ADD/ADHD
advertisement

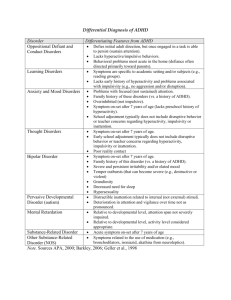
APE FACT SHEET ADD/ADHD Attention Deficit Disorder / Attention Deficit Hyperactivity Disorder DEFINITION: Attention-deficit/hyperactivity disorder (ADHD) is a neurobiological disorder characterized by developmentally inappropriate impulsivity, inattention, and in some cases, hyperactivity. Distractibility (poor sustained attention to tasks) Impulsivity (impaired impulse control and delay of gratification) Hyperactivity (excessive activity and physical restlessness) In order to meet diagnostic criteria, these behaviors must be excessive, long-term, and pervasive. The behaviors must appear before age 7, and continue for at least 6 months. A crucial consideration is that the behaviors must create a real impediment in at least two areas of a person's life, such as school, home, work, or social settings. These criteria set ADHD apart from the "normal" distractibility and impulsive behavior of childhood, or the effects of the hectic and overstressed lifestyle prevalent in our society. The exact nature and severity of AD/HD symptoms varies from person to person. SYMPTOMS AND DIAGNOSTIC CRITERIA FOR ADHD: Adapted from CDC - DSM-IV Criteria for ADHD Deciding if a child has ADHD is a several-step process. There is no single test to diagnose ADHD, and many other problems, like anxiety, depression, and certain types of learning disabilities, can have similar symptoms. The American Psychiatric Association's Diagnostic and Statistical Manual-IV, Text Revision (DSM-IV-TR) is used by mental health professionals to help diagnose ADHD. I. Either A or B: A. Six or more of the following symptoms of inattention have been present for at least 6 months to a point that is inappropriate for developmental level: Inattention 1. Often does not give close attention to details or makes careless mistakes in schoolwork, work, or other activities. 2. Often has trouble keeping attention on tasks or play activities. 3. Often does not seem to listen when spoken to directly. 4. Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (not due to oppositional behavior or failure to understand instructions). Updated 2012, by Young (Reviewed by Maldonado) 5. Often has trouble organizing activities. 6. Often avoids, dislikes, or doesn't want to do things that take a lot of mental effort for a long period of time (such as schoolwork or homework). 7. Often loses things needed for tasks and activities (e.g. toys, school assignments, pencils, books, or tools). 8. Is often easily distracted. 9. Is often forgetful in daily activities. B. Six or more of the following symptoms of hyperactivity-impulsivity have been present for at least 6 months to an extent that is disruptive and inappropriate for developmental level: Hyperactivity 1. Often fidgets with hands or feet or squirms in seat when sitting still is expected. 2. Often gets up from seat when remaining in seat is expected. 3. Often excessively runs about or climbs when and where it is not appropriate (adolescents or adults may feel very restless). 4. Often has trouble playing or doing leisure activities quietly. 5. Is often "on the go" or often acts as if "driven by a motor". 6. Often talks excessively. Impulsivity 7. Often blurts out answers before questions have been finished. 8. Often has trouble waiting one's turn. 9. Often interrupts or intrudes on others (e.g., butts into conversations or games). II. III. IV. V. Some symptoms that cause impairment were present before age 7 years. Some impairment from the symptoms is present in two or more settings (e.g. at school/work and at home). There must be clear evidence of clinically significant impairment in social, school, or work functioning. The symptoms do not happen only during the course of a Pervasive Developmental Disorder, Schizophrenia, or other Psychotic Disorder. The symptoms are not better accounted for by another mental disorder (e.g. Mood Disorder, Anxiety Disorder, Dissociative Disorder, or a Personality Disorder). Based on these criteria, three types of ADHD are identified: 1. ADHD, Combined Type: if both criteria IA and IB are met for the past 6 months 2. ADHD, Predominantly Inattentive Type: if criterion IA is met but criterion IB is not met for the past six months 3. ADHD, Predominantly Hyperactive-Impulsive Type: if Criterion IB is met but Criterion IA is not met for the past six months. Updated 2012, by Young (Reviewed by Maldonado) TREATMENTS: In most cases, ADHD is best treated with a combination of medication and behavior therapy. MEDICATIONS Medications can affect children differently, where one child may respond well to one medication, but not another. o Stimulants are the best-known and most widely used treatments. Between 70-80 percent of children with ADHD respond positively to these medications. Adderall Dexedrine Methylin Addrerall XR Dextrostat Ritalin Concerta Focalin Ritalin SR Cylert Focalin XR Ritalin LA Daytrana Metadate CD Vyvanse Common side effects of stimulants for ADD & ADHD: Feeling restless and Irritability, mood jittery swings Difficulty sleeping Depression Loss of appetite Dizziness Headaches Racing heartbeat Upset stomach Tics o Nonstimulants were approved for treating ADHD in 2003. This medication seems to have fewer side effects than stimulants and can last up to 24 hours. Strattera Overall, while Strattera appears to have fewer side effects, studies show that stimulant drugs are more effective. BEHAVIORAL INTERVENTIONS o Create a routine o Get organized o Avoid distractions o Limit choices o Change interactions with the child o Use goals and rewards o Discipline effectively TEACHING TIPS AND SPECIAL CONSIDERATIONS: Many Children with ADD/ADHD experience difficulty in school, where attention, quick cognitive processing, and motor control are functional requirements for success. Children with ADD/ADHD can show inconsistent and unpredictable behaviors. They respond best in structured and predictible envronments. Provide students with clear rules and expectations with defined immediate consequences. o Post daily schedules and assignments (explain any schedule changes) o Teach self-monitoring strategies Updated 2012, by Young (Reviewed by Maldonado) Use visual and verbal instructions Give frequent feedback & positive reinforcers Give students time to prepare answers/responses if called on Use children for demonstrations, keep them engaged Ask simple questions (check for understanding) if attention starts to wander Work on quality instead of quantity Proximity control Break down large projects into small tasks Decrease the length of activities, and have planned smooth transitions Alternate teaching styles: o Use videos, music, flash cards, small groups, alternate student leaders o Incorporate the children’s interests into lessons and activities o Assessment suggestions: o Behavior assessment o Participation assessment o Persistence and attention assessment o o o o o o o o o o RECOMMENDED ACTIVITIES o Trampoline – jumping and rebounding o Meditation o Yoga o Walking/running outdoors o Martial arts o Dancing, aerobics, gynmastics, stretching o Swimming and aquatic activities o Highly aerobic activities o Cooperative activities (challenging but very benificial) Information on this sheet contains only suggested guidelines. Each student must be considered individually, and in many cases, a physician’s written consent should be obtained. References: CDC - ADHD, Symptoms and Diagnosis - NCBDDD. (n.d.). Centers for Disease Control and Prevention. Retrieved February 19, 2012, from http://www.cdc.gov/ncbddd/adhd/diagnosis.html ADHD Medication - ADHD Medicine like Ritalin, Adderall and Other ADHD Medications. (n.d.). ADHD Treatment – ADD and Attention Deficit Hyperactivity Disorder Information. Retrieved February 19, 2012, from http://www.add-adhd-treatments.com/ADHD-Medication.html Davis., & Dillon. (2010). ADD/ADHD. Adapted Physical Education Desk Reference (pp. 19-22). Blacksburg, VA: PE Central. Updated 2012, by Young (Reviewed by Maldonado)