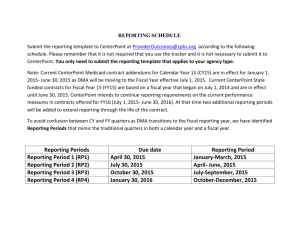
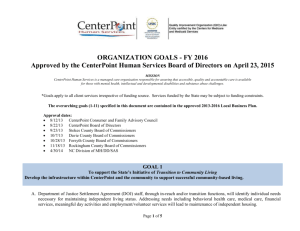
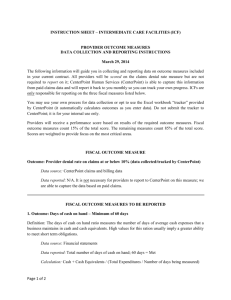
Provider Manual
advertisement

Revised 7/21/15 1 Table of Contents SECTION I: INTRODUCTION AND OVERVIEW A. Welcome to CenterPoint .................................................................................................................. 7 B. An Overview of CenterPoint ........................................................................................................... 7 C. The CenterPoint Model.................................................................................................................... 8 1. Financial Model .................................................................................................................. 8 2. A Self-Managed System ..................................................................................................... 8 D. CenterPoint Mission, Vision and Values ...................................................................................... 8-9 E. The Medicaid Waiver- What is the NC MH/DD/SAS Health Plan? ............................................... 9 F. Opportunities Presented by the 1915 (b)/(c) Waiver System .......................................................... 9 G. About the NC MH/DD/SAS Health Plan ...................................................................................... 10 H. About the NC Innovations Waiver ........................................................................................... 10-11 SECTION II: CENTERPOINT GOVERNANCE AND ADMINISTRATION A. B. C. D. E. F. G. H. I. J. K. L. M. N. O. Governance .................................................................................................................................... 11 Executive Team ............................................................................................................................. 11 Network Management .............................................................................................................. 11-12 Clinical Operations ................................................................................................................... 12-15 Quality Management ................................................................................................................ 15-16 Finance........................................................................................................................................... 16 Information Systems (IS) .......................................................................................................... 17-20 Care Coordination (CC) ............................................................................................................ 20-22 Community Operations .................................................................................................................. 22 Client-Related Functions ............................................................................................................... 23 CenterPoint CCO/Medical Director............................................................................................... 23 Stakeholder Involvement in CenterPoint System Management .................................................... 23 Waiver Advisory Committee .................................................................................................... 23-24 Operational Committees ................................................................................................................ 24 Cross Functional Team Relationships…………………………………………………………25 SECTION III: PROVIDER NETWORK A. B. C. D. E. F. G. H. I. J. The CenterPoint Provider Network ............................................................................................... 26 Cultural Competency of the Network ............................................................................................ 26 Types of Network Providers ..................................................................................................... 27-29 Location of Providers .................................................................................................................... 29 Quality of Care ......................................................................................................................... 29-31 Provider Communication ............................................................................................................... 32 CenterPoint Area Providers Council......................................................................................... 33-34 Changes in Credentialed Status – Licensed Independent Practitioners ......................................... 34 Re-Credentialing – Licensed Independent Practitioners................................................................ 35 Alteration of Practitioner’s Credentialed Status ............................................................................ 36 Revised 7/21/15 2 K. L. M. N. O. P. Q. R. S. T. Reconsideration of Credentialing Decisions.................................................................................. 36 Actions Against Practitioner’s Credentialing Reported to External Bodies .................................. 36 Changes In Enrollment/Contract Status ......................................................................................... 37 Applying for Additional Services ............................................................................................. 37-38 Health and Safety Site Reviews ..................................................................................................... 38 CenterPoint Network Development Plan ....................................................................................... 38 Specialty Providers ........................................................................................................................ 38 Licensed Independent Practitioners ............................................................................................... 39 Clinical Home for Clients .............................................................................................................. 39 Network Design ............................................................................................................................. 39 SECTION IV: CONTRACTS A. Agency Contracts...................................................................................................................... 40-41 B. Licensed Independent Practitioner Contracts ........................................................................... 41-42 SECTION V: CLIENT RIGHTS AND EMPOWERMENT A. B. C. D. E. F. G. H. I. J. K. L. M. N. Rights of Client ......................................................................................................................... 42-43 Civil Rights ............................................................................................................................... 43-44 Informed Consent .......................................................................................................................... 44 Advocacy for Client ....................................................................................................................... 45 Psychiatric Advanced Directives .............................................................................................. 45-46 Confidentiality .......................................................................................................................... 46-47 Second Opinion ............................................................................................................................. 47 Client Appeals .......................................................................................................................... 48-49 Due Process for Medicaid Decisions ............................................................................................. 49 Client Reconsideration.............................................................................................................. 49-51 Non-Medicaid Service Complaint Process ............................................................................... 53-54 Grievances ..................................................................................................................................... 54 Human Rights Committee ............................................................................................................. 55 Consumer and Family Advisory Committee ............................................................................ 55-56 SECTION VI: BENEFIT PACKAGE A. B. C. D. E. F. G. H. I. J. Eligibility ....................................................................................................................................... 56 Who is Eligible for the Medicaid Waivers?.............................................................................. 56-57 Medicaid Waiver Disenrollment .................................................................................................... 57 Eligibility of State Funded Services .............................................................................................. 58 Eligibility for Reimbursement by CenterPoint .............................................................................. 58 Enrollment of Clients ................................................................................................................ 58-60 Service Definitions ........................................................................................................................ 60 Special Needs Populations Designed in the NC MH/DD/SAS Health Plan ............................. 60-62 Service Array ................................................................................................................................. 62 Medicaid Transportation Services ................................................................................................. 62 SECTION VII: CENTERPOINT CLINICAL DESIGN PLAN ...................................................... 62-63 Revised 7/21/15 3 SECTION VIII: ACCESS, ENROLLMENT AND AUTHORIZATION OF SERVICES A. Customer Services Description...................................................................................................... 63 Includes Customer Services Coordinators, Customer Services Clinicians, Eligibility/Enrollment Specialists, Customer Services Liaisons B. Customer Services Process ....................................................................................................... 63-66 C. Access to Services .................................................................................................................... 66-71 Includes Routine Service, Urgent Service, Emergent Service D. Process for Telephonic Pre-Service-Authorization by Calling UM/Provider Line: (1-888-220-5280) ............................................................................................................ 71-74 E. Registry of Unmet Needs............................................................................................................... 74 F. Enrollment ..................................................................................................................................... 75 Includes Processes for Providers with and without an electronic link to CenterPoint G. Initial Assessment .......................................................................................................................... 75 H. Initial Authorization.................................................................................................................. 75-78 I. Continued Authorization of Services ........................................................................................ 78-80 J. Discharge Review ..................................................................................................................... 80-81 K. Utilization Review .................................................................................................................... 81-82 SECTION IX: STATE SERVICE DEFINITIONS ............................................................................... 82 Includes NC MH/DD/SAS Health Plan – 1915 (b) Waiver, NC Innovations Plan – 1915 (c) Waiver and (b)3 Services SECTION X: RESOURCES FOR PROVIDERS 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Training and Technical Assistance ................................................................................................ 83 Advocacy ....................................................................................................................................... 83 Associations .............................................................................................................................. 83-84 Behavioral Healthcare Resources ................................................................................................. .84 Client and Family Resources .................................................................................................... 84-85 Cultural Competency ................................................................................................................ 85-86 Intellectual/Developmental Disabilities .................................................................................... 86-87 Federal Government ...................................................................................................................... 87 Grants and RFPs ............................................................................................................................ 87 North Carolina State Links ............................................................................................................ 88 Other State Links ........................................................................................................................... 88 SECTION XI: GETTING PAID A. Enrollment and Eligibility Process ........................................................................................... 89-90 Includes Eligibility Determination, Key Data to Capture during Enrollment, Effective Date of Enrollment, Member ID B. Authorizations Required for Payment ........................................................................................... 90 Includes System Edits, Authorization Number and Effective Dates, Service Categories or Specific Services, Units of Service, Exceptions to Authorization Rule C. Payment of Claims and Claims Inquiries ................................................................................. 91-92 Revised 7/21/15 4 D. E. F. G. H. I. J. K. Includes Timeframes for Submission of Claims, Process for Submission of Replacement and Voided Claims, Provider Direct Claims Submission, 837 Claims Submission, Providers Who Submit Paper Claims and Documentation Service Codes and Rates ̶ Contract Provisions ............................................................................ 92 Standard Codes for Claims Submission......................................................................................... 92 Includes CPT/HCPCS/Revenue Codes, Modifiers, Diagnosis Codes, Place of Service Codes Definition of Clean Claims ............................................................................................................ 92 Coordination of Benefits........................................................................................................... 92-93 Includes Eligibility Determination Process by Provider, Obligation to Collect, Reporting of Third Party Payments Response to Claims........................................................................................................................ 93 Includes Remittance Advice, Electronic Remittance Advice (835) for 837 Providers, Management of Accounts Receivable - Provider Responsibility Fee-For-Service Equivalency ........................................................................................................ 94 Includes Contract Agreement, Review of FFSE Process, Reconciliation Claims Investigations of Fraud and Abuse ............................................................................... 94-95 Includes Trends of Abuse and Potential Fraud, Audit Process, Role of Finance Department, Voluntary Repayment of Claims, Reporting to State and Federal Authorities Repayment Process/Paybacks ........................................................................................................ 96 SECTION XII: STANDARDS AND REGULATORY COMPLIANCE A. Quality Improvement ..................................................................................................................... 97 B. Performance Measurement ............................................................................................................ 98 Includes Data Collection and Verification, Performance Improvement, C. Performance Monitoring ......................................................................................................... 98-100 Includes Monitoring of Incidents, CenterPoint Incident Review Process, Monitoring to Assure Quality of Care, Grievances, Client Satisfaction Surveys and Mystery Shopping Program D. Corporate Compliance .......................................................................................................... 100-101 Includes Primary Areas Covered by Corporate Compliance, Corporate Compliance Plan E. Monitoring and Auditing ............................................................................................................. 101 F. Investigation of Violations .......................................................................................................... 102 G. Client Records Retention and Disposal Standards ............................................................... 102-103 H. Minimum Standards of Documentation in Client Medical Records ........................................... 103 I. Information Systems .................................................................................................................... 104 SECTION XIII: REVIEW PROCESS FOR PROVIDERS AND RECONSIDERATION A. B. C. D. E. Roles and Responsibilities of the Network Management Department ........................................ 105 Roles and Responsibilities of the Network Operations Cross-Functional Team .................. 105-106 Roles and Responsibilities of the Credentialing Committee ....................................................... 106 Role and Responsibilities of the Finance Department .......................................................... 106-107 Provider Disputes.................................................................................................................. 107-108 Revised 7/21/15 5 SECTION XIV: OFFICIAL COMMUNICATION BULLETINS ..................................................... 108 SECTION XV: GLOSSARY OF TERMS..................................................................................... 109-121 Revised 7/21/15 6 SECTION I: INTRODUCTION CenterPoint Human Services (CenterPoint), its contractors and employees do not discriminate on the basis of race, color, national origin, sex, religion, age or disability in the provision of services. A. Welcome to CenterPoint’s Provider Network Thank you for choosing to be a part of the CenterPoint Human Services Provider Network. CenterPoint looks forward to partnering with providers in promoting wellness, self-determination and recovery in the lives of the people we serve. This Provider Manual is an important tool and includes detailed policies and procedures that impact referrals and authorizations, claims submissions, problem resolution and other areas that impact our partnership. As a contract provider, it is your responsibility to familiarize yourself and your employees with the information contained in this manual. Compliance with CenterPoint’s policies and procedures is necessary to fulfill your contractual obligations as a service provider. This manual includes a glossary of frequently used terms and website links to necessary forms and helpful resources. In addition to this manual, CenterPoint offers an array of scheduled trainings and technical assistance to support your success. Do not hesitate to contact us with questions. B. An Overview of CenterPoint CenterPoint functions as a state-mandated Local Management Entity (LME) and Medicaid-funded Managed Care Organization (LME/MCO). The LME/MCO serves Forsyth, Stokes, Davie and Rockingham Counties with a total population of over 500,000. CenterPoint contracts with providers to offer quality mental health, intellectual/developmental disabilities and substance use services to Medicaid beneficiaries and to eligible individuals without Medicaid (henceforth “client” refers generically to persons whose behavioral health services are funded by Medicaid and/or non-Medicaid funding sources, unless a specified funding source is identified). CenterPoint’s success is the result of client empowerment, implementation of evidence-based and best practices, the System of Care philosophy, partnerships with service providers, and extensive community collaboration with citizens, advocates and community agencies. CenterPoint is equally committed to working with the NC Department of Health and Human Services (DHHS) Division of Mental Health, Developmental Disabilities and Substance Abuse Services (MH/DD/SAS) and the NC Division of Medical Assistance (DMA) in the use of public resources to build a strong, community-based service system. CenterPoint is governed by a board of directors. Its members are appointed by the boards of county commissioners in each of the four contiguous counties within the catchment area. The board’s composition is defined in North Carolina General Statute (NC G.S.) §122C-118.1 and includes specified membership including a commissioner from each constituent county or their designee, consumer and family representatives as well as citizens with specific experience or expertise. Revised 7/21/15 7 C. The CenterPoint Model Financial Model: CenterPoint’s financial model utilizes strategies to re-deploy existing dollars more efficiently and effectively such as blending Medicaid, state and county funding under a single financial manager. Re-engineering the mental health care system away from the use of high-cost and institutional services to a community based system requires that a single entity has the authority to manage the full continuum of care. The NC MH/DD/SAS Health Plan, which consists of the 1915(b) Medicaid Waiver and the 1915(c) Medicaid Waiver, are especially important in redirecting services into more efficient, best practice models of intervention. Capitation of coverage supports the creative flexibility that is necessary in a client driven system of care. Additional services and supports have been developed through Medicaid 1915(b) 3 authority. These services are based on evidence based practices which support the achievement of positive outcomes for people with behavioral health and developmental disabilities. These (b) 3 services provide the additional tools needed to reduce reliance on high cost institutional and facility care and offer a greater range of community services. Self-Managed System Model: CenterPoint’s self-managed system relies on providers who adhere to CenterPoint’s treatment philosophy and community standards of practice, which are clarified in the Clinical Design Plan. Our goal is to develop a system in which the structure, requirements and expectations are so well understood by our providers that extensive intervention by CenterPoint is not required. We want our providers to be involved in managing the system, assisting in the creation of strategies to meet performance objectives, reviewing system performance and developing solutions for systemic problems. Providers participate with CenterPoint through the CenterPoint Area Providers Council, the Clinical Advisory Committee, the Waiver Advisory Groups, and the Global Continuous Quality Improvement Committee (GCQIC). Provider participation in the ongoing operations of the CenterPoint system is critical to developing strategies that will be effective in achieving our goals. Our objectives are to provide easy access to appropriate, high quality services for clients, and to eliminate ineffective services and practices with poor outcomes. Providers are expected to deliver services consistent with those clinical practice guidelines developed and approved by CenterPoint and promulgated on the CenterPoint website (www.cphs.org). D. CenterPoint’s Mission, Vision and Values Mission: CenterPoint Human Services is a managed care organization responsible for assuring that accessible, quality and accountable care is available for those with mental health, intellectual and developmental disabilities and substance abuse challenges. Vision: CenterPoint Human Services will become the best practice public model of managed care for exceptional and compassionate oversight of the provision of care for those with mental health, intellectual and developmental disabilities and substance abuse challenges. Values: We will live out our Mission by: Respecting and valuing all individuals Revised 7/21/15 8 Serving individuals and families with compassion and care Maintaining an unwavering commitment to high quality care given by our provider network Being responsible stewards of the funds entrusted to us Seeking to raise awareness of the needs and challenges of behavioral health in our community Operating with transparency, openness, responsiveness and in collaboration with the many partners within the counties we serve E. The Medicaid Waiver – What is the NC MH/DD/SAS Health Plan? The NC MH/DD/SAS Health Plan is a pre-paid inpatient health plan (PIHP) funded by Medicaid. All Medicaid MH/DD/SA services are authorized by and provided through the CenterPoint Provider Network in accordance with the risk contract between the DMA and CenterPoint. As a prepaid inpatient health plan, CenterPoint assumes financial risk for a discrete set of MH/DD/SA services including both NC Medicaid State Plan services and services included in the NC Innovations Waiver. The NC MH/DD/SAS Health Plan is a combination of two types of Waivers: a 1915(b) Waiver, generally known as a Managed Care/Freedom of Choice Waiver, and a 1915(c) Waiver, generally known as a Home and Community-Based Waiver. Through the 1915(b) section of the Social Security Act, states are permitted to submit a request to waive some Medicaid requirements in order to provide alternatives to the traditional fee for service system of care. Likewise, the 1915 (c) section of the Social Security Act permits states to submit a request to waive some Medicaid requirements in order to provide alternatives to institutional care. Both Waivers are approved under different federal Medicaid regulations and require different reporting and oversight. This type of Waiver system is not intended to limit care but to create an opportunity to work closely with clients and providers on better coordination and management of services, resulting in better outcomes for clients and more efficient use of resources. F. Opportunities Presented by the 1915(b)/(c) Waiver System The 1915 (b)/(c) Medicaid Waiver allows CenterPoint to better coordinate a system of care for clients, families and providers. The Waiver also promotes efficient management of limited public resources. We are able to manage all system resources so that money can be directed to services most appropriate for identified client needs. Finally, the Waiver permits greater flexibility in services offered. CenterPoint has developed a broader range of services and supports including new services in the community that will help to reduce and redirect reliance on high cost institutional and hospital care. G. About the NC MH/DD/SAS Health Plan Key points in North Carolina’s MH/DD/SAS Health Plan are: 1. Locally, the 1915(b)/(c) Medicaid Waiver applies to clients with Medicaid, who reside in Forsyth, Stokes, Davie and Rockingham Counties. 2. All Medicaid clients in specified eligibility groups will be eligible and will be automatically enrolled in this plan for their mental health, intellectual/developmental disability and substance abuse service needs. 3. The services that are available will include current NC State Mental Health Plan Medicaid services including Inpatient Psychiatric Care and Intermediate Care Facilities for Individuals with Intellectual/Developmental Disabilities (ICF-I/ID). Revised 7/21/15 9 4. CenterPoint will partner with the state to create additional services that have been identified as best practices in care. These services are referred to as Medicaid 1915 (b) (3) services. 5. Clients will be able to choose from any provider in CenterPoint’s network that is credentialed and contracted to provide the service they need. 6. Information and education will be provided to clients to help them choose providers. Access to care is available 24 hours daily/7 days weekly through CenterPoint’s Customer Services Center (1888-581-9988). Access is also available during regular work hours through Open Access clinics at specific provider sites. Also, any provider enrolled in CenterPoint’s network is able to begin basic services for an eligible client without going through CenterPoint or a comprehensive community provider. H. About the NC Innovations Waiver The 1915 (c), or NC Innovations Waiver, is a Home and Community Based Waiver that offers alternatives to the provision of institutional care. Funds that are typically used to serve a person with intellectual/developmental disabilities in an Intermediate Care Facility for Individuals with Intellectual/Developmental Disabilities (ICF-I/DD), through this Waiver, can be used to “follow the person” to services outside of the ICF-I/DD facility. The Waiver supports the development of a stronger continuum of services that enables individuals to move to more integrated settings. People served and their families have the information and opportunity to make informed decisions about their health care and services and exercise more control over the decisions they make regarding services and supports. The NC Innovations Waiver has provider directed and individual/family directed tracks. Under the provider directed track, services are delivered in a traditional manner from staff employed by an agency. Under the individual/family directed track, clients and their families may choose from two service models: In the Employer of Record model, the staff is hired, directed and paid by the Innovations participant/legally responsible persons with the assistance of a Community Guide and a Financial Supports Agency. In the Agency with Choice model, the provider agency is the legal employer but the participant/legally responsible person is the managing employer. The managing employer is responsible for interviewing, training, managing (with oversight by the agency Qualified Professional) and making recommendations to the provider agency for hiring and firing. A client or guardian/family member can choose provider directed, individual/family directed or a combination of both options. Revised 7/21/15 10 SECTION II: CENTERPOINT GOVERNANCE AND ADMINISTRATION A. Governance CenterPoint is a political sub-division of the state under NC G.S. §122C. It is a public authority and is governed by a Board that focuses on establishing and monitoring goals as well as policy development. CenterPoint’s Chief Executive Officer (CEO) reports to the Board; all other staff of CenterPoint report to the CEO. B. Executive Team CenterPoint’s Executive Team (ET) consists of the Chief Executive Officer (CEO), Chief Clinical Officer (CCO), Chief Operations Officer (COO), Chief Financial Officer (CFO), Chief Information Officer, (CIO) and Chief Administrative Officer (CAO). This group is responsible for the overall management of the LME/MCO including both short and long term strategic planning. The ET oversees all aspects of the LME/MCO’s operations and is charged with directing and supporting other CenterPoint management and staff in achieving goals and objectives. Planning includes resource management, provider network direction toward best practices, alignment of incentives with LME/MCO goals, investment of new dollars, and reinvestment of savings incurred from service utilization changes. The ET strives to maintain strong working relationships with state and local partners including public agencies, provider agencies, elected officials, and advocacy organizations as well as state and regional staff. CenterPoint is organized into functional departments. These departments have been established to perform operational functions that support the overall work of the agency. CenterPoint also has a system of CrossFunctional Teams (CFTs) that are organized according to business topics. CenterPoint’s departments are described in the sections that follow. C. Network Management The Network Management Department is responsible for the development and maintenance of the provider network to meet the needs of clients, assuring choice and best practices in services. The department includes two teams: Network Operations and Network Development. The Network Operations team is composed of a Manager and Provider Relations Specialists (including a Lead Provider Relations Specialist), Clinical Provider Relations Representatives, a Medical Records/Processing Assistant, and a Provider Affairs Specialist. Network Operations supports the network provider community through the CenterPoint Area Providers Council, regular provider meetings, support of disability-specific focus groups and committees for the implementation of new services. CenterPoint assigns a Provider Relations Specialist to each provider to serve as the “Provider Liaison”, the primary point of contact for technical assistance and questions regarding administrative, contractual and technical issues. The Network Development team is composed of a Manager and Network Development Specialists for MH/SA Adult, MH/SA Child and I/DD Adult and Child, Clinical/EBP, and a trainer. The Network Development team recruits providers with demonstrated competence to meet the service needs of clients and families and coordinates provider training in best practices. The specialists analyze service need, access and network capacity and develop identified services to meet identified gaps and needs. The Network Operations CFT has Revised 7/21/15 11 the decision authority level for the Network Development Plan and the Needs Assessment, and recommends service priorities for Executive Team approval. Your responsibilities as a CenterPoint Contracted Provider are to: Assure that your provider profile in NC Tracks is current and thorough Provide services for which your agency is credentialed or enrolled by CenterPoint Notify CenterPoint of all changes that impact credentialing, including staff changes Be responsive to the cultural and linguistic needs of the clients your agency serves including the use of interpreters as needed Provide services only at enrolled service sites as outlined in your contract Obtain authorizations as required for contracted services Adhere to all performance guidelines in your contract and work to deliver best practices Work in collaboration with other providers, clients and families Work in a solution-focused and collaborative basis within the network Work with CenterPoint to mediate problem areas through Provider Relations staff or designated CenterPoint staff member Submit clean claims within ninety (90) days of the date of services unless otherwise stated in your contract CenterPoint’s responsibilities to providers are to: Actively recruit network providers with a mission and vision consistent with CenterPoint’s Support the development and support of best practices or emerging best practices Identify gaps in network services and create a strategy to develop those services through existing providers or by recruiting new providers for the network Respond to requests for applications for network enrollment according to the needs identified in the Network Development Plan. Assign a Provider Relations Specialist for each network provider as a primary contact and resource for technical assistance Keep network providers informed through provider meetings, electronic updates, the weekly The Friday Email newsletter, and the “CenterPoint website at www.cphs.org Update the Provider Manual, on at least an annual basis, and to reflect changes in requirements Identify training needs for providers and, if possible, facilitate or provide the training Credential and re-credential providers (LIPs, agencies, and facilities) D. Clinical Operations Clinical Operations includes the following departments: Customer Services, Care Coordination, Utilization Management, and Quality Management. Clinical Operations conducts the utilization management/utilization review functions, quality management activities, care coordination functions, customer services, and coordinates the crisis response system. The department defines review dates, completes concurrent and retrospective reviews, and responds to appeals related to denials or reduction of services for service requests. Additionally, the department researches utilization trends, identifies areas for further study and review, and develops Clinical Guidelines and written protocols. This unit supports the Clinical Advisory Committee. The CCO/Medical Director oversees all clinical and quality management activities performed by Clinical Operations. Revised 7/21/15 12 CenterPoint maintains a telecommunications system with 24 hours per day, 7 days per week availability. Access to care for clients is a critical function of Clinical Operations. CenterPoint is responsible for timely response to the needs of clients and for quick linkages to qualified providers of the network through a toll-free number and secure electronic enrollment system. Customer Services provides critical monitoring and management of referral follow-up to care. Utilization Management/Care Management: Utilization Management (UM) is the process of evaluating the medical necessity, appropriateness, and efficiency of behavioral health care services against established guidelines and criteria. CenterPoint has well defined procedures that are used to evaluate medical necessity, the criteria used, and the process for consistent application of these criteria for authorization and denial of services. Care Management includes activities such as the ongoing evaluation of timeliness to care; analysis of utilization patterns to monitor for both under and over utilization; gaps in care; and the use of restrictive services. UM determines whether a client meets and continues to meet medical necessity criteria (and State Benefit Plan requirements when applicable) for the frequency, intensity and duration of requested services. CenterPoint’s goal is to assure that clients receive the right service at the right time and at the right level, thereby creating the most effective and efficient treatment possible. UM staff assists the provider in managing a client’s care needs and identifying appropriate services. Medical necessity for clients with Intellectual and/or Developmental Disabilities (I/DD) is defined in NCGS122C-3(11a), the Developmental Disabilities Act of 1984, Intermediate Care Facility for Individuals with Intellectual and/or Developmental Disabilities (ICF-IDD) Level of Care criteria in NC and Medicaid and Health Choice Clinical Coverage Policy 8E (8/1/15) and The Developmental Disabilities Assistance and Bill of Rights Act of 2000 (Functional Limitations) Utilization Review (UR): The primary functions of UR are: monitoring service utilization and reviewing utilization data to evaluate and assure that services are being provided appropriately within established benchmarks and clinical guidelines; and making sure that services are consistent with the authorization and approved Person Centered Plan (PCP) / Individual Support Plan (ISP)/Treatment Plan. UR is a part of the UM process and involves auditing