Temp
advertisement

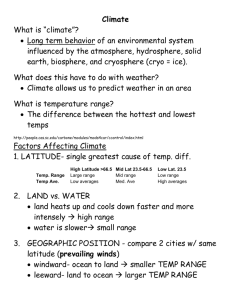
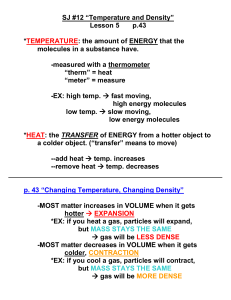
Assessing Health Vital Signs Temperature Pulse Respiration Blood pressure Body Temp • Reflects the balance between heat production and heat loss. • Core temp: in the deep tissues of the body (abdominal cavity)(36-37.5°C) • Surface temp. of the skin Factors affect heat production • Basal Metabolic Rate (rate of energy utilization in the body required to maintain essential activities): ↑ in younger persons. • Muscle activity: shivering ↑ BMR • Thyroxine output: (chemical thermo-genesis) (stimulation of heat production through cellular metabolism) Factors affect heat production • Fever: ↑ cellular metabolism • Epinephrine and sympathetic stimulation Heat Loss • Radiation: b/w 2 surfaces without contact • Conduction: from higher to lower temp (swimming in cold water) • Convection: dispersion of heat by air currents. • Vaporization: evaporation from respiratory tract. Regulation of body temp • Sensors (detect heat/ cold & send signals to reduce temp or increase heat production) • Integrator in the hypothalamus • Effector system to adjust production and loss of heat • Sensors detect cold → vasoconstriction, shivering • Sensors detect warmth → sweating, peripheral vasodilatation Factors affecting body temp • Age (thermoregulation control) (extreme age groups) • Diurnal variation (early morningsleep) • Exercise: increase temp Factors affecting body temp • Hormones (progesterone ↑ temp) • Stress ↑ production of adrenaline • Environment changes. Alterations in body temp • Average (36-38° C) • Pyrexia (hyperthermia) (38-41° C) = Fever= Febrile. • Hyperpyrexia (more than 41° C) • Hypothermia (below 36° C) Common types of fever • Intermittent: alteration of temp on regular intervals • Remittent: wide range of temp fluctuation than 2 °C/24 hrs. • Relapsing: short febrile periods of a few days. • Constant:always remains above normal • Fever spike: rapid rise of temp. S + S OF HYPERTHERMIA • • • • • • • ↑ HR ↑ Resp rate Shivering Cold skin, pallor Photosensitivity ↑ thirst Mild to severe dehydration Nursing Care of ↑ thermia • Monitor V/S • Assess skin: color and temp. • WBC’s • Remove excessive clothes/blankets • Adequate fluids and nutrition •I&O • Antipyretics as prescribed • Tepid sponges Hypothermia • Excessive heat loss • In adequate heat production • Impaired hypothalamic control (regulation) Clinical S + S of ↓thermia • • • • • • • ↓ temp., pulse and resp. Severe shivering Chills Pale, cool. Hypotension ↓ urinary output Drowsiness progressing to coma Nursing Care of ↓thermia • • • • Warm environment Dry clothes Warm IV fluids Warm pads (sponges) Assessing body temp • Oral (food, fluids, smoking, exercise) • Rectal (very accurate) (3.5 cm) (C/I in MI, diarrhea, rectal surgery or diseases) • Axillary (newborn) (inaccurate in fever) • Tympanic (membrane injury) Types of thermometers • Long tip :oral • Rounded : rectal/ Axillary • Electronic • Chemical disposable • Infrared • Skin tape Temp scales • C = (Fahrenheit – 32) x 5/9 • F = (Celsius x 9/5)+ 32 Oral temperature • Accessible and convenient • Easily break down • Inaccurate if hot or cold fluids or smoke ingestion • Injury post oral surgery Rectal temp • Reliable and the most accurate measurement • Inconvenient and unpleasant • Difficult to those clients cannot turn • Could injure rectum post rectal injury • Presence of stool may interfere accuracy Axillary temp • Safe and non invasive • Must left long period of time Tympanic temp • Accessible • Reflects core temp • Very fast • Uncomfortable and may be invasive to membrane • Varied repeated measures • Cerumen may affect readings General guidelines in temp assessment • • • • Explain procedure Hand washing Privacy Sim’s or lateral position • Protective sheath or lubricant • 2-3 min for an oral (either side of frenulum) or rectal temp (deep breath and 3.5 cm against rectal wall) • 6-10 min in axillary (bulb in the center of axilla) temp • Pull pinna slightly upward and backward, anteriorly to ear drum in tympanic temp. • Wiping glass thermometer • Read temp • Wash thermometer • Documentation General guidelines in temp assessment • Use axillary temp in infants • Tympanic or axillary routs are preferable in children