Calgary • ER, Taber Hospital • ER, Vancouver General • ER, Vancouver Children’s • ER, Anaheim Memorial • Urgent Care, Dunedin, NZ • Urgent Care, Queenstown, NZ • Urgent Care, Brisbane, Australia • Suva Hospital, Fiji • Navua Health Clinic, Fiji A Father’s Perspective 3 Disparities Health Outcome Disparities • May be due to impairment or disease process. • May be due to unequal treatment Health Care Disparities • Differences in health care access and quality of health services. 4 United States Havercamp, Scandlin, & Roth. (2004). Health Disparities Among Adults with Developmental Disabilities, Adults with Other Disabilities, and Adults Not Reporting Disability in North Carolina. Public Health Reports, 119, 418-426 Never had Pap Test Adult Females Never had mammogram Females over 40 No Teeth Cleaning for more than 5 years No Disability Other Disability Developmental Disability 2.2 4.7 11.5 13.0 14.5 26.8 8.0 17.2 14.4 5 United States • Racial and ethnic disparities in the use of health care have attracted the greatest public and Congressional notice. Nevertheless, another large subgroup of Americans—the 40 to 50 million individuals with disabilities—experience similar disadvantages while generating little public outcry. • Disparities monitoring is only a first step to eliminat- ing harmful inequalities in health service use across populations. The next more important step is understanding reasons for these disparities and eliminating barriers to equitable use of health care. • Tracking disability disparities: the data dilemma • Journal of Health Services & Research Policy. 13(3):12930, 2008 Jul Iezzoni, Lisa I. 6 United States • Although 82.2% of nondisabled persons had surgery, 68.5% of disabled persons received operations. Adjusted relative risks (RRs) of receiving surgery were especially low for persons with respiratory disabilities (adjusted RR=.76), nervous system conditions (adjusted RR=.86; 95% CI, .76– .98), and mental health and/or mental retardation disorders (adjusted RR=.92; 95% CI, .86–.99). Persons with disabilities had significantly higher cancer-specific mortality rates (hazard ratio [HR]=1.37) than persons without disabilities. Observed differences in cancer mortality persisted after adjusting for demographic and tumor characteristics (adjusted relative HR=1.23). • Iezzoni, L.I. et al. (2008). Treatment Disparities for Disabled Medicare Beneficiaries With Stage I Non-Small Cell Lung Cancer. Archives of Physical Medicine and Rehabilitation, 89, 595-601. 7 Taiwan • After adjusting for age, gender, ethnicity, socioeconomic status and hospital characteristics, the presence of schizophrenia was associated with a 2.83 times higher risk of having a ruptured appendix. • Tsay, J-H.. Lee, C-H,. Hsu, Y-J., Wang, P-J., Bai, Ya-Mei., Chou, Y-J., & Huang, N. (2007)Disparities in appendicitis rupture rate among mentally ill patients. BMC (BioMed Central) Public Health. 7, 331-340. 8 United Kingdom Mencap Reports • Treat me right, 2004 • Poor access to GPs • Poor Treatment in hospitals. • Blatant discrimination cases • Death by Indifference, 2008 • “Senior management within the Department for Health, strategic health authorities, hospital trusts and primary care trusts see people with a learning disability as a low priority” • “Many healthcare professionals do not understand much about learning disability” 9 United Kingdom Healthcare for All, 2008 (Michael Report) • “People with learning disabilities find it much harder than other people to access assessment and treatment for general health problems.” • “insufficient attention given to making reasonable adjustments to support the delivery of equal treatment…” • “Health service staff, particularly those working in general healthcare, have very limited knowledge about learning disability.” • “…witnesses described some appalling examples of discrimination, abuse and neglect across the range of health services “ 10 Canadian Perspectives • “As a group people with DD have poorer health and greater difficulty accessing health care than those in the general population.” • Sullivan et al. Consensus guidelines for primary health care of adults with developmental disabilities. Canadian Family Physician 2006 11 Canadian Perspectives • “Across Canada, there have been insufficient advances in clinical training and service developments to meet the needs of individuals with disabilities and comorbid mental health disturbances” • Lunsky & Bradley. (2001) Developmental Disability training in Canadian residency psychiatry programs. Canadian Journal of Psychiatry • “There are no attractive career paths for health professionals prepared to consider a vocation that emphasizes service to persons with developmental disabilities” • Hennan, B. (2005). Gaps and silos: Persons with developmental disabilities move to the community: University of Manitoba Department of Family Medicine. 