service samples. Information from the client’s record (assessment information, treatment plan and progress notes) is evaluated against medical necessity criteria. This is done concurrently (during re-authorization) and retrospectively (after the service has been provided). The outcome of this review can reveal areas in which provider training is needed, services that did not meet medical necessity criteria, and situations in which the client did not receive appropriate services. Indicators will be identified to select cases for review, such as high utilization of service, frequent hospital admissions and random sampling of other events. CenterPoint utilizes both Focused Utilization Review and Routine Review (which involves a sampling process across Network providers) in its UR methodologies. Focused Review: A Focused Review may be conducted based on the results of provider monitoring reports that identify outliers as compared to expected/established service levels or through specific cases identified in the CenterPoint clinical staffing process to be outside the norm. Focused samples may include: High-risk clients– Examples may include, but are not limited to, clients who have been hospitalized more than one time in a 30-day period; clients with intellectual/developmental disabilities as identified in the Risk/Support Needs Assessment; children and youth with multiple agency involvement; or active substance use by a pregnant female Under-utilization of services – Examples may include, but are not limited to, clients who utilize less than 70% of an authorized service or clients who have multiple failed appointments Revised 7/21/15 13 Over-utilization of services – Clients who continue to access crisis services with no engagement in other services Services infrequently utilized – An available practice that is not being used High-cost treatment – Clients in the top 20% of claims for a particular service Routine Utilization Review: A routine utilization review will focus on the efficacy of the clinical processes in cases as they relate to reaching the goals in the client’s PCP / treatment plan. CenterPoint will also review the appropriateness and accuracy of the service provision in relation to the authorizations. All CenterPoint contract providers currently serving CenterPoint clients are subject to utilization reviews to assure that clinical standards of care and medical necessity are being met. A routine UR will be inclusive of, but not limited to, evaluations of services across the delivery spectrum; evaluations of clients by diagnostic category or complexity level; evaluations of providers by capacity, service delivery and best-practice guidelines; and evaluations of utilization trends. The criteria used in the utilization review processes will be based on the most current, approved guidelines and service manuals utilized under the NC MH/DD/SAS 1915 (b) and (c) Waivers and processes for NC State services. These documents include, but are not limited to: the current NC State Plan service definitions with admission, continuation, and discharge criteria; the CenterPoint-approved Clinical Practice Guidelines; the current approved NC MH/DD/SAS service rules; and the current approved NC DMA Clinical Coverage Policies. Clinical Practices Guidelines Clinical practice guidelines are developed by CenterPoint’s Medical Director and Clinical Operations Team and reviewed and approved by CenterPoint’s Clinical Advisory Committee. Guidelines are obtained or developed for the common diagnoses and treatment modalities found in the population of network clients. Guidelines will be based on scientific evidence and/or the consensus of community standards, the opinion of nationally recognized professional organizations, and expert opinion. Guidelines will be used by network providers to educate and advise their staff and clients concerning the treatment of MH/SA/DD disorders. The guidelines should inform decision-making and clinical care, and CenterPoint will use the guidelines to measure provider care of clients. Practice Guidelines are posted on the external website -- www.cphs.org – and may also be distributed by email. Providers and clients can obtain hard copies of the Guidelines by calling the Provider ACCESS Line 1888-220-5280. Please note that since the Clinical Practice Guidelines posted on the CenterPoint website cover all areas of disabilities, each Provider is responsible for reviewing and identifying those guidelines applicable to the services they deliver. Clinical Practice Guidelines posted on the CenterPoint website cover all areas of disability, providers must review the guidelines and determine which are applicable to the services they deliver. Providers may be monitored for compliance with Clinical Practice Guidelines. CenterPoint staff will focus solely on those guidelines that relate to the Provider’s scope of work. Monitoring may include: Random reviews of Service Authorization Requests Focused reviews due to identification of issues related to clinical practices Investigation of Quality of Care Concerns related to clinical practice Focused reviews of issues identified in routine provider monitoring Revised 7/21/15 14 Your responsibility as a CenterPoint Contracted Provider is to: Submit service authorization requests (SAR) with the proper clinical information to allow UM staff to review for medical necessity. Submit continuing service authorization requests on a timely basis (no later than 14 days prior to the service start date) to allow for UM activities and authorizations prior to beginning services (Note: Emergency authorizations are available, but should only be used when necessary to provide for client health, safety and well-being. See Section III for authorization instructions.) CenterPoint’s responsibilities to providers are to: Provide accurate and timely responses to service authorization requests Assure that clients receive services for which they are eligible and which are clinically appropriate E. Quality Management Quality Management (QM) has oversight for quality assurance and improvement activities throughout the CenterPoint system. QM supports a continuous quality improvement (CQI) system that includes all network providers. The department provides monitoring information to the Human Rights Committee and tracks and trends client incidents and deaths. Quality Management is also responsible for the handling and tracking of grievances and Quality of Care Concerns and for working toward their resolution. Your responsibilities as a CenterPoint Contracted Provider are to: Cooperate fully with any complaint inquiry or follow-up Provide CenterPoint with any requested records and documentation needed to resolve issues within the timeframe specified (Note: The timeframe will vary according to circumstances.) Notify CenterPoint of any concerns/complaints you have in regards to the services provided by the LME/MCO and work with us to develop solutions Develop and implement a CQI system which includes, at a minimum, the development of systems to self-evaluate services, evaluate collected data, and identify needed areas of improvement Implement strategies to address areas of improvement and continual evaluation and refinement of processes Develop/implement systems to assess that clients are achieving positive outcomes from services offered Review, mediate and/or investigate complaints received regarding the quality of services provided by any agency and assure that appropriate corrections are completed if needed CenterPoint’s responsibility to providers: Monitor client satisfaction and positive outcomes for clients Coordination of a CQI system for CenterPoint and the network that includes ongoing evaluation and planning in relation to needed areas of improvement in the service delivery system Review, mediate and investigate complaints regarding the quality of services provided by any agency and assure appropriate corrections are completed if needed Monitor data from across the network and evaluate for trends and patterns Provide training and technical assistance to the provider/practitioner network Revised 7/21/15 15 F. Finance CenterPoint’s Finance Department manages the financial resources of the LME/MCO. This includes management of accountability, availability of funds, claims processing and payment. Finance is responsible for assuring compliance with NC G. S. §159 (The Local Government Fiscal Control Act) and other general accounting requirements. The department supports providers through training and through its Claims Processing Assistants. Your responsibilities as a CenterPoint Contracted Provider are to: Verify client insurance coverage at the time of referral, or o Admission, or o Each appointment, and o On a quarterly basis Determine the client’s ability to pay for all designated non-Medicaid services based on your agency’s contract requirements Bill all first and third party payers prior to submitting claims to CenterPoint Report all first party required fees and third party payments and denials on the claim Submit clean claims electronically within ninety (90) days of the date of service unless otherwise stated in your contract Identify all billing errors to CenterPoint’s Finance Department Manage your agency’s accounts receivable Maintain a denial rate of 10% or less Maintain current, accurate data in NC Tracks Submit all documentation which is required for federal, state, or grant reporting requirements including, but not limited to, required client enrollment demographics that must be reported to the State of North Carolina by CenterPoint CenterPoint’s responsibilities to providers are to: Review and approve all financial commitments made by CenterPoint Certify funding for all contracts in accordance with NC G.S. §159 Assign and monitor maximum funding for contracts Monitor grant funds Monitor retroactive Medicaid eligibility and recovery of funds Manage claims processing to achieve timely payment for providers Issue payments and remittance advices (RAs) on paid and denied claims Assist with review of financial reports, financial statements, audits, and accounting procedures Recover funds based on audit findings Audit providers for coordination of benefits (COB) Pay clean claims within prompt pay guidelines Revised 7/21/15 16 G. Information Services CenterPoint recognizes the importance of management information systems that effectively support the day-today operations of the various functional areas. Consequently, CenterPoint maintains a comprehensive information management system that promotes the safe and accurate handling of data. CenterPoint operations and activities are accomplished, primarily, in an electronic environment. The Information Services (IS) team takes great care in protecting clients’ written and oral protected health information (PHI) or individuallyidentifiable health information (IIHI). CenterPoint has adopted standards for securing PHI and IIHI, not only for its own operation, but for its delegates as well. CenterPoint has several mechanisms in place to ensure data accuracy and traceability, or “data integrity.” For example, when a Utilization Management (UM) Clinician or Specialist opens a record, there is a high level of confidence that the record retrieved is, indeed, the correct record and that the information documented therein is accurate. Verifying accuracy and completeness of information received from providers is critical. The process begins when the provider sends an authorization request to CenterPoint. If the authorization request is complete it is assigned to the designated UM staff caseload for review and is noted in the electronic system as under review. Clinical non-authorizations based on interpretation of clinical information are never issued by non-clinical staff. UM staff record their decisions in the system. The decision is communicated to stakeholders via the Provider portal. An audit trail is maintained for all service requests and UM decisions. If the authorization request is incomplete, it is noted in the electronic system. A message is sent to the provider via the web portal that the request is being returned as “unable to process.” Also included is a statement of the documents that are required before the request can be considered by UM staff. In most cases, the replies are generated from web portal templates. However, there could be occasions upon which original correspondence is completed by administrative staff and documented in the AlphaMCS system attached to the client. (Note: The “begin” date of any authorization will correspond to the date that the complete request was received.) If the request is complete but there is insufficient information to support the request, UM staff informs the individual requesting the services. The requesting provider is informed of the type of information that is needed to complete the review. Documents are stored in AlphaMCS for convenient retrieval. Providers can monitor the status of their authorization requests via this portal. AlphaMCS is used for generating reports and system edits/feedback across all functional areas including UM and resource management. Reports are reviewed by various groups at CenterPoint such as Executive Team, the Quality Operations Team and other applicable Cross Functional Teams (CFTs) and the Clinical Operations Team. The AlphaMCS database stores: Admission and discharge forms Designated target population determinations Service request forms Clinical assessments Revised 7/21/15 17 PCPs, ISPs and treatment plans Crisis plans Service orders CenterPoint maintains a generator that would immediately restore electricity to the LME/MCO if an event such as a thunderstorm leads to a loss of electricity. This generator will supply power to operate lights, telephones and computer terminals in both UM and Customer Services. The impact of a loss of telephone service for providers would have a minimal effect on UM as communication takes place via the web-based portal. As long as web-based electronic systems are functioning, UM staff would continue to receive authorization requests, review those requests, and enter the determination in the electronic client record. However, the impact of a telephone outage on Customer Services for clients is potentially very serious. The telephone system is the primary method used by which clients contact CenterPoint to request needed services. Consequently, CenterPoint has an established protocol to keep Customer Services operational during telephone and power outages. The Customer Services Disaster Recovery Plan utilizes the ability to route calls to a backup call system, to route calls to remote Customer Services staff who work from a home offices and to route calls to a backup call center vendor if necessary. In the event that the building at 4045 University Parkway was incapacitated, Customer Services could also be relocated to a redundant call center which may be located at 4035 University Parkway, or 4025 University Parkway. Any power failure or Alpha MCS outage triggers an immediate shift from electronic to paper processes. Providers are usually aware of issues with the Web-based portal system as they utilize this portal to request authorizations. During a Web-based portal outage, UM personnel accept and process authorization requests using the following manual process: 1. Urgent UM Requests: Providers have been trained to contact CenterPoint by telephone for any urgent authorization requests. Demographic and clinical information is captured on paper, and the UM Clinician conducts a clinical review of the request utilizing the appropriate medical necessity criteria. The criteria are available electronically on the Intranet. However, if the Intranet is down, the criteria are available in hard copy. The case is reviewed, in light of the criteria, and a verbal authorization is provided. All verballyissued authorizations are entered in the electronic system when functioning system is restored. 2. Non-Urgent UM Requests: During an electronic outage, providers are able to send non-urgent authorization requests to UM personnel via facsimile. Fax requests generally include the necessary demographic and clinical information. The UM staff conducts a clinical review of the request utilizing the appropriate medical necessity criteria. The criteria are available electronically on the Intranet. If the Intranet is down, the criteria are available in hard copy. Once the UM determination has been made, an authorization is provided by return fax. All facsimile-issued authorizations are entered in the electronic system when functioning is restored. 3. All Client Calls for Services: The Customer Services unit will continue to function when Information Systems are non-functional. In the event the electronic system is not available, Customer Services Clinicians continue to take telephone calls from clients and conduct the screening, triage, and referral process exactly as it occurs when the electronic system is operational. The screening tool is available in hard copy as well as Revised 7/21/15 18 within the web-based portal system. Customer Services staff members document client interactions on the hard copy backup forms that are located in Red Folders at each staff member’s desk. At a later time, the information is keyed into the system and the hard copy is shredded. In the event that a major disaster disables the use of a CenterPoint-operated site or when critical technology functions have not been restored within eight (8) hours, it is necessary to establish an alternative physical location to serve as a Command Center where essential functions can operate. The CenterPoint CEO and the Board of Directors have identified Customer Services and UM as essential functions. CenterPoint currently operates out of three locations in Winston-Salem, NC: 4025 University Parkway, 4035 University Parkway, and 4045 University Parkway. Each CenterPoint facility can serve as a Command Center if the others are damaged or destroyed by disaster. If all locations are destroyed by a disaster, then a designated, alternate location will be determined and will serve as the Command Center. In the event that a disaster occurs during normal business hours when the usual physical locations are open, emergency operations procedures will be followed to evacuate the disaster area and relocate essential functions. In the event that a disaster strikes a physical location after normal business hours, it is the responsibility of the CEO, who serves as the Lead Emergency Response Team member, to travel to the disaster location to determine relocation needs and begin the Order of Restoration Plan. In the event of a mass disaster where mental health, developmental disability and substance abuse supports may need to be offered in a triage setting, a physical location can be created to provide Crisis Provider Services. (See CenterPoint’s Comprehensive Disaster Plan.) Setting Up a Triage Location: Forsyth County CenterPoint Human Services has access to three physical locations within the Winston-Salem City limits – 4025 University Parkway, 4035 University Parkway, and 4045 University Parkway. . Additional locations can be identified by calling the American Red Cross Northwest Chapter – 336724-0511, the Salvation Army – 336-722-8721 or Forsyth County Emergency Management – 336767-6161. Stokes County Locations can be identified by calling the American Red Cross (NW Chapter) – 724-0511, Salvation Army – 336-722-8721 or Stokes County Emergency Management – 336-593-2724. Davie County Locations can be identified by calling the American Red Cross (NW Chapter) – 724-0511, the Salvation Army – 336-722-8721 or Davie County Emergency Management – 336-761-0879. Rockingham County Locations can be identified by calling the American Red Cross (NW Chapter) – 724-0511, Salvation Army – 336-722-8721 or Rockingham County Emergency Services – 336-634-3000. The Disaster Recovery Plan is tested at least every year. During each recovery test, lessons learned are documented and discussed during a post-testing debriefing. Subsequently, actual testing may be modified based on previous lessons learned. Revised 7/21/15 19 H. Care Coordination Care Coordination (CC) is a basic function of the LME/MCO available to persons with MH/SA and I/DD needs. The CC team coordinates care for individuals who are high cost/high risk, and clients in special health care needs populations. CC manages care across the continuum of care, throughout various care settings, and works in conjunction with the person, providers and others to improve outcomes for the individual and make the best use of resources. These staff members monitor care and services for clients and link them to needed psychological, behavioral, educational and physical evaluations. They monitor the individualized service plan/person centered plan (ISP/PCP), the health and safety of clients as well as provide education regarding all available MH/DD/SA services and supports. The Care Coordination team works with Community Care of North Carolina (CCNC) and primary health care providers to assure integration of care and to address physical health care needs. Care Coordination oversees the development of a comprehensive Person-Centered Plan/Individual Service Plan. If a client is hospitalized, Care Coordination will contact providers to discuss triggers and preventative issues to reduce the risk of re-hospitalization and assure that clients’ needs are being met. In August 2012 the State of North Carolina entered into an agreement with the United States Department of Justice. This agreement was reached in response to the Department of Justice’s concern about a pattern in North Carolina of persons with disabilities being placed in adult care homes. The purpose of the agreement was to make sure persons with behavioral health issues are allowed to reside in the least restrictive setting of their choice. The emphasis is on moving from settings like adult care homes where all residents have some type of disability to independent living situations where they can be integrated with persons without disabilities. The NC Department of Health and Human Services implemented the agreement through the Transition to Community Living Initiative (TCLI). The Transition to Community Living Initiative has six primary components: 1. In-Reach and Transition - Providing or arranging for frequent education efforts and discharge planning targeted to individuals in adult care homes and state psychiatric hospitals. 2. Diversion – Diverting individuals from being admitted to adult care homes. 3. Housing – Providing community-based supportive housing with tenancy supports. 4. Supported Employment – An evidence-based service to assist individuals in preparing for, identifying, and maintaining integrated, paid, competitive employment. 5. Assertive Community Treatment – An evidence-based treatment and support model of services offering intensive customized, community-based services for people with mental illness. 6. Quality Management – using data to evaluate progress and outcomes. Target Population for In-Reach includes: 1. Individuals with Serious Mental Illness (SMI) who reside in ACHs determined by the State to be an IMD 2. Individuals with Serious and Persistent Mental Illness (SPMI) who are residing in ACHs licensed for at least 50 beds and in which 25% or more of the resident population have a mental illness Revised 7/21/15 20 3. Individuals with SPMI who are residing in ACHs licensed for between 20 and 49 beds and in which 40% or more of the resident population have a mental illness 4. Individuals with SPMI who are or will be discharged from a State Psychiatric Hospital and who are homeless or have unstable housing 5. Individuals diverted from entry into ACHs pursuant to the pre-admission screening and diversion provisions established by the State Your responsibilities as a CenterPoint Contracted Provider are to: Actively participate in a process with others serving the individual to develop a comprehensive individualized service plan/person centered plan. For ISPs, providers are responsible for completing the short term goals and the task analysis. Develop treatment and/or habilitative programs that are in accordance with the Person Centered Plan. Update the Person-Centered Plan/Individual Service Plan and crisis plan as issues arise. Communicate with the Care Coordinator about the needs of individuals that you support Notify the Care Coordinator of any changes, incidents or other information of significance related to the individual supported. Provide progress reports throughout or at the end of the treatment year as applicable. CenterPoint’s responsibility to providers is to conduct the following activities for clients who are receiving care coordination: Assessment: I/DD Care Coordinators will complete or arrange for needed assessments to identify support needs and to facilitate ISP / person centered planning processes. MH/SA Care Coordinators will complete or arrange for needed clinical assessments for clients who have special health care needs in order to identify any ongoing special conditions that require treatment or monitoring. Assuring the development of a person centered plan: I/DD Care Coordinators will develop the ISP long term goals on the Person-Centered Plan/Individual Service Plan in collaboration with the individual and his/her support team. I/DD Care Coordination will assure that requirements of the Innovations Waiver, B3 services, and State Funded services are explained where applicable and that an explanation of different services available to the client is provided. I/DD Care Coordination will assist the individual in requesting the chosen services and length of time those services are to be provided, including start and finish dates for each service and its associated cost, within the plan year. The I/DD CC will create a draft of the ISP that includes the services and duration desired by the client, and which will be signed by the client only after it is reviewed with the client. All questions are addressed and changes are incorporated. The client will sign a completed ISP. The I/DD CC will inform the client that the ISP can be changed during the year at the client’s request if service needs change. MH/SA Care Coordinators will assure that a Person-Centered Plan/Individual Service Plan is developed by the behavioral health clinical home. Treatment Planning Care Coordination: Both I/DD and MH/SA Care Coordinators will coordinate services for clients who have been identified as needing assistance to access the care that they need. Activities will involve working across the CenterPoint network and with other systems of care including primary care physicians. I/DD and MH/SA Care Coordinators may work collaboratively if and when a client has needs in both service areas. It is the responsibility of Care Coordination to be sure that all providers serving a client are informed of all care needs. Monitoring: I/DD Care Coordinators will complete on-site visits to monitor the health and safety of the Client, to assess the satisfaction of Clients served, and to monitor implementation of the ISP. This Revised 7/21/15 21 can include review of paid claims and utilization of service throughout the plan year. Providers will work directly with Finance to resolve payment-related concerns. I. Community Operations CenterPoint’s Community Operations unit fosters open communication and cross-collaboration between the LME/MCO, the provider network, governmental agencies, law enforcement, clients, advocacy groups and other community stakeholders. Under the guidance of the Community Operations Director, the department coordinates initiatives that build and strengthen evidence-based/best practice service continuums, and supports the development of community-based prevention and outreach programs to address issues such as juvenile delinquency, substance abuse and homelessness. Community Operations employs specialists with expertise in public relations, communication, housing, client rights, NC mental health court processes and juvenile justice, peer support and recovery, and System of Care. The department manages CenterPoint’s cultural competence initiative, provides liaison duties and support to the LME/MCO’s Consumer and Family Advisory Committee (CFAC) and collaborates with various advisory groups, including the Mental Health/Substance Abuse and I/DD Advisory Committees. In addition, the department develops and manages Wellness Centers across the catchment area to promote whole person health. Your responsibilities as a CenterPoint Contracted Provider are to: Seek opportunities to participate with other community stakeholders in prevention, education and outreach programs Disseminate educational materials to increase awareness and reduce the stigma associated with mental health disorders, intellectual and developmental disabilities and substance abuse issues Participate in the education of stakeholders and clients on system access, services and community resources, appeal and grievance processes, advanced directives, and the provider network Acquire knowledge and an understanding of cultural competence; engage in initiatives to achieve cultural competence and provide services in a culturally competent manner CenterPoint’s responsibilities to providers are to: Work with community stakeholders to develop prevention, education and outreach programs Disseminate public information that is accurate and timely Promote and support cultural competency throughout the provider community and encourage adherence to best practice standards for service delivery Lead community collaborative efforts to assess community capacity and identify needs and service gaps Develop and publish informational materials for providers and clients Partner with the community to prevent and reduce juvenile delinquency, chronic homelessness and substance abuse Build and expand an integrative System of Care for children and their families Provide the www.cphs.org website with up-to-date information about CenterPoint for clients, providers, key stakeholders and the general public Revised 7/21/15 22 J. Client-Related Functions CenterPoint’s The Consumer Affairs Specialist (CAS) Initiates and participates in activities that promote and support the empowerment of clients including participation in community education and the development of educational materials. This position is engaged in client rights protection activities. Your responsibilities as a CenterPoint contracted provider are to: Publicize and support LME/MCO-sponsored opportunities for client training Participate in state and LME/MCO surveys as requested Respond to inquiries from the CAS about client issues and concerns CenterPoint’s responsibility to providers is to: Serve as a liaison to local and state organizations that promote client rights and integration into the community Work with community stakeholders to reduce the stigma and discrimination associated with mental illness, developmental disabilities and/or substance abuse issues Serve as a resource for development of peer support Provide information for clients to make complaints and grievances Assure that client interests are represented throughout the LME/MCO on the Board, the Consumer and Family Advisory Committee, Waiver Advisory Committees, I/DD and MH/SA Advisory Committees, the Human Rights Committee, the Finance Committee, the Clinical Advisory Committee and the Quality Improvement Committee. Be a resource for evidenced based practices and emerging best practices with the goal of improving positive outcomes in the community and the client’s quality of life and progress in recovery K. CenterPoint Chief Clinical Officer/Medical Director CenterPoint’s Medical Director is the Chief Clinical Officer for the CenterPoint LME/MCO. The CCO/Medical Director is a board-certified psychiatrist. The CenterPoint Medical Director is responsible for the overall clinical management of services to clients including authorization of services and utilization management, and is responsible for the overall quality management program. Other activities include oversight of the provider credentialing process, and collaboration with CenterPoint network providers, medical providers in the community, state and community hospitals, as well as development of preventive health projects for CenterPoint clients. L. Stakeholder Involvement in CenterPoint System Management CenterPoint has a comprehensive system of operational forums that assure engagement of clients, family members, advocates, providers and community agencies. Operational committees bring together CenterPoint staff, clients/family members, providers and stakeholders to address issues, provide important feedback to CenterPoint regarding its performance and assist in proactive planning. M. Waiver Advisory Committee CenterPoint established two committees for the purpose of offering input into the LME/MCO’s startup, implementation and effective management of 1915 (b)/(c) Medicaid Waivers. The Mental Health/Substance Revised 7/21/15 23 Abuse (MH/SA) Waiver Advisory Committee and the Intellectual/Developmental Disabilities (I/DD) Waiver Advisory Committee are comprised of representatives from CenterPoint’s catchment area. Membership includes providers, clients, family members, hospital and community agency representatives and advocates. N. Operational Committees The chart below illustrates the relationships and interactions of CenterPoint’s Operational Committees. These Committees provide forums for CenterPoint, clients, family members, providers and other community stakeholders to exchange information and ideas, address problems, and develop plans. Operational Committees help CenterPoint stay focused on the mission and understand the impact of our activities. For the members, these committees have afforded opportunities to understand and assist CenterPoint with the requirements and challenges of its role as LME/MCO. We expect that these groups will continue to grow and positively impact CenterPoint operations and management. Revised 7/21/15 24 Cross-Functional Team Relationships Board Committees: - Executive Committee - Finance Committee - Human Rights Committee - Global Continuous Quality Improvement Committee (GCQIC) Consumer & Family Advisory Committee (CFAC) Board Corporate Compliance Committee CEO Health & Safety Committee Executive Team Clinical Advisory Committee Quality Operations Team Clinical Operations Team Credentialing Committee Quality Management CFT Care Management CFT Financial Operations CFT Integrated Care Committee I/DD Advisory Committee MH/SA Advisory Committee Waiver Advisory Committee – I/DD Waiver Advisory Committee – MH/SA Revised 7/21/15 Network Management CFT Consumer & Community Affairs (Cultural Competency) CFT CenterPoint Area Providers Council (CAPC) Business Processes & Decision Support CFT Forsyth County SOC Collaborative Stokes County SOC Collaborative Davie County SOC Collaborative Rockingham County SOC Collaborative Jail/Mental Health Task Force 25 SECTION III: PROVIDER NETWORK A. The CenterPoint Provider Network The NC MH/DD/SAS Health Plan, as a managed care Waiver, allows CenterPoint flexibility in managing the size and scope of its provider network. The LME/MCO must assure client choice and accessibility of services. However, the managed care Waiver allows CenterPoint to right-size the network in areas of excess capacity. This is important to assure economic viability of providers and efficient delivery of services. CenterPoint encourages provider expertise in evidenced-based practices so that the service system will be better able to meet the needs of individuals served. CenterPoint completes annual needs assessment, geographic access and capacity study leading to generation of a Network Development Plan. The purpose of these studies is to evaluate the capacity of the enrolled provider network to meet the needs of the people served and to measure geographic access to provider locations. The studies inform CenterPoint decisions on whether to add or limit capacity. Additionally, utilization initiatives inform the annual capacity study. For example, initiatives may be established to reduce residential treatment for children while increasing the use of community services. The availability of community services is continually monitored to assure that there is adequate network capacity to meet any increased demand. CenterPoint has a detailed Credentialing Plan outlining the delegated responsibilities via a delegated contract with Smoky Mountain Center (SMC) to conduct the Primary Source Verifications (PSV) required by Utilization Review Accreditation Commission (URAC), Department of Health and Human Services (DHHS), which includes the Division of Medical Assistance (DMA) and the Division of Mental Health, Developmental Disabilities and Substance Abuse (DMH/DD/SA) for the Credentialing process. CenterPoint’s Credentialing Committee, or its designee, reviews all initial and re-credentialing applications for participation in the network. B. Cultural Competency of the Network Historically, CenterPoint has been diligent in its efforts to maintain a workplace that is culturally diverse and free of discrimination in all hiring and business practices. CenterPoint’s internal policies and procedures reflect the principles of state and federal human/civil rights legislation, the Americans with Disabilities Act (ADA) and the Health Insurance Portability and Accountability Act (HIPAA). Over the past decade, globalization of the economy has resulted in changing demographics for many regions of North Carolina, including Forsyth, Stokes, Davie and Rockingham Counties. The 2010 census revealed increases in older and Hispanic populations in CenterPoint’s catchment area. Society has become increasingly aware that cultures are not solely defined by race, age or ethnicity. CenterPoint has recognized the need to broaden its perspective on cultural competence. In 2011, CenterPoint formed a Client and Community Affairs Cross-Functional Team (CFT) that examines cultural competence and language literacy within the organization and throughout the provider network. The CFT, which meets regularly and is led by the Community Operations Director, includes representation from Human Resources, Community Operations, Network Management, Care Revised 7/21/15 26 Coordination and Administration. With input from CFAC and the CenterPoint Area Providers Council, the group is responsible for ongoing development and implementation of a Cultural Competency Plan that includes a work plan for implementation over the next three years. C. Types of Network Providers Agency Provider: An agency is a provider that delivers enhanced services (as defined by NC Division of Mental Medical Assistance Clinical Coverage Policy 8A). For purposes of this manual, agencies are divided into two categories: CABHAs and Specialty Providers: Critical Access Behavioral Healthcare Agency (CABHA) Provider: A Critical Access Behavioral Health Agency (CABHA) is a category of provider agency that delivers a comprehensive array of mental health and substance abuse services. The role of a CABHA is to assure that critical services are delivered by a clinically competent organization with appropriate medical oversight and the ability to deliver a robust selection of services. CABHAs assure client care is based upon a comprehensive clinical assessment and services appropriate to the population. CABHAs are required to offer the following core services: Comprehensive Clinical Assessment, Medication Management and Outpatient Therapy. As of December 31, 2010, CABHAS are the only type of providers that deliver Community Support Team, Intensive In-Home, and Child/Adolescent Day Treatment Services. Specialty Provider: Specialty providers are providers that specialize in a specific service (such as vocational or residential), in serving a specific disability area or both. Specialty providers are important components of the network because they can focus their efforts on best practice strategies for a specific population. The majority of LME/MCO providers are specialty providers. These providers offer best practice service options to clients such as Assertive Community Treatment Team, Multi-systemic Therapy, Mobile Crisis, and Innovations Waiver Services. In addition to agency providers, the CenterPoint network also includes the following kinds of providers: Alternative Family Living (AFL) Provider: AFL services must be provided by agency providers. CenterPoint requires the following for AFL providers: 1. Documentation of training and background checks for both primary staff and back up staff. 2. The AFL site must be the primary residence of the AFL provider (a couple or a single person) who receives reimbursement for cost of care. 3. Any provider offering services outside the scope of the AFL compensation and/or requirements must be an employee of the agency provider. 4. If the AFL serves more than one client or a client less than 18 years of age, the site must be licensed by the NC Division of Health Services Regulation (DHSR). 5. A backup staffing plan must be in place and the backup staff must be employees of the provider. 6. AFL providers must submit to Health and Safety Reviews which are to be completed annually. Revised 7/21/15 27 7. AFL providers are not permitted to provide services to another client while serving a primary client for AFL services at an unlicensed site. 8. AFL providers will be required to pay back funds if a client is moved to a new site and CenterPoint is not notified and the AFL provider bills for the old site. 9. AFL providers must have insurance coverage for automobile; personnel files must be maintained on all AFL providers; and all documentation for service provision must meet APSM 45-2, APSM 45-1, HIPAA and service definition requirements and be readily available for review upon request. Licensed Practitioner and Professional Practice Group: This provider category includes Medical Doctors (M.D.) practicing in behavioral health; doctorate level practicing Psychologists (Ph.D.); Master’s level Licensed Psychologist Associates (LPA); Master’s level Licensed Clinical Social Workers (LCSW); Licensed Marriage and Family Therapists (LMFT); Licensed Professional Counselors (LPC); Licensed Clinical Addiction Specialists (LCAS); Advanced Practice Psychiatric Clinical Nurse Specialists; Psychiatric Nurse Practitioners (PNP); and licensed Physician Assistants (PA) who are members of the provider network and bill under their own license. Network providers must meet CenterPoint criteria for credentialing, enrollment and contracting. CenterPoint assures that each provider has the appropriate training and experience along with a history of offering quality care. Additionally, CenterPoint collects information about the specific expertise of these providers in order to help clients make choices about providers. Associate-Level Licensed Provider: Practitioners who are associate-level licensed providers) in NC and are employed by an agency that is fully contracted with CenterPoint to provide outpatient treatment may submit an application for participation in the CenterPoint provider network. Supporting materials must include documentation of clinical supervision. Provider Network Status: 1. Out of Area Provider: a contracted Licensed Independent Practitioner, agency or hospital, providing behavioral health services outside of the CenterPoint catchment area counties. Such providers meet all network requirements and are considered to be full members of the CenterPoint Network. 2. Out-of-Network Provider: CenterPoint procedures address the process utilized to determine the need for a client-specific agreement or contract with providers outside of the CenterPoint network. Some clients with Medicaid from CenterPoint counties live in other parts of the state. CenterPoint is committed to assuring that providers are available to meet their needs and thus, make arrangements for client-specific agreements and contracts. A client’s need for out of catchment, community-based services may be identified by Utilization Management, Care Coordination, Network Development or Customer Services. The CenterPoint Medical Director reviews client information submitted to assist in determining medical necessity and the need for a client-specific agreement. Out-of-network providers are fully credentialed but are not considered to be members of the CenterPoint network, are not able to receive additional client referrals, and are not included in provider website listings. Revised 7/21/15 28 3. Non-Enrolled, Non-Contracted Provider CenterPoint will pay for acute behavioral emergency care for a CenterPoint Client by a non-enrolled, non-contracted provider. An out-of-network Emergency Department and/or inpatient service (out-of-catchment AND out-of-network Provider) can utilize the one page form available on the CenterPoint website for reimbursement. When a client in the NC MH/DD/SA Health Plan resides outside of the CenterPoint region, CenterPoint will work collaboratively with the client and providers in that area to assure that the client has access to needed services. D. Location of Providers CenterPoint establishes access standards for community-based services: urban (30miles/30 minutes’ drive time), rural (45 miles/45 minutes’ drive time). While most services are available within these standards, some specialty providers may be located outside the person’s county of residence. There may be only one provider of facility-based services, such as Psychosocial Rehabilitation in a county, due to insufficient demand to support two providers and economy of scale factors. CenterPoint will annually evaluate the location of providers and types of services in its capacity study, and determine the need for additional providers. CenterPoint also maintains client/provider mapping capability which allows CenterPoint to associate location of providers in relation to where clients live within the catchment area. E. Quality of Care CenterPoint’s responsibility is to assure the quality of services provided by the CenterPoint provider network. CenterPoint is accountable to the Division of MH/DD/SA and the Division of Medical Assistance in the management of both state and Medicaid services and funds. In addition to state requirements, Medicaid Waiver quality requirements are extensive and include: Health and safety of clients Rights protection Provider qualifications Client satisfaction Management of complaints Incident investigation and monitoring Assessment of outcomes to determine efficacy of care Management of care for Special Healthcare Needs populations Preventive health initiatives Clinical best practices (LINE 20) and clinical guidelines developed and approved by CenterPoint CenterPoint has numerous quality, satisfaction and financial reporting requirements related to contracts with the Division of MH/DD/SA and DMA. A Cross Functional Team (CFT) evaluates CenterPoint performance annually. A team composed of representatives of DMA and the Division of MH/DD/SA conduct quarterly oversight review; annually, a state-contracted vendor also participates in the reviews of each LME/MCO as required by Medicaid regulations (referred to as External Quality Review Organization (EQRO). CenterPoint understands the important role of quality management in protecting clients and in promoting quality of care. Revised 7/21/15 29 As part of the Continuous Quality Improvement process, CenterPoint operates a Global Continuous Quality Improvement Committee (GCQIC). This Committee includes CenterPoint staff, client/family representative(s) and provider representation, striving to include all disabilities/counties. The purpose of the Committee is to assure cooperation and collaboration to achieve system improvements and to monitor the overall quality of services. CenterPoint alone cannot maintain quality, thus this partnership is critical for success. The Quality Management CFT develops a single Quality Management Program Description/Plan (QMPD/P) for the CenterPoint network with input and feedback from the GCQIC and other relevant stakeholders. The plan identifies strengths, weaknesses and areas of improvement and includes a program description, work plan and annual report. Your responsibility as a CenterPoint Contracted Provider is to: Assure clients meet medical necessity requirements for all services that your agency provides Provide medically necessary covered services to clients as specified in your contract and authorized by CenterPoint Strive to achieve best practice in every area of service Provide culturally competent services and assure the cultural sensitivity of staff members Develop a cultural competency plan and comply with cultural competency requirements Have a clinical backup system in place to respond to emergencies on weekends and evenings for people that you serve, or serve as a first responder as outlined in the service definition and your contract Demonstrate client-friendly services and attitude; network provider must have a system to assure good communication with clients and families Comply with the policies and procedures outlined in this manual, any applicable supplements, CenterPoint Communications Bulletins and your provider contract, the General Conditions of the Procurement Contract, applicable state and federal laws and regulations Provide services in accordance with all applicable state and federal laws Provide services in accordance with access standards and appointment wait time as noted in the General Conditions of the Procurement Contract including criteria fort emergent/urgent and routine referrals and criteria that walk in clients are seen within two (2) hours of arrival and client’s with scheduled appointments are seen within sixty (60) minutes of the appointed meeting time Have a “no reject” policy for clients who have been determined to meet medical necessity for the covered services provided by your agency or as a Licensed Independent Practitioner Work with CenterPoint to assure a smooth transfer for any clients that desire to change providers or for whom a transfer is clinically appropriate because you cannot meet his/her special needs or, for any reason, will no longer participate in the CenterPoint provider network Document all services provided as per Medicaid Requirements, NC Waiver Requirements and North Carolina State Rules Agree to cooperate and participate with all utilization review/management, quality management, review, appeal and grievance procedures Comply with the credentialing and/or enrollment procedures and processes of CenterPoint and DMA Comply with authorization and Utilization Management requirements of CenterPoint Revised 7/21/15 30 Comply with the re-credentialing or re-qualifying procedures of CenterPoint Participate in client satisfaction surveys, provider satisfaction surveys, clinical studies, incident reporting, and outcomes requirements Manage client records in a manner consistent with the contract and/or any relevant statues governing such records upon termination of the CenterPoint provider contract, regardless of the reason for contract termination. Per the provider contract with CenterPoint, the following applies: In the event that Provider is terminating its business in NC, the Provider is to provide CenterPoint with the original client records of any Medicaid or state funded client served by Provider. Records should be submitted to CenterPoint within sixty (60) days of contract termination. In the event that the provider plans to continue delivering services in NC, the provider may, at the discretion of the CenterPoint Network Operations Manager, store records in a secure site maintained by Provider as outlined in a written plan requiring CenterPoint approval. Records shall include but not be limited to: a minimum of progress notes that inform of the most recent contacts with a client; any information related to the provider’s efforts to engage the client with an alternate provider of his/her choice; medication management information; a copy of the most recent comprehensive clinical assessment; a copy of the most recent PCP/ ISP updates; any psychiatric or psychological evaluations; up to date demographic information; and any other records required to be maintained. CenterPoint’s responsibility to Network Providers is to: Provide assistance twenty-four (24) hours a day, seven days a week to clients, and potential clients including crisis coordination Assist providers in understanding and complying with CenterPoint policies and procedures, applicable policies and procedures of the Department of Health and Human Services and federal agencies including the Centers for Medicare and Medicaid, as well as the requirements of our accreditation agencies including, but not limited to URAC Provide technical assistance related to CenterPoint contract requirements, CenterPoint Provider Manual requirements, Department requirements of providers, the development of appropriate clinical services, quality improvement initiatives, or to assist the provider in locating sources for technical assistance. CenterPoint is not required to provide technical assistance in areas that would normally be considered standard operational activities of a provider agency or to providers that have shown by history not to be able to assimilate previous technical assistance provided CenterPoint will make available to providers, the results of its capacity study which identifies provider under/over capacity as well as priorities for Network Development. CenterPoint is not required to contract with providers beyond the number necessary to meet the needs of its clients. F. Provider Communication CenterPoint is committed to communication through a variety of means in an effort to keep the community of network providers well informed of state or federal changes, new information, trainings, request for proposals and opportunities for collaboration. CenterPoint maintains a “Provider” section on the website that includes specific information for providers. Additionally, CenterPoint disseminates critical and time sensitive information through official CenterPoint Provider Alerts or communication Revised 7/21/15 31 bulletins and through the use of CenterPoint’s weekly electronic newsletter, The Friday Email. Provider Alerts, and many other documents are also posted on the CenterPoint website. CenterPoint also maintains information on its website for clients, including a searchable list of providers so that clients can search for providers by various factors. CenterPoint has incorporated providers into multiple aspects of operations to assure that management activities will be efficient and effective. Some of these forums include: The CenterPoint Area Providers Council and its Steering Committee Waiver Advisory Committees Ad hoc work groups Provider Forums/meetings Training activities Hands-on technical assistance with billing and other functions through Alpha computer system It is CenterPoint’s intent to communicate regularly with providers through these forums, email updates, and other communications. The training activities offered are intended to support providers’ efforts to attain the skills that are important for quality service provision. Your responsibility as a CenterPoint Network Provider is to: Keep apprised of current information through the communication offered and provide services as specified in the most recent State standards or Waiver service definitions Attend and participate in provider meetings Review the web site for updates on a regular basis at www.cphs.org Review the websites for most up to date information on a regular basis o www.dhhs.state.nc.us/mhddsas o www.dhhs.state.nc.us/dma o www.cms.gov Work in conjunction with the appropriate Department at CenterPoint for technical assistance CenterPoint’s responsibility to you, the provider, is to: Offer provider meetings on a regular basis and post the schedule on the www.cphs.org website under the “Calendar” tab Post electronic updates on the provider page Post official network communications on the CenterPoint website Send written correspondence via the mail as needed Assign a Provider Relations Specialist to each provider to function as a Provider Liaison, serving as the main point of contact to respond to individual provider needs Respond to provider inquiries and provide feedback in a timely manner Revised 7/21/15 32 G. CenterPoint Area Providers Council The CenterPoint Area Providers Council (CAPC) was formed in 2006 as a self-governing group operating under its own bylaws. The list of current officers and membership and minutes of joint meetings between the CAPC Steering Committee and CenterPoint are posted on the CenterPoint website. The objectives for which this Council is formed are as follows: 1. To review materials and advise CenterPoint regarding planning, goals, and objectives of the network 2. To review network performance 3. To review and make recommendations to CenterPoint regarding performance indicator selection and performance issues, including outliers 4. To review reports and make recommendations on mutually identified areas of services and provider network performance (e.g. provider outcomes; service utilization; capacity, gaps and needs ) 5. To suggest new service initiatives to address service gaps 6. To assess and provide for staff education and training needs within their agencies 7. To provide input on community and prevention needs 8. To suggest strategies to address funding and financial issues 9. To review and make recommendation regarding results of the provider satisfaction survey 10. To review the annual updates to the CenterPoint Provider Manual 11. To review the Provider Administrative Disputes and Provider Professional Competence Disputes procedures 12. The CenterPoint Area Providers Council is one of the key advisory committees of CenterPoint and, as such, has responsibilities to network providers in representing their interests and challenges, to clients and family members and to CenterPoint in responding to standards, key indicators, initiatives and requirements CAPC Provider Representatives: Representatives are selected by established processes set forth by the CenterPoint Area Providers Council and its bylaws. Representation typically includes both small and large providers and ideally includes the following provider types: Intellectual/Developmental Disabilities service providers Mental Health Adult service providers Mental Health Child service providers Substance Abuse service providers Comprehensive Providers (Critical Access Behavioral Health Agencies) Licensed Practitioners – Outpatient Services Hospitals CAPC Bylaws: The CenterPoint Area Providers Council Bylaws are developed by the Council and posted on the CenterPoint website. Revised 7/21/15 33 CAPC Code of Ethics: The CenterPoint Area Providers Council establishes and asks their members to adhere to a Code of Ethics developed by the group. Per CenterPoint procedure, provider representatives participate in the provider dispute resolution process through serving on review panels; scope of process includes disputes related to allegations. The CenterPoint Credentialing Committee is responsible for reviewing ethics violations or other infractions or sanctions that may affect network participation status of providers. The Credentialing Committee makes final decisions on network participation. H. Changes in Credentialing Status - Licensed Independent Practitioners, Agencies and Hospitals CenterPoint maintains a provider database with the current practice information submitted by Licensed Independent Practitioners (LIPs), agencies and hospitals in support to our ongoing commitment to our clients receiving quality care. Because this data is used for referral purposes, it is a network participation requirement that: Licensed Independent Practitioners, agencies and hospitals are to notify Network Operations Department in writing within one (1) business day of any changes in credentialed status, including but not limited to, the scope of the license, changes in privileged status at other organizations, pending malpractice claims. Licensed Independent Practitioners, agencies and hospitals are to notify Network Operations Department in writing within one (1) business day of any changes that impact credentialing, including but not limited to, such as change of address, change in ownership, discontinuation of services Licensed Independent Practitioners, agencies and hospitals shall notify Network Operations Department in writing within seven (7) days of personnel changes or information updates which may include, but are not limited to changes in capacity including inability to accept new referrals, addition of capacity or specialty services, address changes as well as changes in other enrollment information Licensed Independent Practitioners wishing to initiate a Leave of Absence shall notify the Credentialing Committee via the Credentialing Specialist in writing, no later than sixty (60) days prior to their desired effective date. Unless the leave is a result of disabling illness, a Licensed Independent Practitioner shall not request more than six (6) months in an initial Leave of Absence, with the option for an extension. An extension to the original leave is not to exceed an additional six (6) months and must be submitted no later than sixty (60) days prior to the expiration of the original Leave of Absence Providers and/or services will only be added based on identified need, on exception criteria specified in CenterPoint policies and/or procedures, and/or on provider performance. If approved, links will be forwarded to the provider to initiate the credentialing process. CenterPoint’s responsibility to providers is to: Update provider credentialing files and network databases in a timely manner to reflect new information provided Notify provider in writing if the change of information impacts on referral status Notify provider in writing credentialing committee decisions Revised 7/21/15 34 I. Re-Credentialing - Licensed Independent Practitioners, Agencies, Hospitals Providers (LIPs, agencies, and hospitals) in CenterPoint‘s provider network are required to have credentials re-reviewed and verified at a minimum of every thirty-six (36) months from the date of the last credentialing review for each practitioner. CenterPoint’s delegate, SMC, will complete the primary source verifications and the Credentialing Committee, or its designee, will approve re-credentialing applications. Your responsibility as a CenterPoint contracted provider is to: Complete, sign, and return your re-credentialing form and disclosure, complete with required materials as outlined in the notification (may include items such as attestation as to correctness/completeness and authorization for release of information and liability, including questions regarding physical and mental health status and lack of impairment due to chemical dependency/substance abuse loss or limitation of privileges and /or disciplinary activity and current malpractice converge) Provide current documentation as requested in the re-credentialing packet LIPs, agencies and hospitals must complete re-credentialing application materials within sixty (60) calendar days of the date of the re-credentialing notice As part of the re-credentialing process, each practitioner has the right: To review information collected during the re-credentialing process, except references and National Practitioner Data Bank (NPDB) results, upon request To be informed of the status of their re-credentialing application, upon request To be notified of information that is significantly different than reported by you and to have the opportunity to correct erroneous information in writing. Correction of the erroneous should be provided by the practitioner within two (2) weeks of notification on any discrepancies in the application To be notified about the credentialing decision within ten (10) business days of the Credentialing Committee's decision CenterPoint process for re-credentialing is as follows: Generate a monthly list of practitioners or providers requiring re-credentialing in six (6) months Review the quality of services provided and assure that the business needs of CenterPoint are satisfactorily met Automatically suspend from the network, any Licensed Independent Practitioner, agency, or hospital that has not returned the completed application within the designated time period of the original notification of re-credentialing Review the returned application materials for completeness and compliance with credentialing standards Issue to provider notification of re-credentialing status (determined by CCO review for “clean” re-credentialing materials or by Credentialing Committee, if there are items that need review) Revised 7/21/15 35 J. Alteration of Practitioner’s Credentialing Status CenterPoint maintains standards for Licensed Independent Practitioners’ participation that will assure competent, effective, and quality care to the patient population. CenterPoint maintains the rights to sanction, suspend, and/or terminate a practitioner for failing to maintain minimum credentialing requirements, and for activity, actions and/or non-actions which are contrary to CenterPoint’s standards of practice, DMA requirements, or relevant statutes. The following non-inclusive list of conditions can affect a practitioner’s credentialing status: LIP fails to maintain compliance with the credentialing and re-credentialing criteria LIP decides not to execute a practitioner contract LIP’s general area of practice or specialty, in the opinion of the Credentialing Committee, involves experimental or unproved modalities of treatment or therapy not widely accepted in the local medical community LIP has breached any material term of his/her provider contract, including failure to comply with medical management or Quality Improvement requirements Contact with a patient of a sexual or amorous nature, or violation of other clinician/patient boundaries LIP fails to maintain ethical standards outlined by the appropriate licensing board and/or state standards K. Reconsideration of Credentialing Decisions Pursuant to URAC standards, the Credentialing Committee has the final authority to approve or disapprove applications by providers for network participation status. The Committee’s decision to deny a credentialing application are final and not subject to dispute. Providers admitted to the network have the right to dispute the Committee’s decision to remove them from the network. L. Actions against Practitioner’s Credentialing Status Reported to External Bodies All disciplinary actions based on professional competency or conduct which would adversely affect clinical privileges for a period longer than thirty (30) days or would require voluntary surrender or restriction of clinical privileges, while under, or to avoid, investigation is required to be reported to the appropriate entity (i.e., State Medical Board, National Practitioner Data Bank, Federation of State Medical Boards, etc.). The CenterPoint CCO or designee is responsible for notifying all appropriate entities including State Medical Board, National Practitioner Data Bank, Federation of State Medical Boards, and the appropriate licensing bodies of the Board’s final determination. Revised 7/21/15 36 M. Changes in Enrollment/Contract Status CenterPoint is diligent in maintaining provider databases with current practice information submitted by providers in support to our ongoing commitment to our clients receiving quality care. Providers are to notify the Network Management Department in writing within one (1) business day of any changes in their status, including, but not limited to, licensure status, changes in privileged status with other accrediting organizations, pending citations and pending malpractice claims. Providers shall notify Network Management in writing prior to the following changes that impact credentialing status within the network: Changes in ownership Proposed changes in facility location or change of address Providers shall notify Network Management in writing within seven (7) days of personnel changes or information updates. This may include, but is not limited to the following: Change in management Changes in capacity Inability to accept new referrals Any proposed acquisitions Any proposed mergers Any pending investigations for Medicaid fraud N. Applying for Additional Services In order for a network provider to be considered for additional services: The provider must be in "good standing" which is defined as having a signed contract and all required submissions and/or reports up to date; and CenterPoint has established there is sufficient need for the service (s); and The provider must submit necessary forms and information required for review; and Any sanctions, including corporate compliance issues, the submission of a Plan of Correction, follow-up review, and/or established wait period following satisfactory implementation of a Plan of Correction, must be completed and verified by CenterPoint‘s Network Management Department CenterPoint will: Determine if there is an established need for a service(s) Post listing of identified services needed on website Within the listing of identified services needed, create a hyperlink to Requests for Information/Request for Proposals/ (RFP/RFI) or service description; create hyperlink to the “Provider Nomination Form” Monitor and gather “Provider Nomination” forms Revised 7/21/15 37 Review the performance record of the provider for quality citations, corporate compliance issues, actions that resulted in suspension of referrals, Division of Health and Human Services findings, Excluded Parties List System and other indicators of quality and best practice. Submit approved provider nominations to SMC to begin the credentialing process O. Health and Safety Site Reviews If a health and safety site visit is required for the new service, Network Operations shall schedule the site visit within thirty (30) days of the completed PSV by SMC. Any site requested to be added to the contract for the new service will be reviewed on all applicable areas. During the site visit, CenterPoint will evaluate the provider applicant’s readiness to provide services according to the requirements outlined in state regulations, the service definition and the CenterPoint contract. P. CenterPoint Network Development Plan The Network Development Plan is informed by and is a part of CenterPoint’s annual capacity analysis. The Network Development Plan is used to delineate priorities for service development as identified in CenterPoint’s Strategic Plan and annual needs assessment and capacity studies. Responsible CenterPoint Departments or Cross-Functional Teams are incorporated into the plan as well as accountability at the Senior and Executive management levels. Progress is monitored through regular reports at the Executive and Board levels of the agency. Q. Specialty Providers Specialty providers are providers that specialize in a specific type of service, e.g. residential, vocational or in a specific disability, or both. Most of the providers in the CenterPoint network are specialty providers. CenterPoint depends on specialty providers to engage in best practice and evidence based practices in the services they provide. Because these providers specialize in a type of service or disability, they are well situated to focus on best practice models of care and services. Many of the Medicaid State Plan service definitions include a “first responder” requirement as part of the service definition. This requires that providers have 24 hour on-call capacity and ability to respond face to face within 2 hours in the event a client in their care experiences a crisis. This means that clients have the advantage of having someone that knows them respond when they experience a crisis at any time. First responders provide immediate intervention when the individual and/or member of their support system initiate contact for assistance involving a psychiatric crisis or emergency. First responder providers will be available 24 hours a day, 7 days a week, and 365 days of the year. First responders are expected to answer calls immediately. No call to a first responder should be left unattended for more than 15 minutes. Revised 7/21/15 38 R. Licensed Independent Practitioners Licensed Independent Practitioners (LIPs) who work independently or in small group practices provide important access to outpatient care for clients. LIPs are required to maintain after-hours coverage to respond to their patients who need assistance. Licensed practitioners also provide services at agencies and hospital. S. Clinical Home for Clients The state Medicaid Service definitions implemented in March 2006 included the designation of a “clinical home” for clients. The role of the clinical home is further reinforced by the development of Critical Access Behavioral Health Agency model (CABHA). CABHAs provide the core clinical services that are needed to assure clients receive the continuity of services that they need. Expected outcomes for CABHAs functioning as clinical homes include: Single point of responsibility to plan, link and coordinate clinical and support services for clients Clinical accountability and development of Person-Centered Plans that reflect client needs “First responder” responsibility is clearly assigned Responsible for development of Crisis Plan and Advance Directive Team approach to planning and monitoring care. Team includes (as appropriate) psychiatrist, nurse, licensed professional, and peer specialist as well as staff from other provider agencies serving the person T. Network Design For clients with enhanced service needs, the clinical home provider develops a Person-Centered Plan that reflects both clinical treatment and support services. The clinical home provider links the client to services provided by other network providers, as well as to medical providers and other community agencies outside the CenterPoint network. The clinical home provider is be responsible for supporting the client in developing Crisis Plans or Advance Directives, and will assure that “first responder” services are provided. The clinical home provider also collaborates with primary care providers and assures that the person has a medical home if at all possible; for people without insurance, this may be difficult. Revised 7/21/15 39 SECTION IV: CONTRACTS Network providers are required to have a fully executed CenterPoint Contract which lists services and approved sites prior to delivery of services to a CenterPoint client. Network providers must first be credentialed by the Network Operation Department, then enter into a Contract before any services can be authorized or paid. The CenterPoint contract outlines the specifics for the provider type, the specific services and locations at which the provider may deliver the services, and related provisions. PLEASE NOTE: Providers will only be reimbursed for services at sites that are specifically listed in their contract, with the exception of basic benefit outpatient services which are not site specific/dependent. If the service is not in the contract the provider may not bill for it. CenterPoint may agree to amend the executed contract to add billable services and/or sites where warranted. The Network Development Department shall determine whether there is a need for additional services and whether the provider has capacity and ability to deliver those services. Provider requests to add services to an existing contract may be subject to Request for Proposal or Request for Information processes. There are four versions of the Contract, one for Intermediate Care Facilities (ICF/MR), one for hospitals, one for agencies and one for Licensed Independent Practitioners. The General Terms and Conditions section of the Contract describe the required compliances according to federal and state regulations, as well as CenterPoint’s Waiver participation agreement(s). The CenterPoint Provider Manual and the NC Innovations Technical Guide are incorporated into the contract by reference. All the CenterPoint Contract templates have been approved by the Secretary of the Department of Health and Human Services as required by NC G.S. §122C 142(a). A. Agency Contracts Your responsibility is to: Review your Contract for accuracy and execute the Contract by signing and dating it in all areas indicated and return to CenterPoint within fifteen (15) days of receipt. Contracts that are not signed in all areas, or that are received past the fifteen (15) day limit cannot be guaranteed payment for services. Request and have a fully executed CenterPoint Contract Amendment for any change to the original Contract. It is YOUR responsibility to report any changes in circumstance or needs to CenterPoint. Submit any required reports or data elements as required in the Contract to remain in “good standing”; submit reports as required in attachments and adhere to reporting requirements Understand the obligations and comply with all terms of the Contract and all requirements in the CenterPoint Provider Manual and NC Innovations Technical Guide. Notify CenterPoint of any prospective changes in identifying numbers (e.g. Tax ID, NPI, Medicaid Provider numbers, phone numbers) Assure that the contract and any addenda are fully executed and signed before any services are entered into the Alpha system If adding a site or services, confirm approval of CenterPoint’s Network Development Department before delivering new services or services at a new site Revised 7/21/15 40 If seeking to add a site, confirm credentialed status of the site by CenterPoint’s Network Operations Department before delivering services there Attempt to first resolve any disputes with other network providers or CenterPoint through direct contact or mediation Notify CenterPoint in advance of any mergers or change in ownership since it may have implications for your contract status with CenterPoint Provide to CenterPoint copies of all current licenses (professional and site/service), Certificates of Insurance, and tax identification numbers (IRS Form W-9) no later than 10 calendar days after expiration of any listed policy or license. Notify CenterPoint of any changes in licensed staff. Any and all Licensed Practitioners must be credentialed by CenterPoint. Meet all Performance Measures outlined in the executed contract, including fiscal, clinical and access measures as indicated. Providers will review the contract for specific measures. B. Licensed Independent Practitioner Contracts Licensed Independent Practitioners are required to have fully executed CenterPoint Contracts which list credentialed services prior to the delivery of services to a CenterPoint client. Your responsibility is to: Review your Contract for accuracy and execute the Contracts by signing and dating it in all areas indicated within fifteen (15) days of receipt. Contracts that are not signed in all areas or that are received past the fifteen (15) day limit cannot be guaranteed payment for services Request and have a fully executed CenterPoint Contract Amendment for any change to the original Contract. It is YOUR responsibility to report any changes in circumstance or needs to CenterPoint. Submit any required reports or data elements as noted in the Contract to remain in “good standing” Understand the obligations and comply with all terms of the Contract and all requirements in the CenterPoint Provider Manual and the NC Innovations Technical Guide Notify CenterPoint of any prospective changes in your legal practice name, the location of your practice site(s) or scope of practice and assure that your contract is amended prior to delivery of contracted services Attempt to first resolve any disputes with other network providers or CenterPoint through direct contact or mediation Notify the CenterPoint advance of any mergers or changes to your practice since it may have implications for your status as a CenterPoint provider Notify CenterPoint of any changes in licensed staff. Any and all Licensed Practitioners must be credentialed by CenterPoint Provide to CenterPoint copies of all current licenses (professional and site/service), Certificates