12 Canadian Perspectives • “The value society has placed on persons with ID has contributed to disinterest in understanding the various etiologies of ID and their health consequences, which has led to inadequate access to needed care.” • Ouellette-Kuntz, Addressing health disparities through promoting equity for individuals with intellectual disability. Canadian Journal of Public Health 2005 13 Some problems • Pandemic Triage Protocol • Poor access to consistent primary care • Quality of life issues – About 15% of infants who die in hospital are viable infants but treatment is withheld or withdrawn because they are considered not to have adequate potential quality. • Issues in prenatal diagnosis and counseling 14 Symptom Masking Diagnostic Overshadowing • The individual’s’ disability becomes the reason for every issue and routing diagnostic and treatment procedures are overlooked. • It is essential to begin with the same diagnostic and treatment assumptions that are typical for other patients. 15 Limited Communication • Symptoms are typically described by the patient. • Signs are measured directly by observer. • Patients with limited communication require increased reliance on objectively reliable signs. 16 Increased Time Requirements • Many people with disabilities require more time for the same health care procedures. • This creates financial disincentives in a “payby-procedure” system. • “Difficult cases” may result in poor utilization and outcome evaluation data. 17 Specialized Equipment Needs • For example, examination tables are rarely accessible making routine examinations difficult or impossible 18 Ghettoization • When some health services actually make people with disabilities welcome and strive to provide services, they are often oversubscribed by patients who are unwelcome or provided with substandard treatment elsewhere. 19 The Deaf Woman & The Red Cockaded Woodpecker • Dubner & Levitt 20 Jan 2008 NY Times • When do the requirements of providing good services result in maneuvers intended to avoid any services at all? 20 Perfectionism & REhabilitation • Rehabilitation Medicine was deeply rooted in restoring people particularly survivors of war to their pre-injury state. The goals for people who had no pre-injury status or who could not be “restored” were less clear. • Eradication of conditions is often conflated with eradication of people who had the condition. 21 Self-Fulfilling Outcome Prophecy Expect poor outcome Withhold treatment Get poor outcome 22 Difficult Consent Issues • The major focus of current ethical discourse is on Autonomy rather than upon beneficence or preventing harm. • The application of the principle of autonomy to people who may not be apple to fully understand the implications of their choices is difficult. 23 Pediatrics to Adult Services • Although pediatric services are far from adequate, children with disabilities are much better served than adults with disabilities. 24 The Magic Bullet • The idea that we will discover a miraculous prevention or cure diverts too much effort away from supportive treatments that make better lives. 25 Already Use More than Their Share • Many people with disabilities have serious health issues. • What would the impact be if we tried to treat everyone. • Baby Doe • Candace Taschuk • Annie Farlow 26 Everyone is in the same boat.. Well… sort of… • When we are all experiencing the same problems such as difficulty in accessing primary or emergency care… it is difficult to focus on the specific needs of small subpopulations.. • We are all feeling the pinch but these problems disproportionately impact some people. 27 The Will to Change • Change will occur only when key stakeholders believe that this is important. • Many stakeholders agree that there is a problem, but it doesn’t seem to be very high on anyone’s priority list. • Some issues may be difficult but others could be easily resolved. 28 Primary Care Networks & Group Practice Can Help • It is important to ensure that the development of primary care networks include provisions for individuals with complex needs. 29 Nurse Clinicians Can Play an Essential Role • They should not replace physicians in serving patients with complex needs but should preprocess files to increase efficiency. 30 Professional Training Curricula • Training programs are already overloaded with content and there are many more things that should be included. • How do we decide what is important enough to include. 31 Meeting Convention Obligations Rights of the Child • Universal and Special Protections • Right to Survival and Development Rights of Persons with Disabilities Article 25 Health • Require health professional to provide care of the same quality • Prevent discriminatory denial of health care… on the basis of disability 32 Child Protection Intervention • Denial of medical care is child endangerment and medical neglect. 33