of Insurance, and tax identification numbers (IRS Form W-9) Meet all Performance Measures outlined in the executed contract, including fiscal, clinical and access measures as indicated. Providers will review the contract for specific measures. Revised 7/21/15 41 CenterPoint will: Enter into client-specific agreements or contracts with providers in order to meet the needs of client who reside outside of the CenterPoint counties. (Note: Providers with client-specific agreements or contracts are not considered full members of the CenterPoint Network, are not posted on the CenterPoint website and are not available as choices for other clients.) SECTION V: CLIENT RIGHTS AND EMPOWERMENT A. Rights of Clients Free speech, religious freedom and personal liberty are fundamental American rights. Personal privacy and confidentiality of personal information are personal rights. When people receive services/supports in the state’s public system, there are additional rights too. State rules and state and federal laws spell out what these additional rights are. Client rights include, but are not limited to: To be treated with respect and due consideration of dignity – You have the right to be treated the way you feel you should when it comes to all aspects of the services provided to you throughout your wellness and recovery process. To privacy – You have the right to privacy under federal and state laws that protect the confidentiality of your personal information. Information can only be shared with others with your express consent. However, there are laws that allow exceptions. These exceptions are: a court order, an emergency, as part of an investigation of child abuse, and if you are determined to be a danger to yourself or others. To be protected from harm, abuse, neglect or exploitation – Your service provider’s employees are required to protect you from harm, abuse, neglect, or exploitation throughout your treatment process. Your provider is required to promote a safe and respectful environment by offering procedures that do not subject you to pain. To be free from any form of restraint or seclusion used as a means of coercion, discipline, convenience or retaliation – Only in cases where there is a danger of injury or harm to self or others can restrictive procedures be used. With this right you are also given safeguards against the use of medications that may present a serious risk to you. To choose your provider – You have the right to choose the agency that provides your services. Once you begin receiving services from a provider, you also have the right to seek services elsewhere if you wish. To an individual Person-Centered Plan – You have the right to a Person-Centered Plan tailored specifically to you. Through this plan you have the ability to set personal wellness, recovery and treatment goals, and you have the right to review your plan at any time. To receive information on available treatment options and alternatives presented to you in a manner appropriate to your condition and ability to understand. – Your treatment options should be shared with you. You should be allowed to ask questions when you don’t understand something. To participate in decisions regarding your health care – This includes being informed of your medications and treatment team recommendations. To refuse treatment. Revised 7/21/15 42 To be informed – You have the right to be informed of all policies and procedures that affect you as a client. All service providers are required to keep you informed of your rights, and each provider is also required to maintain documentation that each employee understands this process. To informed consent – You or your legal representative have the right to be informed in a manner that is understandable when it comes to the benefits, potential risks, and possible alternative methods of treatments. This also includes understanding the length of time the consent for services is valid, and the procedures to be followed if you or your representative chooses to withdraw consent. To understand how service payment will be covered – You have the right to a full understanding of how you, or outside sources will pay for or supplement your services. To file a complaint or grievance – You have the right to submit a formal complaint with CenterPoint. Call 1-888-581-9988 To request an appeal Non-Medicaid services – If your Non – Medicaid services have been denied, partially denied, reduced, suspended or terminated, you can file a request an appeal. To file an appeal call 1-888-581-9988 To request an Appeal for Medicaid services – If your service has been denied, partially denied, reduced, suspended or terminated, you can request Reconsideration Review within 30 days of such notice. This is the first step in the Appeal Process. To file an appeal call 1-888-581-9988 To request a State Fair Hearing – Within certain timeframes, if you disagree with the outcome of the Reconsideration Review, you can submit an appeal to the NC Office of Administrative Hearings and receive what is referred to as a “State Fair Hearing.” To request reasonable accommodations free of charge to you – You have the right to request physical accommodations for accessibility and language assistance including teletypewriter (TTY) services, sign language interpretation, interpretative services if you do not speak English and assistance for the visually impaired. To request and receive a copy of your medical record except as set forth by law. NCGS 122C-53(d) – Each treatment provider has policies and procedures you must follow to view your medical record. Your record can be withheld if your attending doctor determines there is information that would be injurious to your physical or mental well-being. To request your medical record be amended or corrected according to law. 45 CFR Part 164. CenterPoint uses and discloses member protected Individually Identifiable Health Information (IIHI) appropriately in order to protect member privacy. Members can request restrictions on use and disclosure of PHI. Members can request a report of disclosures of PHI. If at any time a member believes that their member rights have been violated, they may contact CenterPoint Consumer Affairs at 1-866-804-4323. Clients can also file a complaint by calling 1-888-581-9988 24 Hours a Day/7 Days a Week/365 Days a Year. A copy of member rights & responsibilities can also be found on the CenterPoint website at www.cphs.org. B. Civil Rights Per NC G.S. §122C 58, except as otherwise provided in the Chapter, adult clients are entitled to all civil rights including: To register and vote To buy or sell property, own property Revised 7/21/15 43 To sign a contract To sue others who have wronged them To marry or get a divorce To procreate and raise children Persons determined to be incompetent and that are assigned a court appointed guardian retain all legal and civil rights except those rights that are granted to the guardian by the court. The protection and promotion of recipient rights is a crucial component of the service delivery system. All clients are assured rights by law and it is expected that Providers will respect these rights at all times and provide clients continual education regarding their rights as well as support them in exercising their rights to the fullest extent. North Carolina General Statutes (NC G.S. §122C 51-67) and the North Carolina Administrative Code (APSM 95-2) outline specific requirements for notification of individuals regarding their rights as well as operational policies and procedures that assure the protection of rights. These statutes and regulations also outline the policy and operational requirements for the use and follow up of restrictive interventions and protective devices. It is expected that all Network providers are knowledgeable of all outlined statutes and regulations regarding client rights and the use of restrictive interventions/protective devices and that providers develop operational procedures that assure compliance. The provider is also expected to maintain an ongoing knowledge of changes to the statutes and regulations and immediately alter operations to meet changes. Each network provider agency is expected to maintain a Client Rights Committee consistent with regulations outlined in North Carolina General Statue and Administrative Code. Providers are required to maintain the minutes of their Client Rights Committee. Providers should de-identify any information that is not in relation to CenterPoint clients. CenterPoint maintains a Human Rights Committee that is responsible, as a sub-committee of the LME/MCO Board, for the monitoring and oversight of Provider Client Rights Committee functions. The CenterPoint Human Rights Committee receives routine reporting from CenterPoint staff on the use of restrictive interventions, rights violations and incidents of abuse, neglect and exploitation within the CenterPoint Network. Additional information for network providers working with clients is found throughout this Manual. Client Rights regulations are located in NC G.S. §122 C-51-67 and APSM 95-2 and APSM 30-1 and NCASC 27G.0504, 10A NCAC 27G.0103 C. Informed Consent A person receiving services has the right to be informed in advance of the potential risks and benefits of treatment options, including the right to refuse to take part in research studies. The person has the right to consent to or refuse any treatment unless: It is an emergency situation The person is not a voluntary patient Treatment is ordered by a court of law The person is under eighteen (18) years of age, has not been emancipated, and the guardian or conservator gives permission Revised 7/21/15 44 The Rights noted in this Manual are based on NC G.S. §122C, Article 3 and the Client Rights Rules, 10 NCAC 27C, 27D, 27E, 27F (APSM 95-2). CenterPoint reserves the right to have more restrictive policies and procedures than state and federal rules and regulations. D. Advocacy for Clients CenterPoint will not prohibit or otherwise restrict a health care professional acting within the lawful scope of practice from advising or advocating on behalf of a client who is his or her patient. CenterPoint will not: Restrict a provider from advocating for medical care or treatment options Restrict a provider from providing information the client needs in order to decide among all relevant treatment options Restrict a provider from providing information about the risks, benefits, and consequences of treatment or non-treatment options to the client Restrict a provider from providing information to the client about his/her right to participate in decisions regarding his or her healthcare, including the right to refuse treatment, and to express preferences about future treatment decisions E. Psychiatric Advance Directives (PAD) In 1997, North Carolina developed a way for mental health treatment clients to plan ahead for mental health treatment they might want to receive if they experience a crisis and are unable to communicate for themselves or make voluntary decisions of their own free will. A statutory form for advance instruction for mental health treatment is provided by NC G.S. § 122C 77 of the North Carolina General Statutes. An Advance Directive for Mental Health Treatment allows clients to specify in writing treatment preferences or instructions if they have a crisis in the future and become unable to make their own mental health treatment decisions. The PAD is not designed for people who may be experiencing mental health problems associated with aging, such as Alzheimer’s disease or dementia. To address these issues, a general health care power of attorney is used. A Psychiatric Advance document can include a person’s wishes about medications, ECT, or admission to a hospital, restraints, and whom to notify in case of hospitalization. The PAD may include instructions about paying rent or feeding pets while the client is in the hospital. The client could also put in an advance instruction “please call my doctor or clinician and follow his/her instructions.” That way if they are in an emergency room and unable to speak for themselves or confused, these instructions can be used as a means to help them at vital moments. The client must sign the Psychiatric Advance Directive for mental health treatment in the presence of two (2) qualified witnesses. The signatures must be acknowledged before a notary public. The witnesses may not be the attending physician, the mental health treatment provider, an employee of the physician or mental health treatment provider, the owner or employee of a health care facility in which the client is a resident, or a person related to the client or the client’s spouse. The document becomes effective upon its proper execution and remains valid unless revoked. Revised 7/21/15 45 If you are assisting a client in completing a Psychiatric Advance Directive, plan on several meetings to thoroughly think about crisis symptoms, medications, facility preferences, emergency contacts, preferences for staff interactions, visitation permission, and other instructions. Upon being presented with a Psychiatric Advance Directive, the physician or other provider must make it a part of the person’s medical record. The attending physician or other mental health treatment provider must act in accordance with the statements expressed in the Advance Directive when the person is determined to be incapable, unless compliance is not consistent with NC G. S. 122C-74(g). This statute contains the generally accepted practice standards of treatment to benefit the client, availability of the treatments or hospital requested, treatment in case of an emergency endangering life or health, or when the client is involuntarily committed to a twenty-four (24) hour facility and undergoing treatment as provided by law. If the doctor is unwilling to comply with part or all of the Advance Directive he or she must notify the client and record the reason for noncompliance in the patient’s medical record. Clients can choose someone they trust (like a family member) to make treatment decisions for them if they cannot make the decisions themselves. This surrogate decision maker has Health Care Power of Attorney and functions as an Agent to carry out instructions of PAD. If the client does not have a PAD, the health care agent must make mental health decisions consistent with what the agent, in good faith, believes to be the wishes of the principal. The health care agent must be competent, at least eighteen (18) years of age, and not providing health care to the client for remuneration. The agent is not subject to criminal prosecution, civil liability, or professional disciplinary action for any action taken in good faith pursuant to an advance instruction. Under the Health Care Power of Attorney a person may appoint a person as their health care agent to make treatment decisions. The powers granted by this document are broad and sweeping and cannot be made by a doctor or a treatment provider under NC law. The Psychiatric Advanced Directive and Health Care Power of Attorney legal forms were designed by Duke University. They are available electronically at http://pad.duhs.duke.edu or via the CenterPoint Human Services Consumer Affairs Specialist (1-888-581-9988). Additional information and forms are available via the North Carolina Department of the Secretary of State Advance Health Care Directive Registry at http://www.secretary.state.nc.us/ahcdr/Forms.aspx F. Confidentiality The Network Provider shall assure that all individuals providing services hereunder will maintain the confidentiality of any and all clients and other information received in the course of providing services hereunder and will not discuss, transmit, or narrate in any form any client information of a personal nature, medical or otherwise, except as authorized in writing by the client or his legally responsible person or except as otherwise permitted by applicable federal and state confidentiality laws and regulations including NC G.S. §122C, Article 3, which addresses confidentiality of all personal Revised 7/21/15 46 information acquired in attending or treating a client, and HIPAA, 42 U.S.C. §1201 et seq. (42 U.S.C. §1320d-2), including 42 CFR, Subchapter A, Part 2, which addresses confidentiality of records of drug and alcohol abuse patients. Information can be used without consent to help in treatment, for health care operations, for emergency care, and to law enforcement officers to comply with a court order (See also NC G.S. §122C-55). A disclosure to next of kin can be made when a client is admitted or discharged from a facility, but only if the client or his/her legal guardian has provided written consent. If the client disagrees with what a physician, treating provider, clinician or Care Coordinator has written in their records, the client can write a statement from their point of view that will be entered into the record, but the original notes will also stay for twenty-five (25) years. If a person applies for a permit to carry a concealed weapon in North Carolina, the person must give consent for the details of mental health and substance abuse treatment and hospitalizations to be released to law enforcement. Since there is no guarantee of adequate firewalls for electronic mail, CenterPoint staff and contractors cannot transmit e-mail with clients about their personal or health matters. Client related information should be communicated by paper mail, face to face, by telephone, or over a secure electronic connection. Confidentiality Rules (ASPM 45-1) were adopted in accordance with NC G.S. §150B-14C. Confidentiality and Privacy Practices are also based on the federal HIPAA regulations. Treatment of Minors Pursuant to the North Carolina General Statutes (NC GS 90-21.5), a minor (any person under the age of 18 who has not been married or who has not been emancipated) may give effective consent for medication services for the prevention, diagnosis and treatment of emotional disturbance and for abuse of controlled substances. Minors can access services by calling the CenterPoint ACCESS line. CenterPoint staff is trained to triage contact from minor, make appropriate referrals, and initiate crisis protocol where necessary. CenterPoint staff will ask the minor questions about the availability of parents/guardians with matters such as transportation and paperwork, but staff will limit access to help based on these factors. The minor seeking help may be directed to contact the provider to inquire about the provider’s specific requirements regarding the presence of parents/guardians. G. Second Opinion A Medicaid client has the right to a second opinion if the person does not agree with the diagnosis, treatment, or the medication prescribed. The CenterPoint Clinical Operations Department will arrange for a second opinion. Clients are informed of the right to a second opinion in the CenterPoint Client Handbook that is sent to them when the individual is enrolled. The role of the Network Provider is to be aware that this is a right of Revised 7/21/15 47 all Medicaid clients and refer the client to the Clinical Operations Department at CenterPoint if a second opinion is requested. H. Client Medicaid Appeals CenterPoint provides an internal system for client appeals that meets regulatory requirements. An appeal is a request for review of an “action” taken by CenterPoint. An “action” is defined as: a. b. The denial or limited authorization of a requested service (including the duration, type or level of service); The reduction, suspension, or termination of a previously authorized service; c. The denial, in whole or in part, of payment for a service; d. The failure to provide services in a timely manner; e. The failure of CenterPoint to act within the timeframes in 42 CFR 438.408(b). The client/guardian may file an appeal. A provider acting on behalf of the client and with the client/guardian’s written consent may file an appeal. Client/guardians can file an appeal with CenterPoint orally or in writing. However an oral appeal must be followed by a written and signed appeal unless the request is for an expedited review. Appeal requests must be made within thirty (30) days of the date of the Notice of Decision letter. Clients have a right to a State Fair Hearing; however consumers MUST exhaust the CenterPoint Reconsideration Review process before requesting a State Fair Hearing. The first step in the client appeal process to review an “action" is a “Request for Reconsideration.” Decisions to Deny, Reduce, Suspend or Terminate a Medicaid Service It is very important that providers understand the following rights so they may support the client/guardian’s request or make the request on the client’s behalf (must show written consent). If the treating physician/practitioner/provider would like to discuss the case with the CenterPoint UM department or the physician/psychologist, please call 1-888-220-5280. There are times when a client’s request for services is denied, and there are times when a current service is changed (i.e. terminated, reduced or suspended) by CenterPoint Utilization Management. Denial: A denial could occur if the criteria are not met to support a new authorization request for a service. Providers are notified of denials via the web portal. The client/guardian will receive a letter via U.S.P.S Certified Mail using a template approved by DMA. The letter will explain the action CenterPoint has taken, the reasons for the action, the client/guardians’ right to request a Reconsideration Review of the Revised 7/21/15 48 decision, the procedures for requesting a Reconsideration Review, the circumstances under which expedited resolution is available and how to request it, provide contact information and client rights information. The client is not eligible for Continuation of Benefits during a Reconsideration Review or Appeal process for new authorization requests (see Section J). If some services are approved, they will continue as long as they are authorized while the client appeals those that were reduced, denied or terminated. New services can also be requested during the appeals process. Reduction, Suspension or Termination: Services client is currently receiving may be reduced, suspended or terminated based on various factors including that clinical information provided does not support that service delivery follows clinical guidelines or that service request meets medical necessity for the frequency, amount or duration of the service. The client/guardian will receive a letter by U.S. Mail at least ten (10) days before the change occurs. The letter is on a DMA-approved template. The letter will explain the action CenterPoint has taken, the reasons for the action, the client/guardians’ right to request a Reconsideration Review of the decision, the procedures for requesting a Reconsideration Review, the circumstances under which expedited resolution is available, the client’s right to have benefits continue and the circumstances under which the client may be required to pay the costs of continued benefits. If the client/guardian desires continuation of services, the steps under section J, Client Reconsideration, “Continuation of Benefits” must be followed. I. Due Process regarding Medicaid Decisions Under The North Carolina Mental Health/Developmental Disabilities/Substance Abuse services Health Plan 1915(b), NC Innovations Home & Community Based Waiver 1915(c), all persons who do not agree with CenterPoint’s Notice of Decision on a request for Medicaid services, are entitled to a Reconsideration Review through the CenterPoint Reconsideration Review process. CenterPoint will consider the client, the client’s representative or estate representative of a deceased client as parties to the appeal. CenterPoint will provide reasonable assistance in completing forms and other procedural steps, including but not limited to, providing interpreter services and toll free numbers with TTY/TTD and interpreter capability. Information is provided in writing and can also be provided orally. If a client or guardian needs assistance with filling an appeal request they can contact CenterPoint’s Grievance and Appeals staff at 336-778-3633 during business hours or 1888-581-9988 24/7. CenterPoint would never retaliate against a client if a client chooses to appeal. Reconsideration must be completed before the client/guardian can request a hearing with the NC office of Administrative Hearings (OAH). Reconsideration Review Reconsideration is the first step in the Medicaid appeals process. It is a local impartial review of CenterPoint’s decision to take an action. The reconsideration decision is determined by a health care professional who has appropriate clinical expertise in treating the client’s condition or disorder and was not previously involved in CenterPoint’s initial decision. Revised 7/21/15 49 It can take up to thirty (30) days from the date the request for appeal is received for a decision to be made. CenterPoint may extend the timeframes by up to 14 calendar days if the client requests the extension; or if CenterPoint shows that there is need for additional information and how the delay is in the client's interest. Once CenterPoint is notified of the request for Reconsideration, the case is assigned to Grievance and Appeals staff. During the Reconsideration Review, the client/guardian may choose someone to represent them. The client/guardian has the right to review any information that was utilized as part of the clinical decision process. CenterPoint staff will acknowledge receipt of the request for Reconsideration to the client/guardian within one business day. All requests for Reconsideration are acknowledged by certified mail. If the client/guardian or provider makes an expedited appeal request, CenterPoint staff may acknowledge receipt orally (by phone). The CenterPoint Grievance and Appeals staff coordinates the due process and will be the primary contact person for the client/guardian or provider. If the client/guardian wishes to submit or have a provider submit additional information to be considered during the Reconsideration Review process it must be received by CenterPoint with 10 days of when CenterPoint received the request for a reconsideration review. CenterPoint will provide written notice of decision after the Reconsideration Review is completed. The written decision notice will include the decision and reasons for decision. For decisions not wholly in the client’s favor the notice will include the right to request a State Fair Hearing; how to request a State Fair Hearing; the right to continue to receive benefits pending a hearing; how to request the continuation of benefits; and if CenterPoint’s action is being upheld in a hearing, the client may be liable for the cost of any continued services. Steps to request Reconsideration Review: To request a CenterPoint Reconsideration Review, the client/guardian must complete and return the CenterPoint Reconsideration Request Form within thirty (30) calendar days (for continuation of benefits during the Reconsideration Review, Form must be submitted within ten [10] calendar days - see below “Continuation of Benefits Section”) by one of the following methods: • Fax 1-336-714-9394 • Mail (CenterPoint Human Services, Attn: QM Grievance and Appeals Coordinator, 4045 University Parkway, Winston Salem, NC, 27106); or • Deliver the form in person to CenterPoint Human Services 4045 University Parkway, Winston-Salem NC 27106; • Verbally by Phone during business hours (1-366-778-3633) – must be followed by written request; • Verbally by Phone outside of business hours (1-888-581-9988) – must be followed by written request. Continuation of Benefits Clients/guardians have a right to request continuation of benefits. CenterPoint must continue the service during the Reconsideration Review process and during the State Fair Hearing if all of the following are met: • The Reconsideration Review is requested within a timely manner, meaning on or before the later of the following: Revised 7/21/15 50 • • • • • o Within ten (10) days from the date of your notice of decision letter or o The intended effective date of CenterPoint’s proposed action The Reconsideration Review request involves the termination, suspension, or reduction of a currently authorized service (does not apply to new services being requested) The service was ordered by an authorized provider The original period covered by the original authorization has not yet expired The client/guardian requests the extension of benefits When a client/guardian files an appeal for the denial of a new service, CenterPoint is under no obligation to provide the requested service during the appeal process. If CenterPoint must continue services, the service must continue until: • The client/guardian withdraws from the Reconsideration Review process • The client/guardian does not request a State Fair hearing within ten (10) days of date CenterPoint mails an adverse decision after the Reconsideration Review process • A State Fair Hearing decision adverse to the consumer is made • The authorization expires or authorization service limits are met If the final appeal decision is not in favor of the client’s request, the client may be held liable for the cost of the services provided during the Reconsideration and/or State Fair Hearing process. If CenterPoint’s original decision is overturned, CenterPoint must authorize or provide the disputed services promptly and as expeditiously as the client’s health condition requires if the services were not furnished while the appeal is pending and if OAH or the State Fair hearing officer reverses a decision to deny, limit or delay services. CenterPoint or the state must pay for disputed services, in accordance with State policy and regulations, if CenterPoint or the State Fair Hearing officer reverses a decision to deny authorization of services, and the client received the disputed services while the appeal was pending. Expedited Appeal Review Process: An Expedited Appeal may be requested either orally or in writing by the client/guardian or a provider acting on behalf of a client. An expedited appeal will be conducted if it is indicated that taking the time for a standard appeal could seriously jeopardize the client’s life or health or ability to attain, maintain, or regain maximum function. If an expedited request is received, it is reviewed and it is reviewed to determine if there is sufficient evidence to support the need for this type of request. A review of decision will be completed within seventy-two (72) hours. Should the client/guardian or provider wish to present evidence and allegations of fact or law, they must do so within one (1) day of the expedited review request so that the case can be resolved as expeditiously as possible. CenterPoint may extend the timeframes by up to 14 calendar days if the client or provider requests the extension; or CenterPoint shows that there is need for additional information and how the delay is in the client's interest. The client/guardian will be notified of the decision. Revised 7/21/15 51 If there is not sufficient evidence to require an expedited request, the client/guardian or provider will be notified of the reason for denial of an expedited Reconsideration Review and the process will follow the normal reconsideration/appeal timelines. The client/guardian may appeal at the next level if there is disagreement of the initial expedite Reconsideration Review decision. To request an expedited appeal, call 1-888-220-5280. The client/guardian has the same rights for expedited appeals as regular appeals. The timeframe for action is different. CenterPoint will not take punitive action against a provider who either request an expedited resolution or supports a client’s appeal. CenterPoint will not retaliate against a client who chooses to appeal. The Appeals Process at State Level: Client/guardian must first utilize the CenterPoint Reconsideration Review process before proceeding to the State Fair Hearing process. If the client/guardian is not satisfied with the Reconsideration Review decision, he/she may submit an appeal to the NC Office of Administrative Hearings (OAH) within thirty (30) days from the date CenterPoint mailed the notice of appeal decision resulting from the CenterPoint Reconsideration Review process. Information and instructions on filing this appeal are included in notification of the Reconsideration Review decision. Pursuant to 42 CFR 408(f) the parties to the State Fair Hearing include CenterPoint as well as the client/guardian and his or her representative or the representative of a deceased client’s estate. The state must reach its decision within the timeframes specified in 42 CFR 431.244(f). Standard resolution is within ninety (90) days of the date the client filed the appeal with CenterPoint (excluding the number of days the client took to subsequently file for a State Fair hearing). Expedited resolution will be no later than three (3) working days after the agency receives CenterPoint notification of the appeal of a denied service that meets the criteria for expedited resolution, but was not resolved by CenterPoint; within the timeframe for expedited resolution, or was resolved within the timeframe for expedited resolution; but the decision was wholly or partially adverse to the client. Mediation: If the client/guardian wishes to appeal Reconsideration Review, the appeal must be filed within thirty (30) calendar days of that decision to the North Carolina Office of Administrative Hearings (OAH). After filing an appeal with OAH, the client/guardian will be offered the opportunity to accept Mediation. A mediator from the Mediation Network of North Carolina will be assigned to the case. The client/guardian may choose to have Mediation by telephone or in person. The client/guardian may bring information to support the need for services based on medical necessity. If the Mediation agreement is successful and agreeable to all present parties, the decision is binding and the process ends. If Mediation is declined, or it is unsuccessful, the appeal can proceed to a hearing at the Office of Administrative Hearings (OAH). This level of appeal is currently available through the State Fair Hearings process. Office of Administrative Hearings: If Mediation is declined or the Mediation is not successful, the client/guardian may proceed to the State Fair Hearing through OAH. Someone must be present at the hearing representing both parties. At the Revised 7/21/15 52 discretion of the Administrative Law Judge/hearing officer, parties may appear by phone but both sides must be available. Decisions are not usually made the same day as the hearing. After the hearing, an Administrative Law Judge will issue a decision and notify all parties. Requesting UM Criteria for Service Authorization: The Clinical Coverage policies for Medicaid services authorized by CenterPoint can be found at http://www.ncdhhs.gov/dma/Waiver/. If you do not have internet access or wish to receive a written copy of these documents, you may call 1-888-220-5280 to request a copy by mail. K. Non-Medicaid (IPRS) Service Appeal Process CenterPoint maintains a formal process to consider appeals of non-certification decisions by clients receiving IPRS funds. Expedited Appeals: Clients and providers have the right to an expedited appeal on any non-certification decision for urgent care cases; urgent cases are typically defined as those related to psychiatric hospitalization, partial hospitalization or detoxification where the life or health of the client would be jeopardized by a delay. Utilization Management staff coordinate and process expedited appeals with the LME/MCO Medical Director or contract psychiatrist. An expedited appeal decision will be made within 72 hours of the receipt of the expedited appeal request. Client and provider will be verbally notified and written notification will follow within 3 calendar days of the verbal notification of the decision. Standard Appeals: Clients have the right to a standard appeal on any non-certification decision for non-urgent cases. Requests to file an appeal may be made either verbally or in writing to Quality Management Grievance and Appeals staff within fifteen (15) calendar days of the date of the non-certification notification. Standard appeals are completed and written notification of the appeal decision is issued within seven (7) business days of receipt of the request for appeal. Reviewer determines the outcome of the appeal, the provider is notified electronically via the web portal; the client is notified through written notification. All Appeals: If CenterPoint’s original decision is upheld, the client/guardian will receive written notification of the decision and of their right to appeal the decision to the North Carolina Division of Mental Health, Developmental Disabilities and Substance Abuse Services (DMH/DD/SAS) within eleven (11) business days from the date of the notice. The notice of decision will include the Appeal Request Form and instructions for filing an appeal with DMH/DD/SAS. According to 10A NCAC 271.0608, the Division has sixty (60) calendar days from the date of the written request for appeal to send the panel findings and decision to the client. Once CenterPoint receives the panel decision from the Division, the outcome of this level of appeal, the final decision letter will be mailed to the client/guardian within ten (10) calendar days. Revised 7/21/15 53 Receiving Services during the Non-Medicaid Appeal Process: CenterPoint has the option of authorizing other Non-Medicaid Services that are appropriate. The duration of the authorization will be noted in the AlphaMCS system. Services may be authorized for the duration of the Appeal process at the discretion of CenterPoint. Other community resources may also be referred to the client for support. Note: When a client/guardian files an appeal for the denial of a new service, CenterPoint is under no obligation to provide the requested service during the Appeal process. L. Grievances Providers in the LME/MCO network must have a Grievance Process to address any concerns of the Client and the Client’s family related to the services provided. The provider must keep documentation on all grievances received including date received, nature of grievances, and resolution information. Any unresolved concerns or grievances should be referred to CenterPoint. The provider’s Grievance Process must be provided to all clients and families of clients. The provider must advise clients and families that they may contact CenterPoint directly about any concerns, complaints or grievances. Information regarding how to file a grievance can be found on the CenterPoint website. Callers may contact the ACCESS line at 1-888-581-9988. This information must be published and made available to the client and family members along with the telephone number of the Governor’s Advocacy Council. CenterPoint Grievance and Appeals staff will acknowledge receipt of each grievance, complaint or concern. The grievant has a right to remain anonymous if they choose. Anyone can report a concern, complaint or grievance including clients, guardians and providers, including complaints against CenterPoint. Grievances are resolved as quickly as possible; CenterPoint strives to have all grievance resolved within thirty (30) calendar days of receipt. CenterPoint may extend the timeframes by up to 14 calendar days if the client requests the extension; or if CenterPoint shows that there is need for additional information and how the delay is in the client's interest. CenterPoint may also receive grievances directly about a provider’s services or staff. Based on the nature of the grievances, CenterPoint may choose to investigate the grievance in order to determine its validity. Investigations may be announced or unannounced. It is very important that the provider cooperate fully with all investigative requests. Refusal to comply with any grievance follow-up or investigation is a breach of the provider’s contract. It is important to understand that this is a serious responsibility that is invested in CenterPoint, and that all grievances will be considered seriously until they are resolved. CenterPoint management of grievances is carefully monitored by DMA and CenterPoint maintains a database where all grievances and resolutions are recorded. CenterPoint maintains documentation on all follow up and findings of any grievance. A written summary will be provided to the grievant unless they chose to remain anonymous. If the grievance warrants a formal network investigation, the provider will receive a written summary of their findings. Plans of Correction may be required, depending on the findings. Revised 7/21/15 54 M. Human Rights Committee The CenterPoint Human Rights Committee (HRC) is a committee that reports to the CenterPoint Board of Directors and is charged with protecting the rights of clients under all applicable laws along with the Vision, Mission and Values of CenterPoint. The HRC meets at least quarterly and is comprised of up to twelve (12) members, including a CenterPoint Board member, with a majority being non-Board members. All reasonable efforts shall be made to have representation from the disability groups, client and/or family members and catchment county residents. • The CenterPoint Human Rights Committee works with the Board to oversee client rights protections including, but not limited to those specified in state and federal client rights laws, rules and regulations including the occurrence of incidents or deaths involving clients and client complaints involving violations and alleged violations of human rights. • The HRC reviews reports/data that have first been reviewed by the Quality Management Department for analysis and trending. The QM department works collaboratively with the HRC to identify service delivery system trends that are of concern. • The HRC will produce an annual report to be provided to the Board. • The Board Chair appoints the member of the HRC. When a vacancy occurs, the HRC Chair may seek recommendations from existing committee members and from CenterPoint community partners. The HRC Staff Liaison contacts the potential member(s) and solicits the completion of an application and conflict of interest form. Applications may be submitted to the Board Chair for appointment. All members serve at the pleasure of the Board Chair. Client Rights regulations are found in NC G.S. §122-C-51-67 and APSM 95-2 and APSM 30-1 and NCASC 27G.0504,10A NCAC 27G.0103 and DMH Communication Bulletin #30. N. Consumer and Family Advisory Committee Consumer and Family Advisory Committee (CFAC): The Consumer/Family Advisory Committee (CFAC) is comprised of clients of mental health, intellectual/developmental disabilities or substance abuse (MH/I-DD/SA) services and family members of clients of these services. CFAC members represent each county in CenterPoint’s catchment area and the three disability areas (mental health, intellectual/developmental disabilities, substance abuse). CFAC is a self-governing advisory committee to the CenterPoint Board of Directors. In compliance with North Carolina General Statute 122C-118.1, CFAC appointees also serve as voting members of the CenterPoint Board. Mission Statement: The Consumer and Family Advisory Committee shall act as an effective voice for the best interests of clients and their families from all disability groups throughout the catchment area, Revised 7/21/15 55 including Forsyth, Stokes, Davie and Rockingham Counties, regarding the public mental health, intellectual/developmental disabilities and substance abuse services system. Vision Statement: The Consumer/Family Advisory Committee supports the vision and guiding principles of the LME/MCO as approved by the LME/MCO Board. CFAC members are actively involved in CenterPoint’s oversight, planning and operational committees. CFAC members serve on the Board of Directors and the following committee: Finance, Human Rights, Global Continuous Quality Improvement and Clinical Advisory. CFAC is a strong voice at CenterPoint and in the community. Members are actively involved in collaborative initiatives, such as Cultural Competency, with CenterPoint staff and provide valuable feedback on the LME/MCO’s social marketing and communications efforts, client and community education and community outreach projects. SECTION VI: BENEFIT PACKAGE A. Eligibility The Provider must not employ any policy or practice that has the effect of discriminating against clients on the basis of race, color or national origin. B. Who is Eligible for the Medicaid Waivers? The NC MH/DD/SAS Health Plan (1915 b Waiver): The following criteria must be met for an individual to be eligible for inclusion in the Waiver: Individuals must have Medicaid in a covered eligibility group and have a county of residence for Medicaid eligibility purposes in Davie, Forsyth, Rockingham or Stokes County. Covered eligibility groups include: o Individuals covered under Section 1931 of the Social Security Act (TANF/AFDC) o Optional Categorically and Medically Needy Families and Children not in Medicaid deductible status (MAF) o Blind and Disabled Children and Related Populations (SSI) (MSB) o Blind and Disabled Adults and Related Populations (SSI, Medicare) o Aged and related populations (SSI, Medicare) o Medicaid for the Aged (MAA) o Medicaid for Pregnant Women (MPW) o Medicaid for Infants and Children (MIC) o Adult Care Home Residents (SAD, SAA) o Foster Care Children and Adoption o Participants in Community Alternatives Programs (CAP/DA, NC Innovations, CAP-C, CAP-MR/DD) o Medicaid recipients living in ICF-MR Facilities o Children are eligible beginning the first day of the month following their third birthday for 1915(b) services, but can be eligible from birth for 1915(c). Revised 7/21/15 56 The NC Innovations Waiver (1915 c Waiver): A person with I/DD and/or a related developmental disability may be considered for Innovations funding if all of the following criteria are met: The individual is eligible for Medicaid coverage, based on assets and income of the applicant whether he/she is a child or an adult The individual meets the requirements for ICF-I/DD level of care as defined by the NC Innovations Technical Guide for the ICF-I/DD Criteria Lives in ICF-I/DD facility or is at high risk for placement in an ICF-I/DD facility High risk for ICF-MR institutional placement is defined as a reasonable indication that individual may need such services in the near future (one month or less) but for the availability of Home and Community-Based Services The individual’s health, safety, and well-being can be maintained in the community with Waiver support The individual requires NC Innovations Services. The individual, his/her family, or guardian desires participation in the Innovations Waiver program rather than institutional services For the purposes of Medicaid eligibility, the person is a resident of one of the four counties within the CenterPoint region, Forsyth, Stokes, Davie and Rockingham Counties The individual will use one Waiver service per month for eligibility to be maintained. Individuals who are new participants to the waiver effective April 1, 2010 must live in private homes or facilities with six (6) beds or less that meet the Home and Community standards. A new participant is a person who was not enrolled in the NC Innovations Wavier as of April 1; 2008. Participants transitioning with their respective LME/PIHP from CAP-MR/DD to NC Innovations are not considered new participants for the purposes of waiver eligibility. The most current NC DMA Clinical Policy for the Medicaid C Waiver contains information about facility size requirements for individuals who are not new participants to the NC Innovations Waiver Must be on registry of unmet needs to be considered for waiver slot funding ICF-I/DD level of care is required for any individual under consideration for NC Innovations Waiver Funding. C. Medicaid Waiver Disenrollment When a client changes county of residence for Medicaid eligibility to a county other than Forsyth, Stokes, Davie and Rockingham, the individual will continue to be enrolled in The NC MH/DD/SA Health Plan until the disenrollment is processed by the Eligibility Information System at the state. Disenrollment due to a change of residence is effective at midnight on the last day of the month. A client will be automatically dis-enrolled from the NC MH/DD/SAS Health Plan if: The individual moves to a county other than the CenterPoint catchment area counties and their Medicaid county assignment also changes The individual is deceased The individual is admitted to a correctional facility for more than thirty (30) days The individual no longer qualifies for Medicaid or is enrolled in an eligibility group not included in the NC MH/DD/SAS Health Plan or NC Innovations 1915 (b)/(c) Waivers Revised 7/21/15 57 Is admitted to a facility that meets the definition of an IMD (Institution for Mental Disease) as set forth in 42 CFR 435.1010 as determined by DMA and is between the ages of 22 and 64. D. Eligibility for State Funded Services Clients that do not have Medicaid may be eligible for state-funded services based on their County of residence and level of need. State-funded services are not an entitlement and may be limited by the finite amount of funds available. CenterPoint and other LME/MCOs are not required to fund services beyond the resources that are available to them. There are also some services, including most residential services for adults that are not reimbursed by Medicaid but may be funded by state funds. Therefore clients who receive Medicaid may also receive state-funded services, based on their individual needs and availability of funding. CenterPoint maintains a Registry of Unmet Needs to track requests for state funding/nonemergency services that have not been met. Clients receiving Medicaid-funded services do not automatically qualify for state-funded services when Medicaid eligibility lapses for any reason. If the provider who has been providing Medicaid funded services also has a contract that includes non-Medicaid funding sources, the provider may request that the authorization be revised from Medicaid to non-Medicaid funding. If the provider does not have a nonMedicaid contract with CenterPoint, it is their responsibility to transition the client to a non-Medicaid provider that can meet the client’s needs. Authorization of state and other non-Medicaid funds is based on availability of funds, on funding sources identified in the provider’s contract and on the non-Medicaid benefit design. Non-Medicaid funded services are not an entitlement. E. Eligibility for Reimbursement by CenterPoint Clients who have their services paid for in whole or in part by CenterPoint must be enrolled in the CenterPoint system. If you have any questions about a client’s eligibility, please call the Customer Services line at 1-888-581-9988. Medicaid and state funds should be payment of last resort. All other funding options need to be exhausted first. Clients with a Medicaid card from Forsyth, Stokes, Davie or Rockingham counties are fully enrolled in the CenterPoint system and are eligible to receive Services which have been authorized by CenterPoint. CenterPoint and its providers shall use best efforts to report to the County DSS any known change to the household composition affecting the client’s eligibility for Medicaid including changes in family size, marital status or residence, within 5 days of the information being known. NOTE: Provider contracts specify the funding source available for provider billing. Providers should know if they have been contracted for Medicaid, State Services or both. If you have questions, please contact your assigned Provider Relations Representative. F. Enrollment of Clients It is important for all providers to assure client enrollment data is up-to-date based on the most current CenterPoint enrollment procedures and training. These documents can be found on the CenterPoint website at www.cphs.org under “Alpha Provider Training”. If enrollment data is not complete prior to service provision, authorizations and claims may be affected. This could result in denial of authorizations Revised 7/21/15 58 requested and/or claims submitted for reimbursement. (See Section IX “Finance” for additional information). Service Eligibility: Services are divided into multiple service categories: Basic Services: The Basic Benefit package includes those services that will be made available to Medicaidentitled individuals and, to the extent resources are available, to non-Medicaid individuals who meet Target Population criteria without prior authorization. These services are intended to provide brief interventions for individuals with acute needs. Any provider with an executed Procurement Contract with CenterPoint may provide the allowed unmanaged visits for any basic benefit service codes included in the contract without prior authorization. Effective June 1, 2014, outpatient therapy benefits (individual, family and group) will be unmanaged for children and adult Medicaid and state funded clients. Psychiatric services will be unmanaged for up to twelve (12) E & M visits for children and up to eight (8) E & M visits for adults. (Please note: CenterPoint does not manage NC Healthchoice (NCHC) benefits, therefore this information does not apply to NCHC clients.) To deliver outpatient services to Medicaid clients under the age of 21 the provider must obtain a referral from the individual’s primary care provider, a Medicaid-enrolled psychiatrist or from CenterPoint. The referral is demonstrated through documentation of the referring body’s NPI. The NPI and the referral must be maintained in the provider’s records. Basic Services: The Basic Benefit package includes those services that will be made available to Medicaidentitled individuals and, to the extent resources are available, to non-Medicaid individuals meeting State Benefit Plan criteria. With the exception of psychological testing, all basic outpatient benefits are unmanaged. Authorization for psychological testing must be obtained through CenterPoint’s Utilization Management Department prior to provision of services beyond the unmanaged benefit for Medicaid (8visits for adults/16 visits for children). Authorization is based on the client’s need and medical necessity criteria for the service requested. If outpatient therapy is to be provided in addition to enhanced benefits authorization is required. Enhanced Services: The Enhanced Benefit package includes those services that will be made available to Medicaidentitled individuals and, to the extent resources are available, to non-Medicaid individuals meeting State Benefit Plan criteria. Enhanced Benefit services are accessed through a personcentered planning process. Enhanced Benefit services are intended to provide a range of services and supports, which are more appropriate for individuals with more severe forms of mental illness, substance use and intellectual and developmental disabilities with more complex service and support needs as identified in the person-centered planning process. The person-centered plan/individual support plan also includes both a proactive and reactive crisis contingency plan. Enhanced Benefit services include services that are comprehensive, more intensive, and may be delivered for a longer period of time. An individual may receive services to the extent that they are identified as medically necessary through the person-centered planning process and utilization Revised 7/21/15 59 management review but may not duplicate services already authorized (for example therapy services for a client receiving ACTT services). The goal is to assure that these individuals’ services are highly coordinated, reflect best practice and are connected to the person-centered plan authorized by CenterPoint. Target Populations:State Benefit Plan: Target PopulationState Benefit Plan designation is for State funded services. It does not apply to clients who are only receiving Medicaid services. The provider must determine the specific State Benefit Plan for the client according to the criteria published by the Division of MH/DD/SAS. Each Benefit Plan is based on diagnostic and other indicators of the client’s level of need. In most cases, if the MH/DD/SAS system does not serve these individuals, there is no other system that will serve them. The MH/DD/SAS system is the public safety net and its resources will be focused on those most in need. To view the most current version of the State Benefit Plan Criteria: Go to one of the IPRS Website links on the NC Division of MH/DD/SAS link home page: http://www.ncdhhs.gov/providers/provider-info/health-care/nctracks G. Service Definitions (EQR II C 2.3) The regulations of a 1915 (b) Waiver require that all NC Medicaid State Plan services be available under the 1915 (b) Waiver. Providers should routinely visit the NC DMA website for current information, including detailed information regarding Service Definitions and the criteria for admission, continuation and discharge for each service. (EQR II C 2.3) H. Special Healthcare Needs Populations Defined in the NC MH/DD/SAS Health Plan Special Healthcare Needs Populations are population cohorts defined by specific diagnostic, functional, demographic and/or service utilization patterns that are indicators of risk and need for assessment to determine need for further treatment. The goal of the Managed Care Waiver is to first identify these individuals and intervene in order to assure that they receive both appropriate assessment and medically necessary services. Treatment Planning Care Coordination is a managed care tool that is designed to proactively intervene and assure optimal care for Special Healthcare Needs Populations. The Treatment Planning Care Coordination function is provided through the CenterPoint Care Coordination Department. CenterPoint Care Coordinators carry out this function in order to provide necessary support for individuals meeting the criteria defined below. The goal is to assure that clients are referred to and appropriately engaged with providers that can meet their needs, both in terms of MH/DD/SAS as well as medical care. Intellectual and/or Developmental Disabilities: CenterPoint may conduct care coordination for individuals who are functionally eligible for, but not enrolled in, the Innovations Waiver, or who are not living in an ICF-I/DD facility OR individuals with an intellectual or developmental disability diagnosis who are currently, or have been within the past thirty (30) days, in a facility operated by the Department of Correction (DOC) or the Department of Juvenile Revised 7/21/15 60 Justice and Delinquency Prevention (DJJDP) for whom the MCO has received notification of discharge. CenterPoint provides care coordination for all I/DD persons enrolled in a service that CenterPoint pays for. In addition, annual telephone contact is made with all individuals screened and found to be eligible for the I/DD Registry of Unmet Needs who are not enrolled in a paid service. Child Mental Health: Children who have a diagnosis within the diagnostic ranges defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) and its successors: 293-297.99 298.8-298.9 300-300.99 302-302.6 302.8-302.9 307-307.99 308.3 309.81 311-312.99 313.81313.89 995.5-995.59 V61.21 AND Current CALOCUS Level of VI, OR who are currently, or have been within the past thirty (30) days, in a facility (including a Youth Development Center and Youth Detention Center) operated by the DJJDP or DOC for whom the MCO has received notification of discharge. Adult Mental Health: Adults who have a diagnosis within the diagnostic ranges of: 295-295.99 296-296.99 298.9 309.81 AND A Current LOCUS Level of VI Substance Dependent: Individuals with a substance dependence diagnosis AND Current ASAM PPC Level of III.7 or II.2-D or higher. Opioid Dependent: Individuals with an opioid dependence diagnosis AND Who have reported to have used drugs by injection within the past thirty (30) days Co-occurring Diagnoses: Individuals with both a mental illness diagnosis and a substance abuse diagnosis AND A current LOCUS/CALOCUS of V or higher, OR Current ASAM PPC Level of III.5 or higher Individuals with both a mental illness diagnosis and an intellectual or developmental disability diagnosis AND Current LOCUS/CALOCUS of IV or higher Individuals with both an intellectual or developmental disability diagnosis and a substance abuse diagnosis AND Revised 7/21/15 61 Current ASAM PPC Level of III.3 or higher. Department of Justice Settlement: Individuals involved in the United States Department of Justice and North Carolina Settlement Agreement/Transitions to Community Living Initiative. I. Service Array For a listing of services, refer to the most current version of the service arrays by benefit level and disability. For Mental Health, Substance Abuse and Developmental Disabilities, further detail can be found in the Clinical Design Plan. For the NC Innovations Waiver, further detail can be found in the NC Innovations Technical Guide. All manuals can be accessed via the CenterPoint website at www.cphs.org. J. Medicaid Transportation Services Transportation services are among the greatest needs identified to assist clients in accessing care. It is CenterPoint’s goal to assist clients in accessing generic public transportation. Providers are requested to assist in meeting this need whenever possible. The Department of Social Services in each county has access to Medicaid approved transportation. Transportation is for medical appointments or getting prescriptions at the drug store. Riders have to call two (2) to four (4) days ahead to arrange a ride. There is no fee for clients who are enrolled in Medicaid. For those who are not enrolled in Medicaid, transportation depends on available space, and there is a fee. SECTION VII: CENTERPOINT CLINICAL DESIGN PLAN The North Carolina Mental Health/Developmental Disabilities/Substance Abuse Services Health Plan and the NC Innovations Waiver are important building blocks of the foundation of a reengineered system that will more effectively and efficiently address the needs of clients with mental illness, intellectual and/or developmental disabilities, and substance abuse disabilities. This system depends on coordination and management of all public resources available to support this system of care. Federal, State and County funds will be strategically managed for optimal outcomes for individual clients. Significant changes have begun and will continue to take place in a planned, controlled and sequential manner. Both external events and improvements in management strategies continue to result in refinement and improvements to our strategies. Our Goals: 1. To maintain a Clinical Model that is the foundation for all activities. This plan must be continually and consistently enforced through a variety of activities including Care Management, authorization, clinical protocols, application of culturally competent recovery principles and practices, utilization review, Care Coordination, Care Management, and provision of feedback/training to providers. 2. To develop a Self-Managed System by developing and training a selectively qualified and comprehensive network of providers. Revised 7/21/15 62 3. To use funding to encourage the development and provision of services that are based on clinical evidence, culturally competent and recovery practices, and which have proven desirable outcomes. 4. To involve clients and families in ways that assure their ownership and satisfaction, and which engenders a feeling of shared responsibility. 5. To develop a sense of community ownership that comes from communication, collaboration and a commitment to people of the local communities, including providers. 6. To apply the principles of cultural competence, recovery, and person centered care to assure equitable access to, engagement with, and benefit from services. 7. To use data that can be translated into knowledge in order to demonstrate accountability, efficiency, need, quality, outcomes, awareness of cultural and ethnic variations and to identify areas for change and improvement. A full version of CenterPoint’s Clinical Design Plan is posted on the CenterPoint website at www.cphs.org. SECTION VIII: ACCESS, ENROLLMENT AND AUTHORIZATION OF SERVICES A. Customer Services Description Customer Services is a critical function of the LME/MCO. CenterPoint is responsible for timely response to consumers and for quick linkages to qualified network providers. Our Customer Services Department operates two dedicated, toll-free telephone lines for offering assistance to consumers and providers. ACCESS Line: 1-888-581-9988 CenterPoint maintains a toll-free “ACCESS” line that is available 24 hours a day, 7 days a week, 365 days a year. This simple system allows for consumers to receive telephonic assessments and crisis intervention. Additionally, we can provide callers with information and referral to MH, I/DD and SA services in the four-county area that includes Forsyth, Stokes, Davie and Rockingham. Provider Line: 1-888-220-5280 The Customer Services Department operates the Provider Line. This line is available 24 hours a day, 7 days a week, 365 days a year. This phone line gives providers an option for immediate assistance or the option to leave a voicemail. If a message is left on the Provider Line voicemail, the call will be returned within 30 minutes. The following are examples of ways in which providers can utilize the UM/Provider Line: • To obtain authorizations for emergency services such as inpatient hospitalization, detoxification services, partial hospitalization, MH/DD respite or mobile crisis registration • To check on a faxed hospital discharge request • To obtain follow-up appointments for consumers being discharged from an emergency department Revised 7/21/15 63 • • Hospital transfers General information about CenterPoint B. Customer Services Process The Customer Services Department responds to calls from both the ACCESS Line and the Provider Line. The Customer Services Department utilizes four (4) different types of personnel: customer services clinician, customer services specialist, customer services representative, and customer services office assistant. The following are their respective qualifications: 1. Customer Services Clinician: • Master's degree with coursework in psychology, social work, human services, or related field, and • At least three (3) years of experience in clinical and service needs assessment, or an equivalent combination of education and experience • Possession of an active, unrestricted LPC, LCSW, LCAS and/or LPA licensure in the State of North Carolina. (Note: It is not CenterPoint’s current practice to hire registered nurses or physicians to perform the clinical triage function.) Duties performed by Customer Services Clinician: • Determine acuity of need, complete assessments, provide crisis intervention and enter initial authorizations for services needed emergently • Provide case consultation to non-licensed staff • Answer clinical communications received directly or through warm transfers from customer services specialists (non-licensed CS Staff) • Provide follow-up for clients who “no-show” to their scheduled appointments • Document grievances or complaints in the IS system and attempt to resolve them • If unable to resolve an issue, route it to the appropriate staff • Log and appropriately route any requests for appeals 2. Customer Services Specialist: • Master's degree with coursework in psychology, social work, human services, or behavioral health and one year of post graduate related experience; or • Bachelor’s degree in psychology, social work, human services or behavioral health and two years of post-graduate related experience; or • Bachelor’s degree in a field other than human services and four years of postgraduate related experience Duties performed by the Customer Services Specialist: • Answer calls received by the Customer Services Department and determine whether caller’s needs are routine or non-routine ̶ emergent or urgent calls that contain specific behavioral signs of psychiatric distress and/or involve substance abuse Revised 7/21/15 64 • • Promptly conduct “warm transfer” for all calls deemed non-routine to Customer Services Clinician Complete routine assessments and enter referral for services as determined by procedure (Referral for Services – Routine) The person in this position does not engage in any activities requiring clinical judgment or interpretation. 3. Customer Services Representative: • • Associate’s degree or High School Diploma/GED with two (2) years of experience in the human services field. Experience in customer services work in the health care field is preferred. Duties performed by Customer Services Representative: • Answer calls received in the Customer Services Department and determine routine (Routine) vs. non-routine (Emergent, Urgent). Non-routine calls are defined as any call that contains specific behavioral signs of psychiatric distress and/or involve substance abuse. • Promptly conduct warm transfer for all calls deemed non-routine to Customer Services Clinician • Complete Routine assessments and enter referral for services as determined by procedure (Referral for Services – Routine) • Provide information regarding community resources • Provide Follow-up for clients who “No-Show” to scheduled appointment • Attempt to resolve any grievances or complaints; document in IS system. Route to appropriate staff if unable to resolve • Log and appropriately route any requests for appeals 4. Customer Services Office Assistant: • High school education, or General Educational Degree (GED) and three (3) years of experience in office assistance work Duties performed by Customer Services Office Assistant: • Provide administrative support to Customer Services Clinicians and Customer Services Specialists • Faxing copies of completed consumer screenings to providers • Tracking consumer appointment compliance • Preparing materials for staff meetings • Responding to non-clinical inquiries from providers The Customer Services Office Assistant does not answer the Access Line, and does not perform any clinical activities. The person in this position does not engage in any activities requiring clinical judgment or interpretation. His/her only interaction with consumers is to schedule appointments, when available, for Revised 7/21/15 65 those consumers who were placed on a waiting list. If any clinical issues are raised by the consumer during the course of appointment setting, a licensed clinician will be immediately available to speak with the consumer. If necessary, the clinician conducts a clinical triage in an effort to assure consumer safety. Your responsibilities as a CenterPoint contracted provider: • Train staff to call the UM/Provider Line (1-888-220-5280) for assistance • Instruct staff NOT to call the Access Line about provider issues • Be clear when requesting information and services C. Access to Services Routine Services: The access standard for routine services is to arrange for services within ten (10) working days (14 calendar days) of contact with the Customer Services Access Line. The geographic access standard for services is thirty (30) miles or thirty (30) minutes driving time in urban areas. Currently all of CenterPoint’s catchment area is designated as urban. Screening and triage is designed as a brief inquiry, not an in-depth assessment, to determine need and to facilitate access to a clinical service by a provider. Screening and triage is intended to identify the nature of a presenting MH/DD/SA issue, recommend a Triage Severity of Need Determination and facilitate referral to a provider of choice or other resource. All calls answered in the Customer Services Department will be answered by a Customer Services Clinician, Customer Services Specialist, or a Customer Services Representative. All calls will be initially screened and triaged into three (3) different “Triage Severity of Need Determination” categories: Emergent, urgent or routine. The category of “Triage Severity of Need Determination” will dictate how the call is routed. Customer Services Staff are trained to prioritize “ruling out” emergent situations when the call is initiated. A call will be screened and triaged as “Triage Severity of Need – Routine” when the call has been “ruled out” as an emergent or urgent severity of need call and the caller presents with mild risk or incapacitation in one or more area(s) of safety, or physical, cognitive, or behavioral functioning related to MH/DD/SA problems. Customer Services Staff are able to override a triage disposition after consultation and approval by the Customer Services Director, Manager, Chief Operations Officer or the Medical Director. This consultation and approval must be documented in the call documentation. All calls answered by a Specialist or Representative will be asked the following questions: • For every consumer call that a Specialist or Representative answers, the following questions are asked: o “Are you currently considering hurting yourself or others? What about over the past month?” o “Are you having feelings of hopelessness or wanting to isolate yourself?” Revised 7/21/15 66 o “Do you hear voices or see things that no one else can hear or see?” If caller responds with “Yes” to any of the above questions the call will be “warm” transferred to a Customer Services Clinician. If caller responds “No” to above questions, the Specialist or Representative may continue the process of scheduling the caller for an assessment with a provider. • When caller is requesting Substance Abuse services or endorses substance use then Specialist and Representatives will ask the following questions: o “Are you having any withdrawal symptoms? Such as abdominal pain, nausea, flu-like symptoms, or tremors.” o “Do you have any current or significant medical conditions? Such as severe pain, bleeding, GI issues, or pregnancy.” o “Have you used any alcohol or drugs today?” If caller responds with “Yes” to any of the above questions the call will be “warm” transferred to a Customer Services Clinician. If caller responds “No” to above questions, the Specialist or Representative may continue the process of scheduling the caller for an assessment with a provider. • If Answered or “Warm” Transferred to a Customer Services Clinician: The Customer Services Clinician will finish collecting the demographic information on the client and search for the client in AlphaMCS. 1. Once the call is triaged as ROUTINE the Customer Services Staff will: Complete the State mandated Screening, Triage, and Referral elements and document the information obtained in AlphaMCS; Retrieve and review the client’s historical information, as needed; Using the information provided determine the type of services indicated. 2. If the caller does not identify a provider of choice, the Customer Services staff will offer the client a choice of three Providers (when available). 3. The Customer Services staff consults the provider’s scheduling calendar for immediate scheduling while the client is still on the line. If an appointment is not available within access guidelines this will be documented and the client may choose another provider. The provider agency may view on the provider portal the pertinent referral information gathered in the screening as well as a description of the needed services. 4. If a call is answered by a Customer Services Specialist or Representative, and if during the course of the call they have any question of the client requiring emergent care rather than a routine referral, the call will be “warm transferred” to a Customer Services Clinician to implement the appropriate intervention and/or referral. Revised 7/21/15 67 5. Training of staff occurs at the time of hire. All Customer Services staff are responsible for staying constantly alert to the potential of an emergent or urgent need and the required intervention. Urgent Services: Receiving Calls: Currently all of CenterPoint’s catchment area is designated as urban. Screening and Triage is designed as a brief inquiry, not an in-depth assessment, to determine need and to facilitate access to a clinical service by a provider. It is intended to identify the nature of a presenting MH/DD/SA issue, recommend a “Triage Severity of Need Determination,” and facilitate referral to a provider of choice or other resource. All calls answered in the Customer Services Department will be answered by a Customer Services Clinician, Customer Services Specialist, or a Customer Services Representative. All calls will be initially Screened and Triaged into three (3) different “Triage Severity of Need Determination” categories: Emergent, Urgent, and Routine. The category of “Triage Severity of Need Determination” will dictate how the call is routed. • A call will be Screened and Triaged as “Triage Severity of Need – URGENT” including but not limited to the following: A. A client reporting a substance related problem, but denying any imminent risk of harm to themselves or others. B. The client seems to be at risk for continued deterioration in functioning if not seen within 48 hours. C. The client requires reassurance that help is available. Protocol for Calls Screened and “Triaged as Severity of Need – URGENT” due to criteria “A” above: • If Call Answered by Customer Services Specialist or Representative: When caller is requesting Substance Abuse services or endorses substance use then Specialist and Representatives will ask the following questions: o “Are you having any withdrawal symptoms? Such as abdominal pain, nausea, flu-like symptoms, or tremors.” o “Do you have any current or important medical conditions? Such as severe pain, bleeding, GI issues, or pregnancy.” o “Have you used any alcohol or drugs today?” If caller responds with “Yes” to any of the above questions, the call will be “warm” transferred to a Customer Services Clinician. If caller responds “No” to above questions then Specialist and Representative may continue to schedule caller for an assessment with a provider. Revised 7/21/15 68 • If Answered or “Warm” Transferred to a Customer Services Clinician: The Customer Services Clinician will finish collecting the demographic information on the client and search for the client in AlphaMCS. Protocol for Calls Screened and “Triaged as Severity of Need – URGENT” due to criteria B and C above: • If Call Answered by Customer Services Specialist or Representative: For every client call that a Specialist or Representative takes the following questions are asked: o “Are you currently considering hurting yourself or others? What about over the past month?” o “Are you having feelings of hopelessness or wanting to isolate yourself?” o “Do you hear voices or see things that no one else can hear or see?” If caller responds with “Yes” to any of the above questions, the call will be “warm” transferred to a Customer Services Clinician. If caller responds “No” to above questions then Specialist and Representative may continue to schedule caller for an assessment with a provider. • If Answered or “Warm” Transferred to a Customer Services Clinician: The Customer Services Clinician will collect demographic information on the caller and the client and search for the client in AlphaMCS. If clinical intervention is not warranted, then Customer Services Staff will continue with the call: 6. If the client is not located in the eligibility file, the Customer Services Staff will advise the client of this, and proceed with collection of enrollment data. 7. The Customer Services Staff will evaluate the client’s needs as follows: Complete the State-mandated Screening, Triage, and Referral elements and document the information in AlphaMCS; Retrieve and review the client’s historical information, as needed; Using the information provided, determine the type of services indicated. 8. If the caller does not identify a provider of choice, the Customer Services Staff will offer the client a choice of three Providers (when available). 9. The Customer Services Staff will view the chosen provider’s scheduling calendar for immediate scheduling while the client is still on the line. If an appointment is not available within 48 hours, this will be documented and the client may choose another provider. If no appointments are available within the mandated timeframe the client will be treated as “EMERGENT” and referred to “walk-in” to an Advanced Access Provider or hospital emergency department. In the event the client prefers an appointment time outside of the 48 hour timeframe, the Customer Services Staff schedules the appointment and documents the client’s preference in the screening record. 10. The information obtained in the screening is communicated electronically to the provider agency as well as information indicating the service to be provided. The appointment is also entered into the provider’s scheduling calendar. 11. The Customer Services Staff will remind the client that the Customer Services Department is available twenty-four (24) hours a day and instruct them to again contact Revised 7/21/15 69 12. 13. the Customer Services line at any time the situation escalates and requires immediate attention. Customer Services Staff will monitor appointment compliance data and continue to follow-up with any Urgent contacts who no show for their scheduled appointment and make attempts to reschedule the appointment and/or reclassify their level of urgency (higher or lower) if appropriate. Training of staff occurs at the time of hire. All Customer Services staff are responsible for staying constantly alert to the potential of this type of call or need for intervention. Emergent Services: Receiving Calls: The access standard for non-life threatening emergency services is within two (2) hours or immediately for life-threatening emergencies. The geographic access standard for services is thirty (30) miles or thirty (30) minutes driving time in urban and rural areas Screening and Triage is designed as a brief inquiry, not an in-depth assessment, to determine need and to facilitate access to a clinical service by a provider. It is intended to identify the nature of a presenting MH/DD/SA issue, and to recommend a triage severity of need determination and facilitate referral to a provider of choice or other resource. All calls answered in the Customer Services Department will be answered by a Customer Services Clinician, Customer Services Specialist or a Customer Services Representative. Customer Services Staff are trained to prioritize “ruling out” Emergent situations when the call is initiated. A call will be screened and triaged as “Triage Severity of Need – Emergent” when the caller demonstrates one or more of the following, including but not limited to: • Real and present danger to self or others as indicated by behavior, means, plan, or intent • Voice tremulous or raised • Rapid speech or slow speech • Crying • Making threats or indicating intent to harm self or others • Confusion • Any other statements or presentation indicative of caller being unstable and demonstrating significant impairment in judgment, impulse control, and/or functioning due to psychotic symptoms, chemical intoxication, or both • Immediate and severe medical complications concurrent with or as a consequence of psychiatric or substance related illness and/or its treatment • The caller indicates, either by request or through clinical assessment, a need to be seen immediately Protocol for Calls Screened and “Triaged as Severity of Need – EMERGENT”: • If Call Answered by Customer Services Specialist or Representative: If call is answered by a Customer Services Specialist or Representative and triaged as “Severity of Need EMERGENT” the caller will be “warm” transferred to a Customer Services Clinician. Revised 7/21/15 70 • If Answered or “Warm” Transferred to a Customer Services Clinician: The Customer Services Clinician will determine through clinical assessment whether the client represents an immediate danger to his/her self or others. If the client is in immediate danger, the Customer Services Clinician will implement crisis intervention procedures in an attempt to stabilize the client. • If the situation is stabilized, then: A. The Customer Services Clinician will attempt to collect the remaining STR data elements and identify treatment needs. B. If the client has viable and safe transportation to a local provider, the Customer Services Clinician will direct the client to the Advanced Access Provider nearest them or local Emergency Department and document the referral in AlphaMCS. C. The Customer Services Clinician will contact the provider and give a brief overview of the client’s need and give them the referral number so the provider can access the screening information in AlphaMCS. D. If there is no viable transportation, the Customer Services Clinician will contact the client’s First Responder (if the client is receiving an enhanced benefit service already) or Mobile Crisis Management (MCM) clinician (regardless of enrollment status) to respond to the client in their current location. The Customer Services Clinician will continue to follow up with the client until the Mobile Crisis Clinician has arrived. • If the Client is unable to be stabilized, then: A. The Customer Services Clinician will determine if there is a family member or other reliable support system with or nearby the client. If there is someone present the Clinician will: 1. Speak directly with the person and obtain their name. 2. Determine if the person is responsible and can safely transport the client to the closest Advanced Access Provider or emergency room. 3. Assure the support person has the appropriate phone number and/or address to which the client will be transported. 4. Inform the person that the Customer Services Clinician will contact the facility to inform them of the client’s pending arrival. 5. Ask the client or responsible person to take any insurance information with them, if possible. 6. If it is determined that the person is not able to provide safe transportations move to B. B. When there is no responsible person present, the Customer Services Clinician will: 1. Remain on the telephone with the client while a co-worker calls “911”. It is extremely important to keep the client on the line while requesting assistance from other Customer Services staff. The Customer Services Clinician will give the co-worker the following information on the client: a. Name of the client Revised 7/21/15 71 b. 2. 3. 4. 5. Phone number and address where the client is currently located (do not assume the client is at his or her residence.) c. The current situation d. Type of response needed (i.e. EMS or Law Enforcement) Once the emergency personnel arrive speak with them to confirm their name and the location to which the client will be transported. Once the safety of the client has been established, the Customer Services Clinician will contact the agency/facility of the client’s pending arrival and a brief description of the situation The Customer Services Clinician requests the name of the person taking the information and requests a return call to confirm the client has arrived. The Customer Services Clinician carefully documents all the specifics of the contact including: a. Times b. Clinical information, attempts to stabilize the client, and names of any individual involved with the call (client, responsible persons, emergency personnel, agency staff, etc.) c. That “911” and the agency/facility was contacted d. Any outcomes or dispositions C. The Customer Services Clinician will continue to follow-up with any emergent contacts until it is ascertained that the client has been able to receive the care that is most appropriate to meet the client’s clinical needs. D. If a shift change occurs during the client’s initial call, the Customer Services Clinician who is on the phone with the client will continue working with the client or responsible person until they arrive at the hospital or appropriate agency. Once this has occurred the Clinician will give a detailed report of the situation to the on-coming Customer Services Clinician who will complete the follow-up. If there is an “adverse event”, the original clinician will also contact the Customer Services Director or representative prior to completing his or her shift. E. Training of staff occurs at the time of hire. All Customer Services Department staff are responsible for staying constantly alert to the potential of this type of call or need for intervention. NOTE: It is the responsibility of the Customer Services staff to inform clients of the availability and type of Emergency Services nearest them as they are assisting the client in an emergency. D. Process for Telephonic Pre-Service Authorization by Calling Provider Line: (1-888-220-5280) 1. Customer Services Staff will conduct telephonic reviews for pre-service authorization of the following services due to the acute nature of the need: Revised 7/21/15 72 Acute Psychiatric Inpatient All Detoxification Services Facility-based Crisis Services Emergency Respite Services Mobile Crisis Management Services The CenterPoint Customer Services Staff will conduct telephonic reviews for Pre-Service Authorization of “acute services” or services for which access is urgent or emergent. Except for instances of life threatening emergency situations, a Pre-Service Authorization review is conducted between the provider or facility staff and a CenterPoint Customer Services Staff to determine the appropriateness of care. The clinical information provided in the review must have been obtained from a face-to-face assessment of the eligible client conducted within twenty-four (24) hours Pre-Service to the call. a. When the provider calls CenterPoint with a Pre-Service Authorization request, the call is answered by Customer Services Staff. Customer Services Staff will confirm eligibility and enrollment of the client. If the client is not enrolled, the Customer Services Staff will assist the provider in enrolling the client. (See - Eligibility and Enrollment above). If there is a question about the client’s eligibility, even if eligibility is not confirmed at the time of the call, the Pre-Service-authorization review will be conducted and a decision made, with a disclaimer given that eligibility must be confirmed in order for payment to occur. b. If the client’s situation meets CenterPoint’s established clinical criteria for the requested service, the Customer Services Staff will complete the following steps: Authorize the service based on the Authorization Guidelines. The Customer Services Staff will verbally notify the caller of the authorization, and generate an authorization number, by completing a standardized authorization request. This number generated from this request will serve as the authorization number. c. If the client’s condition does not meet the criteria for the requested service, the Customer Services Clinician will promote the request for peer clinical review after determining eligibility for funding. 2. Concurrent authorization requests for acute services: Concurrent authorization requests are received and reviewed during regular business hours. a. For concurrent reviews of urgent services, the facility’s Utilization Department contacts CenterPoint’ UM staff to complete a telephonic review b. Eligibility is confirmed c. The request is reviewed by Clinical staff with a decision provided to the Facility within twenty-four (24) hours of the original request 3. Discharge: Discharge planning begins at the time of the initial assessment and is an integral part of every client’s treatment plan regardless of the level of care being delivered. The discharge planning process includes use of the client’s strengths and support systems, the provision of treatment in the least restrictive environment possible, the planned use of treatment at varying levels of intensity, and the selected use of community services and support when appropriate to assist the Revised 7/21/15 73 client with functioning in the community. Care Coordinators - Hospital Liaisons and the UM department assist with the discharge planning for clients in acute levels of care. Among the functions: Identify clients who have multiple admissions to acute care facilities and make recommendations, when appropriate, that enhanced services start prior to client discharge Make follow-up appointments with appropriate community providers with-in forty-eight (48) hours of discharge, when available 4. Follow up after Discharge: Clinical Operations staff recognizes the importance of follow up care after a client is discharged from an acute level of care. Every effort is made to assure the client is engaged in treatment. All discharge appointments are followed up on to make sure the client was seen. This is done by contacting the provider to verify that the appointment was kept. This along with the next appointment date is monitored in the IS system. If an appointment is not kept, Care Coordination staff: a. Document the reason (i.e. No Show, client canceled, provider canceled, etc.) and whether or not the appointment was rescheduled b. Contact the client to discuss barriers and attempt to schedule another appointment c. If the client is still not able to engage in treatment the Care Coordination Staff will contact the client face to face to attempt to engage them in services E. State Funded, MH/SA Registry of Unmet Needs (Note: Not applicable to Medicaid Clients and Medicaid-funded services) The purpose of the Registry of Unmet Needs is to assure a standardized practice of initiating, monitoring and managing a registry of services that reach capacity as a result of limitations of non-Medicaid funding sources. 1. Process: a. A Registry of Unmet Needs for services may be necessary when the demand for services exceeds available state resources or when service capacity is reached as evidenced by no available provider for the service needed (e.g. all residential beds are full). This applies to Non-Medicaid Funds Only. b. Standardized monitoring reports will be available from CenterPoint’s Finance Department indicating level of funding available for services. c. Reports are routinely monitored by the CFO, the Finance Cross-Functional Team(s) and by the Utilization Management Director. d. Should funding levels reach a point where projections indicate all funds are encumbered, the CFO will notify the Utilization Management Director and Network Management Director. e. Network Development will maintain a State funded, MH/SA Registry of Unmet Needs for all services meeting the service capacity or funding limitation criteria listed above. Network Management CFT will review the list and make recommendations for meeting the needs to Finance CFT and Care Coordination CFT. . (Please note: the I/DD Registry is managed by Care Coordination and monitored separately) Revised 7/21/15 74 For the additional information or a copy of the most recent CenterPoint procedure on the Registry of Unmet Needs, please call 1-888-581-9988. If a Medicaid funded service is needed by a Medicaid recipient, and there is no capacity within the network to provide this service or an alternative agreeable to the client, the service will be sought from an out of network provider. F. Enrollment Refer to Section XI (“Getting Paid”). G. Initial Assessment Providers should complete an initial assessment addressing the elements required in the current Service Records Manual (APSM 45-2). 1. Service Authorization Request (SAR) Forms: CenterPoint has a standardized authorization request form that captures demographic and clinical information. When this form is completed thoroughly, Utilization Management will be able to make the clinical determination required for the clients’ needs. If the form is not completed fully, including all clinical information required, a delay in the approval of a service request or a denial of the authorization request may occur. Utilization Management will attempt to garner the information through contact with the provider, but this can take several days to resolve in some cases. Providers will be monitored for request form completeness and will be identified for additional training as needed. H. Initial Authorization The purpose of this process is to identify the steps required in performing prior-authorization of services. Prior-authorization of services is the responsibility of CenterPoint’s Utilization Management Department. Requesting the Authorization is the responsibility of the provider. Process: 1. Prior-authorization is required for all CenterPoint covered services, with the following exceptions: a. Unmanaged outpatient basic benefits for individual, family and group therapy; twelve (12) psychiatric E & M visits for children and eight (8) psychiatric E & M visits for adults. Please see the UM Medicaid and state funded benefits design packages for specifics related to psychological testing. Initial eight (8) adult and the initial sixteen (16) children outpatient services per year that are covered under the Basic Benefit Package b. Emergency/Crisis services for Behavioral Healthcare c. Codes specifically agreed upon by CenterPoint and provider to be listed as “No Auth Required” in the published UM Medicaid and state funded benefits design packages. Please see the UM design packages for applicability. Revised 7/21/15 75 2. Pre-Service reviews processes based on classification of request Pre-service reviews are processed depending on whether the request is classified as urgent or nonurgent.. Expedited requests may be requested by the client/guardian or the provider where the time taken for standard resolution could seriously jeopardize the client’s life, health or ability to attain, maintain or regain maximum function. If the request meets the expedited criteria, a decision will be made within 72 hours. If expedited criteria are not met, standard timeframes apply. Urgent requests (i.e., those related to inpatient behavioral health services where the provider does not use the pass through request, partial hospitalization, detoxification and emergency respite may be processed by phone 24 hours a day, 7 days a week. In most cases, a determination will be made by the end of the phone call, but a determination is always made (and the client or provider advised) within 24 hours of the request. For urgent requests involving Medicaid Clients, the time period for certification decisions may be extended by 14 days (upon request of the client or provider or upon determination by LME/MCO that an extension is justified). The LME/MCO will notify the client prior to the expiration of the initial 14 calendar day period of the circumstances requiring the extension and the date when the decision is expected to be made. Please note that Requests for State funding will not be extended (per the NC Division of Mental Health/Developmental Disabilities/Substance Abuse Services). For non-urgent requests, determination is issued no later than 14 day calendars from receipt of the request. For Medicaid clients, this time period will be extended by an additional 14 days (upon the client’s or provider’s request or upon determination by the LME/MCO that an extension is justified). The LME/MCO will notify the client prior to the expiration of the initial 14 calendar day period of the circumstances requiring the extension and the date when the decision is expected to be made. If information necessary to make a determination is not submitted, the notice of extension must specifically describe the required information. Please note that Requests for State funding cannot be extended (per the NC Division of Mental Health/Developmental Disabilities/Substance Abuse Services). 3. To remain consistent with Division of Medical Assistance (DMA) guidelines the CenterPoint Utilization Management Department (UM) is only able to make formal decisions (approval, denial, or extensions when appropriate) when a complete request is received: For a request to be considered “complete” it must contain the following elements: Recipient Name Medicaid ID Date of Birth Provider contact information Date of request Revised 7/21/15 76 Service(s) requested Service Order Completed Check boxes (Signature Page / Service Order Yes or No Check Boxes related to medical necessity, direct contact with the individual, and review of the individual’s Clinical Assessment) Person-Centered Plan/Individual Service Plan, if applicable. If an authorization request is received that requires a corresponding PCP and none is submitted the request will be returned as unable to process. 4. Initial Authorization of Basic Augmented and Enhanced Services: a. Prior-authorization for all Basic Augmented Services may be requested through electronic submission through AlphaMCS of the standardized authorization request form (an expedited prior-authorization can be requested telephonically for any service if immediate access is clinically indicated.) b. For Telephonic Prior-Authorization, Customer Service Clinicians may conduct telephonic reviews for prior-authorization of following services due to the acute nature of the need: o Acute Psychiatric Inpatient o All Detoxification Services o Facility-based Crisis Services o Emergency Respite Services o Mobile Crisis Management Services CenterPoint will conduct telephonic reviews for prior-authorization of “acute services” or services for which access is urgent. Except for instances of life threatening emergency situations, a prior-authorization review is conducted between the provider or facility utilization review staff and a CenterPoint staff to determine the appropriateness of care and to certify the initial treatment plan. The clinical information provided in the review must have been obtained from a face-toface assessment of the eligible client conducted within twenty-four (24) hours prior to the call. When the provider calls CenterPoint with a prior-authorization request, staff will confirm eligibility and enrollment of the client. If the client is not enrolled, the clinician will assist the provider in enrolling the client. If there is a question about the client’s eligibility, even if eligibility is not confirmed at the time of the call, the prior authorization review will be conducted and a decision made, with a disclaimer given that eligibility must be confirmed in order for payment to occur. When a request for prior-authorization for the above services is received, the Clinician will access any existing clinical case information in CenterPoint’s database. If the client’s situation meets CenterPoint’s established clinical criteria for the requested service, the Clinicians will complete the authorization. Note: If a provider continues to request authorization for services which do not appear to meet CenterPoint’s applicable clinical criteria and guidelines, the Clinician will advise the provider that a peer review will be necessary. The Customer Services Clinician or Utilization Management Clinician will refer the case to peer clinical review. If after the peer clinical review it cannot be Revised 7/21/15 77 determined that the request for service meets established clinical criteria the provider will be contacted to schedule a peer to peer conversation. This is a review with the Chief Clinical Officer, staff psychologist or a Contractor with expertise in the area requested. 5. Initial Authorization of Enhanced Services: Enhanced services will be authorized through review of the authorization request form and approved Person-Centered Plan as submitted by the Clinical Home Provider or assigned Care Coordinator if applicable. Services will be identified through the Person-Centered Planning process in a coordinated effort between the Clinical Home Provider, the client, client’s family/guardian and other providers as appropriate. I. Continued Authorization of Services Continued Authorization of Basic Augmented Services: If the PCP has changed or has been updated, the PCP and authorization request form must be completed before an authorization of services can occur. If the PCP has not been updated, the continuing authorization of services will be the responsibility of the provider. At the time of need for a continued authorization, the provider shall complete an authorization request form and submit it electronically to Utilization Management at CenterPoint. The information required establishing the need for continued medical necessity and service continuation criteria must be included. The next review date is indicated by the end date on the authorization notification. It is the provider or facility's responsibility to submit a request for further service authorization to CenterPoint’s UM prior to and no sooner than twenty-one (21) days before the expiration of the current authorization. Based on a review of the information provided, the Utilization Management staff will make an authorization decision according to the following: a. If the client's condition continues to meet CenterPoint’s clinical criteria for the current level of care, the UM staff will certify the care within the guidelines applicable to the requested level of care and generate an authorization notification. b. If the client's condition appears to no longer meets the criteria for the current level of care, the UM staff will refer the case for peer clinical review and advise the provider. c. If, after review, the request for authorization for services does not appear to meet applicable CenterPoint clinical criteria, the UM staff should advise the provider that a peer to peer conversation review is available. All determinations and related actions will be recorded in CenterPoint’s Management Information System. Continued Authorization of an Enhanced Service: The Person-Centered Plan and authorization request form must be completed before an authorization of services can occur. The continuing request for authorization of services is the responsibility of the provider. Revised 7/21/15 78 At the time of need for a continued authorization, the provider shall complete an authorization request form and submit it electronically to Utilization Management at CenterPoint. The information required establishing the need for continued medical necessity and service continuation criteria must be included. The next review date is indicated by the end date on the authorization notification. It is the provider or facility's responsibility to submit a request for further service authorization to CenterPoint’s UM prior to, but no sooner than twenty-one (21) days before the expiration of the current authorization, and to conduct a concurrent clinical review. Based on a review of the information provided, the Utilization Management staff will make an authorization decision according to the following: a. If the client's condition continues to meet CenterPoint’s clinical criteria for the current level of care, the UM staff will certify the care within the guidelines applicable to the requested level of care and generate an authorization letter. b. If the client's condition no longer meets the criteria for the current level of care, the UM staff will refer the case for peer clinical review and advise the provider. c. If, after review, the request for authorization for services does not appear to meet applicable CenterPoint clinical criteria, the UM staff should advise the provider that a peer to peer conversation is review is available. All determinations and related actions will be recorded in CenterPoint’s IS System. As with Prospective/Pre-Service Reviews, Continued Authorization/Concurrent Reviews are processed differently depending on the service being reviewed. In the event a physician who has knowledge of a case states that a non-urgent case is, indeed, urgent, then UM staff processes the case as urgent. Again, an expedited request may be requested by the client/guardian or provider/representative if it is indicated that taking the time for a standard resolution could seriously jeopardize the client’s life, health or ability to attain, maintain or regain maximum function. If the request meets the expedited criteria, a decision will be made within 72 hours. If expedited criteria are not met, standard timeframes apply. For urgent requests involving continued stay reviews for inpatient behavioral health services, partial hospitalization, and ASAM Level 3.7 D detoxification, requests are submitted via the AlphaMCS as described in non-urgent pre-service reviews. The UM staff will notify the client or provider of confirmation of certification within 24 hours from receipt of request for State and Medicaid clients (assuming request was received at least 24 hours before the expiration of the currently certified period of treatment). For Medicaid clients only, if the request is received less than 24 hours before the expiration of the currently certified period of treatment, a determination is made and notification provided within 72 hours. For requests involving Medicaid Clients, this time period will be extended one time for an additional 14 days if the client requests the extension or the provider requests one on behalf of the client. The LME/MCO may issue an extension without request if it is in the best interest of the Client. The LMEO/MCO will notify the client prior to the expiration of the initial 14 calendar day period of the circumstances requiring the extension and the date when the decision is expected to be made. Please note that Requests for State funding will not be extended (per the NC Division of Mental Health/Developmental Disabilities/Substance Abuse Services). Revised 7/21/15 79 For non-urgent requests, determination is issued no later than 14 day calendars from receipt of the request. For Medicaid clients, this time period will be extended by an additional 14 days (upon the client’s or provider’s request or upon determination by the LME/MCO that an extension is justified). The LME/MCO will notify the client prior to the expiration of the initial 14 calendar day period of the circumstances requiring the extension and the date when the decision is expected to be made. If information necessary to make a determination is not submitted, the notice of extension must specifically describe the required information. Please note that Requests for State funding cannot be extended (per the NC Division of Mental Health/Developmental Disabilities/Substance Abuse Services). J. Discharge Review Discharge planning begins at the time of the initial assessment and is an integral part of every client’s treatment plan regardless of the level of care being delivered. The discharge planning process includes use of the client’s strengths and support systems, the provision of treatment in the least restrictive environment possible, the planned use of treatment at varying levels of intensity, and the selected use of community services and support when appropriate to assist the client with functioning in the community. Involvement of family members and other identified supports, including members of the medical community, require the client’s written consent. The purpose of this process is to identify the steps to be taken by the Utilization Management staff in assisting with Discharge Planning Efforts. Process: 1. The Utilization Management staff reviews the status of the discharge plan at each review to assure that: A discharge plan exists The plan is realistic, comprehensive, timely and concrete Transition from one level of care to another is coordinated The discharge plan incorporates actions to assure continuity of existing therapeutic relationships The client understands the status of the discharge plan 2. When the discharge plan is lacking in any respect, the Utilization Management staff addresses the relevant issues with the provider. 3. The Utilization Management staff assists with the development of discharge plans for clients in all levels of care. Among the functions: Identify clients who are remaining hospitalized, or at any other level of care, who do not meet criteria for that level of care and help develop a plan to get the right service at the right level Monitor clients to assure that they receive clinically indicated services Whenever a client is discharged from detoxification, inpatient psychiatric or partial hospitalization care, the discharge plan should include a follow-up appointment within five working days. Utilization Management staff will work with the discharging facility to assure that an appointment is made and monitor whether the client kept the appointment. Revised 7/21/15 80 The Utilization Management staff will coordinate with the person’s Clinical Home to assure there are appropriate services in place following discharge. If the person does not have a Clinical Home, and the person meets High Cost, High Risk or Special Health Care Needs Population criteria, the UM staff will refer to the Care Coordination Department for follow-up K. Utilization Review The primary function is to monitor the utilization of services and review utilization data to evaluate and assure that services are being provided appropriately within established benchmarks and clinical guidelines; that services are consistent with the authorization and approved PCP/Treatment Plan; and that established penetration goals are maintained. Utilization Review is an audit process that involves a review of a sample of services that have been provided. Information from the client’s record (assessment information, treatment plan and progress notes) is evaluated against Medical Necessity Criteria. This is done concurrently (during re-authorization) and retrospectively (after the service has been provided). The outcome of this review can indicate areas where provider training is needed, services that were provided that did not meet Medical Necessity, and situations where the client did not receive appropriate services or care that was needed. Indicators will be identified to select cases for review, such as high utilization of service, frequent hospital admissions, etc. as well as random sampling of other events. CenterPoint utilizes both Focused Utilization Review and a sampling process across Network providers in its Utilization Review methodologies. Focused Review: A Focused Review will be based on the results of Monitoring Reports that identify outliers as compared to expected/established service levels or through specific cases identified in the CenterPoint clinical staffing process to be outside the norm. Focused samples may include: High-risk clients – Examples may include, but are not limited to, clients who have been hospitalized more than one time in a thirty (30)-day period; developmentally disabled clients as identified in the Risk/Support Needs Assessment; children and youth with multiple-agency involvement; or active substance use by a pregnant female Under-utilization of services – Examples may include, but are not limited to, clients who utilize less than 70% of an authorized service or clients who have multiple failed appointments Over-utilization of services – Example: clients who continue to access crisis services with no engagement in other services Services infrequently utilized – Example: an available practice that is not being used High-Cost Treatment – Clients in the top 20% of claims for a particular service Routine Utilization Review: A Routine Utilization Review will focus on the efficacy of the clinical processes in cases as they relate to reaching the goals in the client’s PCP/treatment plan. CenterPoint will also review the appropriateness and accuracy of the service provision in relation to the authorizations. All providers contracted with CenterPoint who are currently serving CenterPoint clients are subject to Utilization Reviews to assure that clinical standards of care and medical necessity are being met. A routine UR will be inclusive of, but not limited to: evaluations of services across the delivery spectrum; evaluations of clients by diagnostic Revised 7/21/15 81 category or complexity level; evaluations of providers by capacity, service delivery and best-practice guidelines and evaluations of utilization trends. SECTION IX: STATE SERVICE DEFINITIONS 1. NC MH/DD/SAS Health Plan – 1915 (b) Waiver: The NC MH/DD/SAS Health Plan services follow the NC State Medicaid Plan Service Array for Behavioral Healthcare. 2. NC Innovations Plan – 1915 (c) Waiver (c): The NC Innovations Waiver is a 1915(c) Home and Community-Based Waiver. The services defined under this Waiver replace the Community Alternatives Program (CAP) services under the NC CAP-I/DD Waiver Plan 3. B-3 Services: These are Medicaid services that are funded through a separate capitation payment. Mental Health, Developmental Disabilities and Substance Abuse Services (MH/DD/SAS) Service Definitions Manual may be accessed online at: http://www.ncdhhs.gov/mhddsas/providers/servicedefs/ Clinical Coverage Policies 8A-8P may be accessed at: http://www.ncdhhs.gov/dma/mp/index.htm Revised 7/21/15 82 SECTION X: RESOURCES FOR PROVIDERS Contracted providers must keep abreast of rule changes at the State level, attend workshops and trainings to maintain clinical skills and/or licensure, be knowledgeable on evidenced based or emerging practices and be current on coding and reimbursement. CenterPoint will provide a number of resources to assist providers in meeting this requirement. We will communicate information regarding workshops through a variety of mediums and will offer trainings or technical assistance as needed. Network Development will coordinate a training calendar that lists all trainings planned, on an annual basis, and will provide this to providers. The following resources are provided as assistance and linkage and are not designed to be a comprehensive list for providers. 1. Training and Technical Assistance: CenterPoint at NetworkDevelopment@cphs.org 2. Advocacy: National Alliance on Mental Illness (NAMI) www.nami.org 3. Associations: American Academy of Child and Adolescent Psychiatry www.aacap.org American Academy of Psychoanalysis and Dynamic Psychiatry www.aapsa.org Association of Ambulatory Behavioral Healthcare www.aabh.org American Association for Geriatric Psychiatry www.aagponline.org American Association of Marriage and Family Therapy www.aamft.org American Association of Pastoral Counselors www.aapc.org American Psychiatric Association www.psych.org American Psychological Association www.apa.org American Psychological Society www.psychologicalscience.org Autism Society of America www.autism-society.org National Association of Protection and Advocacy Systems (NAPAS) www.protectionandadvocacy.com National Association of Psychiatric Health Systems www.naphs.org National Association of Social Workers Revised 7/21/15 83 www.socialworkers.org National Association of State Mental Health Program Directors (NASMHDPD) www.nasmhpd.org National Council for Community Behavioral Healthcare www.nccbh National Mental Health Association (NMHA) www.nmha.org North Carolina Council of Community Programs www.nc-council.org North Carolina Substance Abuse Professional Certification Board www.ncsappb.org United States Psychiatric Rehabilitation Association www.uspra.org 4. Behavioral Healthcare Resources: Behavioral Healthcare Institute http://www.behavioralhealthcareinstitute.com/ Boston University Center for Psychiatric Rehabilitation www.bu.edu/sarpsych CARF www.carf.org International Center for Clubhouse Development www.iccd.org Latino Behavioral Healthcare Institute www.lbhi.org Manisses Communication www.manisses.com National Center for Child Traumatic Stress (NCCTS) www.NCTSNet.org National Committee for Quality Assurance (NCQA) www.ncqa.org North Carolina Foundation for Alcohol and Drug Studies www.ncfads.org Research and Training Center for Children’s Mental Health http://rtckids.fmhi.usf.edu Teen Screen www.teenscreen.org 5. Client and Family Resources: Association for Person in Supported Employment (APSE) www.apse.org Children and Adults with Attention-Deficit/Hyperactivity Disorder www.chadd.org CHADD online library Revised 7/21/15 84 www.help4uadhd.org/library.cfm Federation of Families for Children’s Mental Health www.ffcmh.org NMHA-Consumer Supporter Technical Assistance Center www.ncstac.org/ National Empowerment Center www.power2u.org National Mental Health Consumers Self-Help Clearinghouse www.samhsa.gov/recoverytopractice/RTP-Contribution-Detail-ForThe_National_Mental_Health_Consumers__Self_Help_Clearinghouse-239.aspx 6. Cultural Competency: CenterPoint Cultural Competency Page www.cphs.org Annie E. Casey Foundation www.aecf.org Association of Gay and Lesbian Psychiatrists www.aglp.org Association for Lesbian, Gay, Bisexual & Transgender Issues in Counseling www.algbtic.org Diversity Inc., www.diversityinc.com Indian Country (The nation’s leading American Indian news source) www.indiancountry.org Latino Behavioral Health Institute www.lbhi.org Medline Plus has health information in over 40 different languages www.medlineplus.gov National Asian American Pacific Islander Mental Health Association www.naapimha.org National Congress of American Indians www.ncai.org National Latino Behavioral Health Association www.nlbha.org National NAMI (Has NAMI en Espanola, as well as the NAMI Multicultural Center Resources webpage) www.nami.org National Organization of People of Color Against Suicide www.nopcas.org Native Web (resources for indigenous cultures around the world) www.nativeweb.org NC African American Impact Study www.kenan-flagler.unc.edu/kenan-institute/publications/2007-african-american NC Hispanic Impact Study Revised 7/21/15 85 http://www.kenanflagler.unc.edu/KI/economicDevelopment.cfm NCLR – National Council of La RAZA (the largest Latino civil rights and advocacy organization in the U.S.) www.nclr.org Pan American Health Organization www.paho.org The Association of Black Psychologists http://www.abpsi.org/ The Black Mental Health Alliance www.blackmentalhealth.com The Office of Ethnic Minority Affairs of the American Psychological Association has a webpage www.apa.org/pi/oema/homepage.html World Federation for Mental Health (making mental health a global priority) www.wfmh.com World Health Organization (This website can be accessed in Arabic, Chinese, English, French, Russian and Spanish) www.who.int/en 7. Intellectual/Developmental Disabilities: Autism Speaks Family Services www.autismspeaks.org Center for Study on Autism www.autism.org Centers for Medicare and Medicaid www.cms.gov Council for Exceptional Children (CEC) www.cec.sped.org Exceptional Children’s Assistance Center www.ecac-parentscenter.org Family Support Network of North Carolina www.fsnnc.org NC Division of Health and Human Services www.dhhs.state.nc.us Spectrum Resources of NC www.spectrumresourcesofnc.net The Arc of the United States www.thearc.org The Arc of NC www.arcnc.org The Autism Society of NC www.autismsociety-nc.org/ The Beach Center/Family Training www.beachcenter.org The Durham Center Revised 7/21/15 86 www.alliancebhc.org/ The National Inclusion Project www.inclusionproject.org Piedmont Down Syndrome Support Network www.pdssn.org Brain Injury Association of North Carolina www.BIANC.net The American Association of Intellectual and Developmental Disabilities www.AAIDD.org 8. Federal Government: US Department of Health and Human Services – Substance Abuse and Mental Health Services Administration www.samhsa.gov Centers for Medicare and Medicaid www.cms.hhs.gov Medicare www.medicare.gov National Council on Disability www.ncd.gov President’s Committee on Employment of People with Disabilities www.dol.gov/odep/ President’s New Freedom Commission www.mentalhealthcommission.gov Health Care Financing Administration https://www.federalregister.gov/agencies/health-care-finance-administration Knowledge Exchange Network http://www.gken.org/ National Institute on Alcohol Abuse and Alcoholism www.niaa.nih.gov National Institute on Drug Abuse www.nida.nih.gov United State Department of Housing and Urban Development www.hud.gov White House Office of National Drug Control Policy www.whitehousedrugpolicy.org 9. Grants and RFPs: American Psychiatric Foundation www.psychfoundation.org Foundation Center Philanthropy News Digest- RFP Bulletin http://fdncenter.org/pnd/index.jhtml Revised 7/21/15 87 10. North Carolina State Links: Institute of Government www.sog.unc.edu/ North Carolina Department of Health and Human Services www.dhhs.state.nc.us North Carolina Division of Mental Health, Developmental Disabilities and Substance Abuse Services www.dhhs.state.nc.us/mhddsas North Carolina Coalition to End Homelessness www.ncceh.org North Carolina Division of Medical Assistance www.dhhs.state.nc.us/dma/ North Carolina Division of Medical Assistance Publications www.ncdhhs.gov/mhddsas/statspublications/index.htm North Carolina Housing Coalition www.nchousing.org North Carolina Housing Finance Agency www.nchfa.com 11. Other State Links: New York State Office of Mental Health www.omh.state.ny.us Revised 7/21/15 88 SECTION XI: GETTING PAID A. Enrollment and Eligibility Process Eligibility Determination: Clients who have their services paid for in whole or in part by CenterPoint must be enrolled in the CenterPoint system. If you have any questions about a client’s eligibility, please call the Customer Services Center at 1-888-581-9988. It is the responsibility of each provider to make a complete and thorough investigation of a client’s access to third party payers prior to requesting to enroll that person into the CenterPoint system. This would require that the Provider check for the following: Current enrollment or eligibility to enroll in Medicaid Current Medicare or other third party insurance coverage Involvement of a third party payer such as worker’s compensation, EAP, program, court ordered services paid for by the court, etc. Possible eligibility for local or state services funds as determined by whether the client meets the criteria: o Lack of Medicaid or other third party insurance Previous enrollment in the CenterPoint system. If the client has Medicaid or has already been enrolled in the CenterPoint system, they are financially eligible for Medicaid reimbursable services from CenterPoint. If they are not yet enrolled, then the provider must provide the data necessary to enroll them. Providers should assist clients that may be eligible for Medicaid funding in applying for Medicaid through the county Department of Social Services. Each client who requests enrollment in the CenterPoint system should be asked to sign a Privacy Notice from CenterPoint, making them aware of their rights and the use of their Individually Identifiable Health Information to obtain payment for their services. 1. Key Data to Capture During Enrollment: All providers are required to assure client enrollment data is up-to-date based on the most current CenterPoint enrollment procedures and training. If enrollment data is not complete prior to service provision, authorizations and claims will be affected. This would include denials of authorizations and claims. The Medicaid information must be provided to the Customer Services Department when requesting an enrollment. If the client has any other third party insurance, including Medicare, this information must also be included in the enrollment request. Clients whose services are paid in part by third party insurance can be enrolled if CenterPoint is to be a secondary payer. 2. Effective Date of Enrollment: Enrollment into the CenterPoint system must be done prior to providing services except in emergency situations. It is the provider’s responsibility to complete the eligibility determination process, including verification of previous enrollment in the CenterPoint system and to complete the enrollment process prior to providing services. Crisis services are provided in an emergency Revised 7/21/15 89 situation are an exception to this rule. In these cases, the provider must enroll the individual within seven (7) days and indicate the date of enrollment as the date that the emergency services were provided. Services with service delivery dates prior to an enrollment date will be denied. 3. Member ID: The Member ID Number identifies the specific client receiving the service and is assigned by the CenterPoint information system. The client must be enrolled in the CenterPoint system in order for a claim to be accepted. In order for the provider to obtain this number, the client must have been successfully enrolled into the CenterPoint information system. All claims submitted with incorrect Member ID numbers, or for clients whose enrollment is no longer active, will be denied. B. Authorizations Required for Payment 1. System Edits: CenterPoint’s information system is specifically designed to look for authorization data prior to paying claims. The information system has edits that are verified, so the provider must be very attentive to what has been authorized to assure maximum reimbursement. 2. Authorization Number and Effective Dates: Each authorization will have a unique number, a start date and an end date. Only services with dates of service within these specific time frames will be paid. Dates and/or units outside these parameters will be denied. 3. Service Categories or Specific Services: Each authorization will indicate specific categories of services or in some cases very specific services that have been authorized. Each service will be validated against the authorization to make sure that the service matches the authorization. Services that are outside of these parameters will be denied. 4. Units of Service: Each authorization will indicate the maximum number of units of service that are being authorized. As each claim is being processed, the system will check to make sure that the units being claimed fall within the units of services authorized. The system will deny any claims that exceed the limits. Providers need to establish internal procedures to monitor units of service against authorizations to avoid having claims denied due to exceeding units of service. 5. Exceptions to Authorization Rule: There are certain services that will be paid without an authorization. These services are limited in scope and are limited in total number to a client, not to a provider. Once the annual limit has been reached for a client, then all services without an authorization, regardless of the provider of the service, will be denied. Providers must be constantly aware of this issue in order to avoid denied claims. Revised 7/21/15 90 C. Payment of Claims and Claims Inquiries (EQR 5.3) Providers must submit claims electronically unless an exception has been established by CenterPoint, allowing an alternative method. Providers are encouraged to produce routine billings on a weekly or bimonthly schedule. 1. Timeframes for Submission of Claims: All claims must be submitted within ninety (90) days of the date of service to assure payment unless otherwise specified in provider’s contract. Claims submitted outside of the allowable billing days will be denied. 2. Process for Submission of Replacement and Voided Claims: Replacement Claim: Providers may submit replacement claims for originally paid claims within one hundred eighty (180) days from the original approval date. Replacement claims submitted past one hundred eighty (180) days from the original approval date will be denied for exceeding billing days and cannot be resubmitted. Once the replacement claim has been received your original claim will be reverted and the replacement claim will be processed according to all CenterPoint billing guidelines. Voided Claims: There is no time limitation restriction for submitting voided claims. They should be submitted as soon as identified. Voided claims will be reverted from our system and the original claim payment will be recouped. 3. AlphaMCS Claims Submission: Providers are contractually required to submit billing electronically. Alpha MCS is a web-based system available to CenterPoint providers. Billing through the AlphaMCS System is Direct Data Entry (DDE) in which an electronic CMS1500 or UB04 is accessed and billing information is entered and submitted to CenterPoint for reimbursement. Providers will receive orientation, training and technical assistance in this process upon their entrance into the LME/MCO network. 4. 837 Claims Submission: Providers will receive orientation, training and technical assistance in this process upon their entrance into the LME/MCO network. The orientation will at a minimum include detailed information on the following: a. Formats b. Multiple Occurrences of Same Service in a Day c. Authorization d. NPI (National Provider Identifier) e. Verification and Notification Revised 7/21/15 91 5. Providers Who Submit Paper Claims: Providers who continue to submit paper claims until they can transition to electronic claims processing will be required to submit an accurate CMS1500 or UB04 billing form with the correct data elements. Inquiries regarding the status of claims should be directed to the CenterPoint Finance Claims Staff at Claims&Billing@cphs.org Contact information can be accessed via the CenterPoint website www.cphs.org. D. Service Codes and Rates: Contract Provisions Publishing of Rates: Provider contracts include a listing of services which they are eligible to provide. All providers are reimbursed at the CenterPoint published rates for the service being provided unless otherwise stated in their contract. Providers must only use the service codes in their contract or reimbursement will be denied as non-contracted services. Providers can submit claims for more than the published rates, but only the published or contracted rate will be paid. If a provider submits a service claim for less than the published rate, the lower rate will be paid. It is the provider’s responsibility to monitor the publishing of rates and to make the necessary changes to their billing systems. E. Standard Codes for Claims Submission Providers will receive orientation, training and technical assistance in this process upon their entrance into LME/MCO network. The orientation will at a minimum include detailed information on the submission claims. CenterPoint provides claims and billing training in a classroom setting and video-based claims training online. The training information is found on CenterPoint’s website at: http://www.cphs.org/AlphaProviderTraining.aspx 1. CPT/HCPCS/Revenue Codes 2. Modifiers 3. Diagnosis Codes 4. Place of Service Codes F. Definition of Clean Claims A clean claim is defined as a claim that has all of the required data elements, is submitted in the correct format and meets the terms of the contract between CenterPoint and the provider. G. Coordination of Benefits CenterPoint is the payer of last resort. Providers are required to collect all first and third party funds prior to submitting claims to CenterPoint for reimbursement. First party payers are the clients or their guarantors. Third party payers are any other funding sources than can be billed to pay for the services provided to the client. This can include worker’s compensation, disability insurance or other health Revised 7/21/15 92 insurance coverage. All claims must identify the amounts collected from both first and third parties and only request payment for any remaining amount. 1. Eligibility Determination Process by Provider: Providers should conduct a comprehensive eligibility determination process whenever a client enters the delivery system. Periodically (no less than quarterly), the provider should update its eligibility information to determine if there are any first or third party liabilities for this client. It is the provider’s responsibility to monitor this information and to adjust billing accordingly. First or third party insurances should be added to the client’s record at the LME/MCO. 2. Obligation to Collect: Providers must make good faith efforts to collect all first and third party funds prior to billing CenterPoint. First party charges must be shown on the claim whether they were collected or not. The CenterPoint IS System has the ability to validate third party payers and can deny or adjust the claim. 3. Reporting of Third Party Payments: Providers are required to record on the claim either the payment or denial information from a third party payer. Copies of the Remittance Advice (ERA) or Explanation of Benefits (EOB) from the insurance company should be retained by the provider if they submit electronic billing. If paper tickets are submitted to CenterPoint the provider is required to submit copies of the ERA or EOB with the claim form to CenterPoint. Providers must bill any third party insurance coverage. This includes worker’s compensation, Medicare, Employee Assistance Programs, etc. Providers must wait a reasonable amount of time in order to obtain a response from the insurance company. However, it is important that providers not exceed the 90-day rule before submitting claims. If an insurance company pays after a claim has been submitted to CenterPoint, the provider must notify CenterPoint and reimburse CenterPoint. H. Response to Claims 1. Remittance Advice: The Remittance Advice is CenterPoint’s way of communicating back to the provider community exactly how each and every service has been adjudicated. CenterPoint provides the Remittance Advice report electronically under the AlphaMCS provider portal. 2. Electronic Remittance Advice (835) – for 837 Providers: Per HIPAA regulations, payers are to supply providers with an electronic Remittance Advice known as the 835. The 835 will report electronically the claims status and payment information. This file is used by the provider’s information system staff or vendor to automatically post payments and adjustment activity to their client accounts. This allows providers the ability to manage and monitor their accounts receivables. 3. Management of Accounts Receivable – Provider Responsibility: Providers must take full responsibility for the management of their client accounts receivable management. CenterPoint produces Remittance Advices based on the current check write schedule. Revised 7/21/15 93 I. Fee-For-Service Equivalency 1. Contract Agreement: Each provider agency will have a contract that defines the terms of payment. On a selected basis some of the smaller agencies will have grant-funded or what is known as Fee-For-Service Equivalency (FFSE) contracts. In these contracts, providers are given a pre-established amount of funding with the expectation that they will provide a determined amount of services for these funds. CenterPoint has developed a process to receive claims against these contracts so that it can monitor the services being provided, but not pay these claims on a Fee-For-Service basis. The information system will price the claims, but then adjust the amount so that the claim is zero paid on the remittance advice. This is known as Fee-For-Service Equivalency (FFSE). This approach cannot be used to pay Medicaid claims. Only State and Local funds can be paid using this methodology. 2. Review of FFSE Process: Once these contracts are active, the provider will submit claims to CenterPoint in the same fashion as all other claims. If the claims are Medicaid claims, then those claims will be paid following the standard Fee-For-Service methodology. However, if the contract for State or Local funds is set up as a Fee-For-Service Equivalency (FFSE), then the claims will be adjudicated as usual except the allowed amount on the claim will be adjusted (via a contractual allowance) to zero. The provider will receive a single detailed remittance showing all claims adjudicated. The FFSE claims will show as being fully adjudicated, but with a zero dollar amount paid. Payments will be made on a monthly basis as determined in contract. 3. Reconciliation: It is important that the provider post these “paid claims” against their client accounts receivable system. Even though these FFSE claims are zero dollars, they are considered paid in full and will be counted against their FFSE contract obligations. J. Claims Investigations of Fraud and Abuse Providers and clients are expected to report suspected fraud and abuse and can do this though a variety of avenues, including a dedicated email address to compliance@cphs.org, the LME/MCO’s toll-free “whistle blower” number at 1-877-372-8302, or by calling any number at CenterPoint and asking for the Compliance Officer. CenterPoint, operating as the LME/MCO, will provide training, orientation and technical assistance to providers upon their entrance into the Network and clients will receive orientation to the LME/MCO system upon enrollment. In the event of any allegation of abuse (e.g. fraud, waste, abuse, over utilization), the provider shall have thirty (30) days to appeal. Appeals may be initiated by following the instructions in this Manual, Section XIII E Provider Disputes. 1. Trends of Abuse and Potential Fraud: One of the primary responsibilities of CenterPoint will be to monitor the provider Network for fraud and abuse. Both the Medicaid and state contracts make CenterPoint responsible for monitoring and conducting internal and external monitoring and periodic audits to assure Revised 7/21/15 94 2. 3. 4. 5. compliance with all federal and state laws and in particular the Medicare/Medicaid fraud and abuse laws. Specifically, CenterPoint will need to validate the presence of material information to support billing of services consistent with Medicaid and state regulations. CenterPoint will systematically monitor the paid claims data to look for trends or patterns of abuse. Audit Process: CenterPoint has the responsibility to assure that funds are being used for the appropriate level and intensity of services as well as in compliance with federal, state and general accounting rules. The CenterPoint Compliance Department conducts billing audits and investigations for all contract providers. The Finance Department is primarily responsible for collecting any paybacks that result from audits. The Finance Department will work with the Compliance Department and provider in the collection of any determined paybacks or overpayments. Role of Finance Department: The Finance Department will assist the Compliance Department with the review of financial reports, financial statements and accounting procedures. Voluntary Repayment of Claims: It is the provider’s responsibility to notify CenterPoint in writing of any claims billed in error that will require repayment. Reporting to State and Federal Authorities: In each case where CenterPoint investigates a credible allegation of fraud, CenterPoint shall provide DMA Program Integrity with the following information on the DMA approved template: Subject (name, Medicaid provider ID, address, provider type) Source/origin of complaint Date reported to CenterPoint or if developed by the CenterPoint, the date CenterPoint initiated the investigation. Description of suspected intentional misconduct, with specific details including: o The category of service o Factual explanation of the allegation o Specific Medicaid statutes, rules, regulations, or policies violated o Dates of conduct. Amount paid to the provider for the last three years or during the period of the alleged misconduct, whichever is greater. All communications between CenterPoint and the provider concerning the conduct at issue, when available. Contact information for CenterPoint staff persons with practical knowledge of the workings of the relevant programs. Sample/exposed dollar amount, when available. K. Repayment Process/Paybacks The Finance Department is responsible for the recovery of funds based on any audit findings. If CenterPoint determines a provider has failed to comply with State, Federal, Medicaid or any other revenue source requirements, CenterPoint will recoup the amount owed from current and/or future claims. If payback amount exceeds outstanding provider claims, CenterPoint will invoice the provider the amount Revised 7/21/15 95 owed. Providers shall have thirty (30) calendar days from the invoice date to pay back the total amount owed. If a provider fails to repay funds identified CenterPoint reserves the right to take action to collect the outstanding balance from the provider. Payment plans may be established through the compliance department and the development and terms of these plans are at the sole discretion of the compliance department. If CenterPoint or a provider determines they have received revenues as a result of an error or omission, CenterPoint will consult with the provider on the method of repayment. If the provider fails to repay CenterPoint within the specified period, CenterPoint will recoup the amount owed from current and/or future claims. If CenterPoint, through an audit or review, determines a provider has been paid for a service or a portion of a service that should have been disallowed, CenterPoint will recoup the amount owed from current and/or future claims. If payback amount exceeds outstanding provider claims, CenterPoint will invoice the provider the amount owed. Providers shall have thirty (30) calendar days from the invoice date to pay back the total amount owed. If a provider fails to repay funds identified CenterPoint reserves the right to take action to collect the outstanding balance from the provider. CenterPoint may establish a payment plan with the provider for repayment of funds. If CenterPoint, through an audit or review, determines a provider has been paid for a claim that was fraudulently billed, CenterPoint will recoup the amount owed from current and/or future claims. If payback amount exceeds outstanding provider claims, CenterPoint will invoice the provider the amount owed. The provider shall have thirty (30) calendar days from the invoice date to pay back the total amount owed. Fraudulent billing may include, but is not limited to, unbundling services, billing for services by non-credentialed or nonlicensed staff, or billing for a service that the provider never rendered or for which documentation is absent or inadequate. Revised 7/21/15 96 SECTION XII: STANDARDS AND REGULATORY COMPLIANCE CenterPoint is committed to working in collaboration with the network of providers to achieve the highest standards of quality in service delivery. A. Quality Improvement CenterPoint maintains a strong commitment to continual improvement of its services and those services provided directly to clients. A focus on quality requires basic principles, which include: Commitment to the involvement of the clients in all areas and levels of the service system in regards to analysis, planning, implementing changes, and assessing quality and outcomes Commitment to strengthen systems and processes – By viewing the system as a collection of interdependent processes we can understand how problems occur and can strengthen the system as a whole Encouraging participation and teamwork – Every member of the system can help assure quality if they are included in processes and are empowered to solve problems and recommend improvements Decisions are based on reliable information – By collecting and analyzing accurate, timely and objective data we can diagnose and solve system problems and measure progress Improvement in communication and coordination – Different members of the system can work together to improved quality if they share information freely and coordinate their activities CenterPoint maintains an established quality structure that assures the participation of all persons and agencies involved in the service system. Committees include: Global CQI Committee (GCQIC) CenterPoint Area Providers Council (CAPC) Consumer and Family Advisory Committee (CFAC) Human Rights Committee (HRC) Clinical Advisory Committee (CAC) Credentialing Committee The continual self-assessment of services and operations and the development and implementation of plans to improve outcomes to clients is a value and expectation that CenterPoint extends to its network providers. Network providers are required to be in compliance with all Quality Assurance and Improvement standards outlined in North Carolina Administrative Code as well as the CenterPoint contract. These items include: The establishment of a formal Quality Improvement Committee to evaluate services, plan for improvements and assess progress made towards goals The assessment of need as well as the determination of areas for improvement should be based on accurate, timely, valid data. The provider’s improvement system, as well as systems used to assess services, plans for improvement and their effectiveness will be evaluated by CenterPoint on a scheduled basis Revised 7/21/15 97 B. Performance Measurement Data collection and verification: CenterPoint is required to measure outlined performance indicators in the following domains: Access, Availability, Quality of Care, Quality of Services, Appropriateness of Services, System Performance and Satisfaction, in order to assure compliance with DMH & DMA contract requirements. Performance improvement: CenterPoint will complete Quality Improvement Projects (QIPs) as indicated in DMA and DMH contracts and URAC accreditation standards. These Quality Improvement Projects may require provider participation. C. Performance Monitoring An important part of CenterPoint’s role as LME/MCO is to monitor the performance of providers in its network CenterPoint maintains the following systems to assist in monitoring the health and safety of clients, rights protections and quality of care: 1. Monitoring of Incidents: An incident is an event at a facility or in a service that is likely to lead to adverse effects upon a client. Incidents are classified into several categories according to the severity of the incident. Providers are required to develop and maintain a system to collect documentation on any incident that occurs in relation to a client. This includes all state reporting regulations in relation to the documentation and reporting of critical incidents. Providers must enter all Level II and Level III incidents into a state hosted database (IRIS) and Level I incidents must be documented internally by each provider. As part of its quality management process, it is important for the provider to implement procedures that assure the review, investigation and follow up for each incident that occurs through its own internal Quality Management process. This includes: A review of all incidents on an ongoing basis to monitor for trends and patterns Strategies aimed at the reduction/elimination of trends/patterns Documentation of the efforts at improvement as well as an evaluation of ongoing progress Mandatory reporting requirements are followed Enter level II and III incidents into the state’s Incident Response Improvement System (IRIS) There are specific state laws governing the reporting of abuse, neglect or exploitation of clients. It is important that the provider’s procedures include all of these requirements. If a report alleges the involvement of a provider’s staff in an incident of abuse, neglect or exploitation, the provider must assure that clients are protected from involvement with that staff person until the allegation is proved or disproved. All allegations of abuse, neglect or exploitation by staff persons must be reported to the DHHS Health Care Personnel Revised 7/21/15 98 Registry. The agency must take action to correct the situation if the report of abuse, neglect or exploitation is substantiated. 2. CenterPoint Incident Review Process: CenterPoint is required, under North Carolina Administrative Code, to monitor certain types of incidents that occur within providers in its network, as well as, providers who while not in CenterPoint’s network, operate services in one of the four (4) counties CenterPoint area covers. Regulations regarding the classification of incidents (Level I, II, or III) as well as requirements related to the submission of incident reports to home and host LME/MCOs and state agencies can be located in North Carolina Administrative Code. CenterPoint is required to monitor the state IRIS system. For more information regarding these classifications, please see the following website: http://www.ncdhhs.gov/mhddsas/providers/NCincidentresponse/index.htm CenterPoint Provider Relations Specialists shall review all incidents when received by CenterPoint for completeness, appropriateness of interventions, achievement of short and long term follow up both for the individual client, as well as the provider’s service system. If questions/concerns are noted when reviewing the incident report the Provider Relations Specialist will work with the provider to resolve these. If concerns are raised related to client’s care or services or the provider’s response to an incident, the Network Operations Department may elect to conduct an onsite review of the provider. If at all possible the review will be coordinated with the provider and, if deficiencies are found, the Provider Relations Specialist will work with the provider on the implementation of a plan of correction. 3. Monitoring to Assure Quality of Care: The CenterPoint Network Management Department is charged with conducting routine monitoring and compliance reviews utilizing state mandated forms to perform post payment reviews of paid claims and onsite visits to include audits of medical records, administrative files, the physical environment and other areas of service including cultural competency reviews. Network Management is the department at CenterPoint that performs compliance safety reviews of non-licensed programs and sites, monitors providers, reviews critical incidents, death reports and restrictive interventions as an important role in assuring the protection of rights and the health and safety of clients. Network Operations reviews incidents reported and determines whether any follow up is needed. Network Operations may conduct investigations of incidents reported directly by providers on Incident Reports, as well as reports provided by clients, families and the community. 4. Grievances: CenterPoint may receive grievances from providers, stakeholders, clients, families, legal guardians or anonymous sources regarding CenterPoint’s provider network, and/or a specific provider’s services or staff. Based on the nature of the grievance, CenterPoint’s Network Revised 7/21/15 99 Management Department may choose to investigate the grievance in order to determine its validity. Investigations may be announced or unannounced. It is very important that the provider cooperate fully with all investigative requests. It is important to understand that this is a serious responsibility that is invested in CenterPoint, and that we must take all grievances very seriously until we are able to resolve them. CenterPoint management of grievances is carefully monitored by DMA and CenterPoint maintains a data base where all grievances and resolutions are recorded. CenterPoint’s Network Management Department maintains documentation on all follow up and findings of any grievance investigation and a written summary will be provided to the provider. If problems are identified, the provider involved may be required to complete a plan of correction. 5. Client Satisfaction Surveys and Mystery Shopping Program: CenterPoint values the satisfaction of clients/family members/stakeholders with service provided in the CenterPoint Network. CenterPoint has various ways client satisfaction is measured. These include annual surveys and “mystery shopping.” The goal of these initiatives is to gather feedback on how various CenterPoint departments perform during random and anonymous monitoring. This system has provided excellent information that has been used to pinpoint the need for additional training of staff D. Corporate Compliance Providers and clients are expected to report suspected fraud and abuse and can do this though a variety of avenues, including a dedicated email address to compliance@cphs.org, the LME/MCO’s toll-free “whistle blower” number at 1-877-372-8302, or by calling any number at CenterPoint and asking for the Compliance Officer. CenterPoint, operating as the LME/ MCO, will provide training, orientation and technical assistance to providers upon their entrance into the network and clients will receive orientation to the LME/MCO system upon enrollment. Providers are advised that CenterPoint expects all its employees to practice honesty, directness and integrity in dealings with one another, business partners, the public, the business community, internal and external stakeholders, “customers,” suppliers, elected officials, and government authorities. 1. Primary Areas Covered by Corporate Compliance: Corporate compliance deals with the prohibition, recognition, reporting and investigation of suspected fraud, defalcation, misappropriation and other similar irregularities. The term “fraud” includes misappropriation and other irregularities including dishonest or fraudulent acts, embezzlement, forgery or alteration of negotiable instruments such as checks and drafts, misappropriation of an agency’s, employee, customer, partner or supplier assets, conversion to personal use of cash, securities, supplies or any other agency assets, unauthorized handling or Revised 7/21/15 100 reporting of agency transactions, and falsification of an agency’s records, claims or financial statements for personal or other reasons. The above list is not all-inclusive but intended to be representative of situations involving fraud. Fraud may be perpetrated not only by an agency’s employees, but also by agents and other outside parties. All such situations require specific action. Within any agency, management bears the primary responsibility for detection of fraud. The Corporate Compliance Department in particular is accountable to implement the Compliance Plan and monitor any potentially fraudulent situations. 2. Corporate Compliance Plan: Agency providers that receive in total more than $300,000 in Federal funds must develop a formal Corporate Compliance Plan that includes procedures designed to guard against fraud and abuse. The plan should include: a. An internal audit process to verify that services billed were furnished by appropriately credentialed staff and appropriately documented b. The plan will assure that staff performing services under the CenterPoint contract have not been excluded from participation in Federal Health Care Programs under either Section 1128 or 1128A of the Social Security Act. The agency consults with the Health and Human Services Office of the Inspector General’s list of Excluded Individuals, the Medicare Exclusion Databases (MED), and the Excluded Parties Listing System (EPLS) c. Written policies, procedures and standards of conduct that articulate the agency’s commitment to comply with all applicable State and Federal standards for the protection against fraud and abuse d. Designation of a Compliance Officer and Compliance Committee e. A training program for the Compliance Officer and agency employees f. Systems for reporting suspected fraud and abuse by employees and clients and protections for those reporting g. Provisions for internal monitoring and auditing h. Procedure for response to detected offenses and for the development of corrective action plans i. Reporting to monitoring and law enforcement agencies, including CenterPoint Note: All providers must monitor for the potential for fraud and abuse and take immediate action to address reports or suspicion. E. Monitoring and Auditing CenterPoint takes reasonable steps to monitor and audit corporate compliance, including the establishment of monitoring and auditing systems that are reasonably designed to detect violations by CenterPoint employees and agents of the agency. CenterPoint has established a reporting system to support efforts to identify non-compliance issues. Providers may access this reporting system’s toll free number at 1-877-372-8302. Reporters may make reports anonymously or provide their name. Reports may also be made by calling 1-336-714-9100 and asking for the Corporate Compliance Officer. Revised 7/21/15 101 It is a violation of CenterPoint policy to intimidate or impose any form of retribution on an employee, agent, or provider that utilizes our reporting system in good faith to report suspected violations (except that appropriate action may be taken against such employee, agent, or provider if such is implicated as one of the wrongdoers). F. Investigation of Violations If CenterPoint receives information regarding an alleged corporate compliance violation, an investigation will occur to evaluate such information as to gravity and credibility. CenterPoint may also disclose the results of investigations to regulatory and/or law enforcement agencies depending on the nature of the allegation. G. Client Records Retention and Disposal Standards Providers are responsible for safeguarding records accrued during the course of providing publicly-funded mental health, developmental disabilities, or substance abuse services as outlined in state and federal regulations. Retention and disposition requirements for publicly-funded mental health, developmental disabilities, and substance abuse services are governed by the Records Retention and Disposition Schedule (APSM 10-5 and APSM 1-3). The current retention schedule is as follows: Providers shall retain service records of adult Consumers 11 years after the date of the last encounter. Service records of minor Consumers who are no longer receiving services shall be retained for 12 years after the minor has reached the age of majority (18 years of age). Providers may consult the following manual websites for additional and updated information on retention: • http://www.ncdhhs.gov/mhddsas/statspublications/Policy/apsm10-3retentionupdated5-05.pdf • http://www.ncdhhs.gov/mhddsas/providers/recordsmanagement/index.htm • http://www.ncdcr.gov/archives/ForGovernment.aspx • http://www.records.ncdcr.gov/local/2011_10_LocalProviderRetention_Official.pdf Original service records remain the property and responsibility of the provider and should not be relinquished to another provider or disposed of outside the parameters of record retention requirements CenterPoint shall also require Providers to submit a plan for maintenance and storage of all records for approval by the PIHP or transfer copies of medical records of Enrollees served pursuant to this Contract to PIHP in the event that provider closes its North Carolina business operations, whether the closure is due to retirement, bankruptcy, relocation to another state, or any other reason. The PIHP has the sole discretion to approve or disapprove such plan. PIHP shall not be held liable for any Provider records not stored, maintained or transferred pursuant to this provision so long as it has attempted, in good faith, to obtain a written plan for maintenance and storage or a copy of such records from the Provider. If the Provider's contract is terminated or if the Provider closes network operations (but continues to have operations elsewhere in the State), the Provider may either provide copies of Medical records of Enrollees to PIHP or submit a plan for maintenance and storage of all records for approval by the PHIP. The PHIP has the sole discretion to approve or disapprove such plan. PIHP shall not be held liable for any Provider Revised 7/21/15 102 records not stored, maintained or transferred pursuant to this provision so long as it has attempted, in good faith, to obtain a written plan for maintenance and storage or a copy of such records from the Provider. Abandoned Records: Abandonment of records is a serious HIPAA and contractual violation which can result in sanctions and financial penalties. Providers must maintain network client records in compliance with confidentiality standards set out in APSM-45-1 and the HIPAA Privacy and Security Regulations (including the HITECH Act) and the provider’s Procurement Contract with CenterPoint Human Services. H. Minimum Standards of Documentation in Client Medical Records Providers are expected to meet all standards of documentation for client medical records. Providers will adhere to the medical record regulations and standards set forth in state and federal rules and statutes. These include: • • • • • • • APSM 45-2: Records Management and Documentation Manual for Providers of PubliclyFunded MH/DD/SA Services, CAP-MR/DD Services, and Local Management Entities APSM 45-1: Confidentiality Rules APSM 10-3: Records Retention and Disposition Manual NC MN/DD/SAS Health Plan and NC Innovations Waivers HIPAA Privacy and Security Regulations, including the HITECH Act Provider Procurement and State Funded Contract with CenterPoint Human Services Clinical Coverage Policies and Service Definitions found therein Updates to documentation standards may be found at state sources, including: http://www.ncdhhs.gov/mhddsas/servicedefinitions/index.htm http://www.ncdhhs.gov/mhddsas/statspublications/manualsforms/aps/apsm1026servicedef1-03.pdf http://www.ncdhhs.gov/dma/mp/mpindex.htm. Providers are responsible for regularly consulting with state sources to check for changes in documentation standards. Provider will include in the client medical record all information developed or received by the provider about the client during the course of treatment. Per the Records Management and Documentation Manual, client medical records should include – at a minimum – the following: • • • • • • • • Client’s name Service record number Medicaid ID number Demographic information on a service record face sheet Emergency contact information Informed written consent for treatment Informed written consent for planned use of restrictive intervention Written consent granting permission to seek emergency care from a hospital or physician Revised 7/21/15 103 • • • • • • • • • • • • • • • • • • • • • • • • • • • • Informed written consent for participation in research projects (where applicable) Written consent to release information Documentation regarding confidentiality Evidence of written summary of client rights given and explained to client/legally responsible person Screening Documentation of strategies used to address the individual’s presenting problem Admission/eligibility assessments and other clinical evaluations, completed according to the governing body policy and prior to the delivery of services Diagnoses and list of health history and risk factors A Person-Centered Plan Cost summary Signed service plan/treatment plan (where PCP is not required) Documentation of incidents Service notes for documentation of services provided, including interventions, treatment, effectiveness, progress toward goals, service coordination and other case management activities Copies of relevant legal papers Documentation of medication allergies Documentation of medications and a Medication Administration Record Medication orders Copies of lab tests Identification of team members Documentation of care coordination Clinical or level of functioning measurement tools Referral documentation Treatment decision-making process Advance directives Service authorizations Incoming and outgoing correspondence Discharge plans Discharge summaries It is recommended, but not required, that information needed for reimbursement purposes be filed in the client medical records. Providers should record and retain billing records and related information pursuant to the specific requirements of the payers involved. I. Information Systems Each provider must have Internet Capacity. Each provider must comply with HIPAA Security Regulations that includes the ability to encrypt emails including PHI (or IIHI) sent both internally and externally. Please go to CMS web site as a further resource -- http://www.cms.hhs.gov When you get to the CMS.gov website, click on the Research, Statistics, Data & Systems tab for additional links. Revised 7/21/15 104 SECTION XIII: REVIEW PROCESS FOR PROVIDERS AND RECONSIDERATION (NC G.S. 108C-12; URAC N-NM 14; URAC N-NM 15) The following is a delineation of the process for the review of actions taken against providers by CenterPoint. An action is defined as an event in which CenterPoint applies sanctions such as the requirement for a Plan of Correction, payback or referral freeze. The action may be the result of findings from audits, quality of services evaluations, investigations or report by outside investigative authorities. An action also includes a denial (in whole or in part) of a provider’s request to employ a family member to serve a client. A. Roles and Responsibilities of the Network Management Department The Network Management Department conducts routine, focused, targeted and investigative provider audits of service delivery, clinical and billing documentation. Note: The CenterPoint Corporate Compliance unit may also conduct audits related to allegations of Medicaid fraud, waste or abuse. Network Management: 1. Determines the need for a plan of correction based on the outcome of the audit, investigation, or review 2. Determines provider paybacks 3. Makes reports to Departments of Social Services regarding client care and protection 4. Reports to the Division of Health Service Regulation (DHSR) any infractions as required by NC Administrative Rule or by contract 5. Reports to CenterPoint Program Integrity and/or NC DMA regarding potential fraud, waste or abuse 6. Reports licensure issues to applicable agencies or boards Timeline: CenterPoint Network Management staff, or the assigned department, shall make a good faith effort to acknowledge grievances and Quality of Care Concerns regarding a provider within 3 business days of receipt of the concern. Grievances/Quality of Care Concerns are resolved as quickly as possible; CenterPoint strives to have all grievances/Quality of Care Concerns resolved within thirty (30) days B. Roles and Responsibilities of the CenterPoint Network Management Cross-Functional Team The CenterPoint Network Management Cross-Functional Team (CFT) provides oversight of Network Management Department actions regarding provider audits, investigations, and imposition of sanctions. It also collaborates with other CFTs and departments in regard to provider enrollment and disenrollment matters, and the addition of services. The Network Management CFT is responsible for reviewing recommendations of sanctions or penalties against providers brought before it by Network Management staff or directors/managers from other departments. Generally, provider violations and corresponding sanctions are found in internal procedures Revised 7/21/15 105 (see sanctions grid, NM/MP-3.01-6). Where there is evidence that a provider’s actions pose a significant risk to client safety or where there is evidence that a provider’s actions result in significant waste, then Network Department staff or manager/directors from other departments may recommend the imposition of sanctions to the Network Management CFT. The Network Management CFT may approve, deny, delay, or approve with amendments any recommendations to impose sanctions. The Network Management CFT determines the appropriateness and length of a penalty or sanction and may set conditions upon which a sanction against a provider can be lifted. Sanctions the Network Management CFT may consider include, but are not limited to: 1. A corrective action plan 2. Suspension of referrals 3. Transfer of CenterPoint-funded clients to another provider 4. Additional audits 5. Interest charges on paybacks 6. Loss of enrollment/contract The Network Management CFT directs Network Management staff to notify the provider of any sanctions imposed against it. C. Roles and Responsibilities of the Credentialing Committee The Credentialing Committee is tasked with assuring that licensed practitioners, agencies and hospitals meet standards for entrance into and ongoing participation in the CenterPoint provider network. The Committee is made up of CenterPoint staff and local practitioners that are already members of the CenterPoint network. Each clinical specialty is represented on the Committee. The Committee reviews licensure, education, sanctions, criminal background checks and other documents to decide if the applicant meets CenterPoint credentialing standards. If those standards are met, the Committee credentials the practitioner. A credentialed practitioner can enter the CenterPoint network and bill for services delivered only after a contract is fully executed. NOTE: URAC standards require that the Credentialing Committee have the final authority to approve or disapprove applications by providers for network participation status. Providers already credentialed have the right to contest decisions made by the Credentialing Committee to de-credential the provider or otherwise change their credentialed status. The Credentialing Committee may change a provider’s credentialing status (i.e. suspension or revocation) on the basis of an action or non-action that is found to violate CenterPoint’s standards of practice. The Credentialing Committee will report to the licensing boards for licensed practitioners or t other regulatory agencies as appropriate, based on audit findings. D. Roles and Responsibilities of the Finance Department The Finance Department validates the payback findings by Network Operations or Corporate Compliance Departments and determines the availability of funds from outstanding claims to recover the amount of Revised 7/21/15 106 the payback. The Finance Department may pursue a variety of options to enforce the assessed payback, including withholding of future claims payments, invoicing and collecting from the provider organization (with collection efforts to include initiating legal action and obtaining a judgment and execution of the judgment against the provider for the payback), or referring the assessment to a third party collection agency. The Finance Department has responsibility to assess provider paybacks arising from Coordination of Benefits (COB) audits. E. Provider Disputes Note: Based on URAC standards, the Credentialing Committee has the final authority to approve or disapprove applications by providers for network participation status. Credentialing Committee decisions to exclude an applicant from the network are not subject to the dispute process. Credentialing Committee decisions to de-credential a contracted provider is subject to the Provider Competence Dispute Procedure. The provider dispute processes only apply to contracted network providers. Not all contracted provider disputes are subject to the dispute process. For example, the dispute process is not applicable to explicit requirements stated in the provider contract or to medical necessity appeals. CenterPoint seeks to resolve provider issues, concerns or questions at the lowest level possible. As a first step in resolving issues, the following contacts may be utilized: Provider questions or concerns: Contact assigned CenterPoint Provider Liaison Authorizations: Contact Utilization Management at lawarren@cphs.org. Claims: Contact Billing & Claims Manager at Billing&Claims@cphs.org. CenterPoint implements various mechanisms consistent with its written agreements, including, but not limited to, provider contracts and memoranda of agreement, (“Contracted Provider[s]”), to address alleged contractual violations by Contracted Providers. At times, these actions taken by CenterPoint will lead to provider disputes with CenterPoint. CenterPoint respects the rights of provider and employs a formal process to address significant Contracted Provider disputes in a fair, respectful, impartial and timely manner. Note: Service appeals regarding reduction, suspension or termination of services are subject to CenterPoint procedures and information set forth in Section V of this CenterPoint Provider Manual. 1. Types of Provider Disputes: a. Provider Administrative Disputes – Applies only to contracted network providers and is not applicable to explicit requirements stated in the provider contract or to provider medical necessity appeals ( e.g., issues related to timely filing of claims, network accessibility issues, failure to submit requested medical records, appeals of administrative service denials). b. Provider Professional Competence Disputes – Applies to those disputes regarding a provider’s professional competence or conduct that could result in a change in provider Revised 7/21/15 107 credentialed status (e.g. ethics violations, clinical boundaries, dual relationships, professional competence to perform contracted services, and the appropriateness or quality of professional services including assessment, treatment, consultation, and referral). CenterPoint establishes specific procedures that address the process for resolution of provider disputes. The procedures may be accessed on the CenterPoint website at www.cphs.org. SECTION XIII: OFFICIAL COMMUNICATION BULLETINS All Official Communication Bulletins are posted on the North Carolina Department of Health and Human Services, Division of Mental Health, Developmental Disabilities and Substance Abuse Services (NC DHHS - Division of MH/DD/SAS) website at http://www.ncdhhs.gov/mhddsas/. Revised 7/21/15 108 SECTION XV: GLOSSARY OF TERMS Ability-to-Pay Determination: The amount a client is obligated to pay for services. The ability to pay is calculated based on the client’s income, and number of dependents. The Federal Government Poverty Guidelines are used to determine the client’s payment amount. See http://www.medicaid.gov/MedicaidCHIP-Program-Information/By-Topics/Eligibility/Eligibility.html Abuse: Provider practices that are inconsistent with sound fiscal, business, or medical practices, and result in an unnecessary cost to the Medicaid program, or in reimbursement for services that are not medically necessary or that fail to meet professionally recognized standards for health care. It also includes beneficiary practices that result in unnecessary cost to the Medicaid program. (Guidelines for Addressing Fraud and Abuse in Medicaid Managed Care, October 2000) Customer Services/ Access Line: Access management is a critical function of the LME/MCO. CenterPoint is responsible for timely response to the needs of clients and for quick linkages to qualified providers of the network. To assure the simplicity of the system requested by clients and stakeholders, CenterPoint will maintain a toll-free call system to receive all inquiries. This will include information, access to care, emergency and network provider assistance. The toll-free call system will rely on information systems management software to assist in tracking and responding to calls. Action: Pursuant to 42 C.F.R. § 438.400, “action” is defined as the denial or limited authorization of a requested service, including the type or level of service; the reduction, suspension, or termination of a previously authorized service; the denial, in whole or in part, of payment for a service; the failure to provide services in a timely manner, as defined by the State; the failure of PIHP to act within the timeframes provided in 42 C.F.R. 438.408(b); or, for a rural area resident with only one MCO, the denial of an Enrollee’s request to obtain services outside the network under the following circumstances: a. When services from any other provider (in terms of training, experience, and specialization as determined by the PIHP) are not available in the Network b. From a provider not part of the PIHP Closed Network who is the main source of a service to the Enrollee—provided that the provider is given the same opportunity to become a participating provider as other similar providers. If the provider does not choose to join the Network or does not meet the qualifications, the Enrollee shall be given a choice of participating providers and shall be transitioned to a participating provider within 60 days. c. Because the only plan or provider available does not provide the service because of moral or religious objections. d. Because the Enrollee’s provider determines that the Enrollee needs related services that would subject the Enrollee to unnecessary risk if received separately and not all related services are available within the network. e. The State determines that other circumstances warrant out-of-network treatment. Adjudicate: A determination to pay or reject a claim. Revised 7/21/15 109 Administrative Review: A review of documentation to determine whether CenterPoint procedures were followed, and if any additional information provided warrants a change in a previous determination. Agency: An Area Facility as defined by NC G.S. §122C-3 subsection 14A. An Agency may deliver a number of services, typically including enhanced benefit Medicaid services, submits and bills claims under a federal tax ID number. ANSI: American National Standards Institute Advanced Directive: A communication given by a competent adult which gives directions or appoints another individual to make decisions concerning a patient's care, custody or medical treatment in the event that the patient is unable to participate in medical treatment decisions. Appeal: A request for review of an action, as “action” is defined in this glossary. Appellant: An individual filing an appeal. Assessment: A procedure for determining the nature and extent of need for which the individual is seeking services. Authorized Service: Medically necessary services pre-approved by the LME/MCO. Basic Augmented Services: The Basic Augmented Benefit package includes those services that will be made available to Medicaid – entitled individuals and, to the extent the resources are available, to non Medicaid individuals meeting Priority population criteria. An individual requiring this level of benefit is in need of more that the automatically authorized (unmanaged) eight (8) or sixteen (16) visits in order to maintain or improve his/her level of functioning. An Authorization for the services available in this level will need to be requested through CenterPoint’s Utilization Management Unit. Authorization is based on the client’s need and medical necessity criteria for the services requested. Basic Benefit Plan: The Basic Benefit package includes those services that will be made available to Medicaid-entitled individuals and, to the extent resources are available, to non- Medicaid individuals. These services are intended to provide brief interventions for individuals with acute needs. The Basic Benefit package is accessed through a simple referral from the Customer Services Department following a screening, triage and referral process. Once the referral is made, there are no prior authorization requirements for these services. Referred individuals can access up to eight (8) visits for Adults ages twenty-one (21) and up and sixteen (16) visits for children and adolescents below age twenty-one (21) from the Basic Benefit package from any provider enrolled in the CenterPoint provider network. Benchmark: A standard by which something can be measured, judged, or compared. Best Practices: Recommended practices, including Evidenced-Based Practices, that consist of those clinical and administrative practices that have been proved to consistently produce specific, intended Revised 7/21/15 110 results, as well as, Emerging Practices for which there is a preliminary evidence of effectiveness of treatment. Billing Audit: An audit conducted by CenterPoint to assess the presence of appropriate documentation to support claims submitted for payment by CenterPoint. Business Associate: A person or organization that performs a function or activity on behalf of a covered entity but is not part of the covered entity’s work force. A business associate can also be a covered entity in its own right. See the HIPAA definition as it appears in 45 CFR 160.103. CALOCUS: Child and Adolescent Level of Care Utilization System – A standardized measure of level of care needs for children and adolescents. Care Coordination: Care Coordination is monitoring of an individual clients’ care and services, including follow–up activities, as well as, assistance to clients in accessing care on non–plan services, including referrals to providers and other community agencies. Catchment Area: Geographic Service Area meaning defined grouping of counties Clean Claim: A “Clean Claim” is a claim that can be processed without obtaining additional information from the provider of the services or a third party. It does not include a claim under review for medical necessity, or a claim from a provider that is under investigation by a governmental agency for fraud or abuse. Claim: A claim is a request for reimbursement under a benefit plan for services. Client: The term “client” is defined in the NC G.S. §122C-3 (6). CMS: Centers for Medicare and Medicaid Services Critical Access Behavioral Healthcare Agency (CABHA): A Critical Access Behavioral Health Agency (CABHA) is a provider who delivers a comprehensive array of mental health and substance abuse services (does not include intellectual/developmental disability services). The role of a CABHA is to assure that critical services are delivered by a clinically competent organization with appropriate medical oversight and the ability to deliver a robust array of services. CABHAs assure client care is based upon a comprehensive clinical assessment and appropriate array of services for the population served. A CABHA is required to offer the Core Services, as well as medical/psychiatric and clinical oversight. Concurrent Review: A review conducted by the LME/MCO during a course of treatment to determine whether services meet medical necessity criteria and quality standards; whether services should continue as prescribed; or whether services should be terminated, changed or altered. Revised 7/21/15 111 Client: A person enrolled (“recipient”)in the North Carolina Medicaid program; may be used to refer to an individual who needs or is receiving services for treatment of a mental health, intellectual and/or developmental disability, or substance use condition. Contractor: An individual or entity providing services to the LME/MCO described in either the Procurement Contract for Provision of Services to Clients with Disabilities or the Consultant Contract for the Provision of Services. Covered Services: The service which the LME/MCO agrees to provide, or arranges to provide to all clients. Credentialing: The review process to approve licensed practitioners, agencies and hospitals that have applied to participate in the LME/MCO network of providers. Crisis Intervention: Unscheduled assessment and treatment for the purpose of resolving an urgent/emergent situation requiring immediate attention. Crisis Plan: A Crisis Plan is an individualized written plan developed in conjunction with client and treatment team. The Plan contains information to assist in deescalating a crisis as well as clear directives to the individual crisis workers or others involved. Crisis plans are developed for clients at risk for inpatient treatment, incarceration or out-of-home placement. Cultural Competency: The understanding of the social, linguistic, ethnic and behavioral characteristics of a community or population and the ability to translate systematically that knowledge into practices in the delivery of behavioral health services. Such understanding may be reflected, for example, in the ability to identify and value differences; acknowledge the interactive dynamics of cultural differences; continuously expand cultural knowledge and resources with regard to populations served; collaborate with the community regarding service provisions and delivery; and commit to cross-cultural training of staff and develop policies to provide relevant, effective programs for the diversity of people served. Days: Except as otherwise noted, refers to calendar days. "Working days or "business day" means day on which CenterPoint is officially open to conduct its affairs. Intellectual/Developmental Disabilities (I/DD): 1. Impairment of general intellectual functioning and adaptive behavior that occurs before age twenty-two (22) which; 2. Substantial limitations in three (3) of seven (7) more major life functions (self-care, expressive and receptive language, learning, mobility, self-direction, capacity for independent living, economic self-sufficiency); 3. IQ of sixty-nine (69) or below; 4. Impairment has continued since its origination or can be expected to continue indefinitely. Denial of Service: A determination made by CenterPoint in response to a Network Provider’s request for approval to provide in-plan services of a specific duration and scope which: Revised 7/21/15 112 1. Disapproves the request completely; or 2. Approves provision of the requested service(s), but for a lesser scope or duration than requested by the provider; (an approval of a requested services which includes a requirement for a concurrent review by CenterPoint during the authorized period does not constitute a denial); or 3. Disapproves provision of the requested service(s), but approves provision of an alternative service(s). Dispute Resolution Process: CenterPoint process to address verbal concerns, grievances and/or disputes by providers in a consistent manner. DMA: The State of North Carolina’s Division of Medical Assistance DMH/DD/SAS: The State of North Carolina’s Division of Mental Health, Developmental Disabilities and Substance Abuse Services. Eligibility: The determination that an individual meets the requirements to receive services as defined by the payer. Emergency Medical Condition: A medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical attention to result in: 1. Placing the health of the individual (or with respect to a pregnant woman, the health of the woman or her unborn child) in serious jeopardy 2. Serious impairment to bodily functions, or 3. Serious dysfunction of any bodily organ or part Emergency Services: With respect to a member, covered inpatient and outpatient services that: 1. Are furnished by a provider that is qualified to furnish such services; and, 2. Are needed to evaluate or stabilize an emergency medical condition as defined above. Emergent Need - Mental Health: A life threatening condition in which a person is suicidal, homicidal, actively psychotic, displaying disorganized thinking or reporting hallucinations and delusions that may result in self-harm or harm to others, and/or vegetative signs and is unable to care for self. Emergent Need - Substance Abuse: A life threatening condition in which the person is by virtue of their use of alcohol or other drugs, suicidal, homicidal, actively psychotic, having disorganized thinking or reporting hallucinations and delusions which may result in self-harm or harm to others, and/or is unable to adequately care for self without supervision due to the effects of chronic substance abuse or dependence. Enrollment (Network): The process of granting a credentialed and contracted provider of behavioral health services the ability to bill for Medicaid-funded services to individuals whose Medicaid originates in one of the CenterPoint catchment area counties. Revised 7/21/15 113 Enhanced Benefit Plan: Includes those services, which will be made available to Medicaid entitled individuals and non-Medicaid individuals meeting priority population criteria. Enhanced Benefit services are accessed through a person-centered planning process. Enhanced Benefit services are intended to provide a range of services and supports, which are more appropriate for individuals seeking to recover from more severe forms of mental illness and substance abuse and with more complex service and support needs as identified in the person-centered planning process. Enrollment: Action taken by the Division of Medical Assistance (DMA) to add a Medicaid recipient’s name to the monthly Enrollment report. Enrollment Period: The time span during which a recipient in enrolled with CenterPoint as a Medicaid Waiver eligible recipient. EPSDT: Early and Periodic Screening, Diagnosis and Treatment (EPSDT) is the federal law that says Medicaid must provide all necessary health care services to Medicaid eligible children. Even if the service is not covered under the NC Medicaid State Plan, it can be covered for recipients under 21 years of age if the service is listed at 1905 (a) of the Social Security Act. Facility: As defined in NC G.S. §122-C subsection 14, “Facility” means one location whose primary purpose is to provide services for the care, treatment, habilitation, or rehabilitation of the mentally ill, the intellectually/developmentally disabled, or substance abusers, and includes: a. An “area facility”, which is a facility that is operated by or under contract with the area authority or county program. For the purposes of this subparagraph, a contract is a contract, memorandum of understanding, or other written agreement whereby the facility agrees to provide services to one or more clients of the area authority or county program. Area facilities may also be licensable facilities in accordance with Article 2 of this Chapter. A State facility is not an area facility; b. A “Licensable facility” is a facility that provides services for one or more minors or for two or more adults. When the services offered are provided to individuals who are mentally ill or intellectually/developmentally disabled, these services shall be day services offered to the same individual for a period of three hours or more during a 24-hour period, or residential services provided for 24 consecutive hours or more. When the services offered are provided to individuals who are substance abusers, these services shall include all outpatient services, day services offered to the same individual for a period of three hours or more during a 24-hour period, or residential services provided for 24 consecutive hours or more. Facilities for individuals who are substance abusers include chemical dependency facilities; c. A “private facility”, which is a facility that is either a licensable facility or a special unit of a general hospital or a part of either in which the specific service provided is not covered under the terms of a contract with an area authority; d. The psychiatric service of the University of North Carolina Hospitals at Chapel Hill; e. A “residential facility”, which is a 24-hour facility that is not a hospital, including a group home; f. A “State facility, which is a facility that is operated by the NC Secretary of Health and Human Services; Revised 7/21/15 114 g. A “24-hour facility”, which is a facility that provides a structured living environment and services for a period of 24 consecutive hours or more and includes hospitals that are facilities under this Chapter; and h. A Veterans Administration facility or part thereof that provides services for the care, treatment, habilitation, or rehabilitation of the mentally ill, the developmentally disabled, or substance abusers. Fee-For-Service: A payment methodology that associates a unit of service with a specific reimbursement amount. Fidelity: Adherence to the guidelines as specified in evidenced-based best practices. Financial Audit: Audit generally performed by a Certified Public Accountant (CPA) in accordance with Generally Accepted Accounting Principles to obtain reasonable assurance about whether the general purpose financial statements are free of material misstatement. An audit includes examining, on test basis evidence supporting the amounts and disclosers in the financial statements. Audits also include assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall general purpose financial statement presentation. Fiscal Audit: Audit performed by the Financial Department of CenterPoint which includes a review of the Contractor’s evaluation of client’s income, client’s determined ability to pay, third party insurance verification, first and third party billing, receipts and denials. A review of COB information will also be conducted to verify support of claimed amounts submitted to CenterPoint. Fiscal Agent: An agency that processes and audits provider claims for payment and performs certain other related functions as an agent of DMA and DMH. Fraud: An intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit to himself or some other person. It includes any act that constitutes fraud under applicable Federal or State law. (Guidelines for Addressing Fraud and Abuse in Medicaid Managed Care, October 2000) GAF: Global Assessment of Functioning. Grievance: An expression of dissatisfaction about any matter other than an action, as “action” is defined in this section. The term is also used to refer to the overall system that includes grievances and appeals handled at the LME/MCO level and access to the State Fair hearing process. (Possible subjects for grievances include, but are not limited to, the quality of care or services provided, and aspects of interpersonal relationships such as rudeness of a provider or employee, or failure to respect the client’s rights). Grievance Procedure: The written procedure pursuant to which clients may express dissatisfaction with the provision of services by the LME/MCO and the methods for resolution. Revised 7/21/15 115 HIPAA: Acronym for the Health Insurance Portability and Accountability Act of 1996. Incident: An unusual occurrence as defined in APSM 30-1. Incidents are reported as Level I, II or III as defined in APSM 30-1. Initial Authorization (also called Pre-Authorization): Approved medically necessary services at a given level of care prior to services being rendered. JCAHO (Joint Commission on Accreditation of Healthcare Organizations): The national accrediting organization that evaluates and certifies hospitals and other healthcare organizations as meeting certain administrative and operational standards. Least Restrictive Environment: The least intensive/restrictive setting of care sufficient to effectively treat a client. Licensed Independent Practitioner (LIP): Licensed behavioral health professionals who may apply, be credentialed, contracted and enrolled to participate in the CenterPoint provider network. LME/MCO: Local Management Entity/Managed Care Organization (LME/MCO), a local political subdivision of the state of North Carolina as established under NC G. S. §122C. MCO Authorization: Same as Initial authorization above. MCO Authorization Request Form: The most currently approved standardized authorization request form that is used to request initial or continuing services. LOCUS: Level of Care Utilization System – A standardized tool for measuring the level of care needs for adult clients. Material Change: A material change in any written instrument is one which changes its legal meaning and effect. Medicaid Identification (MID) Card: The Medical Assistance Eligibility Certification card issued monthly to Recipients. Medicaid for Infants and Children (MIC): A program for medical assistance for children under the age of nineteen (19) whose countable income falls under a specific percentage of the Federal Poverty Limit and who are not already eligible for Medicaid in another category. Medicaid for Pregnant Women (MPW): A program for medical assistance for pregnant women whose income falls under a specified percentage of the Federal Poverty Limit and who are not already eligible in another category. Revised 7/21/15 116 Medical Assistance (Medicaid) Program: The NC Department of Health and Human Services’ Division of Medical Assistance (DMA) program to provide medical assistance to eligible citizens of the State of North Carolina, established pursuant to Chapter 58, Articles 67 and 68 of the North Carolina General Statutes and Title XIX of the Social Security Act, 42 U.S.C. 1396 et. se. Medical Record: A single complete record, maintained by the Provider of services, which documents all of the treatment, service plans and behavioral health services received by the client. Medically Necessary Services: A range of procedures or interventions that is appropriate and necessary for the diagnosis, treatment or support in response to an assessment of a client’s condition or need. “Medically necessary” services supplies refers to those services and supplies that are: 1. Provided for the diagnosis, secondary or tertiary prevention, amelioration, intervention, rehabilitation, or care and treatment of a mental health, intellectual/developmental disability or substance abuse condition, and 2. Necessary for and appropriate to the conditions, symptoms, intervention, diagnosis, or treatment of a mental health, intellectual/developmental disability or substance abuse condition, and 3. Within generally accepted standards of medical practice, and 4. Not primarily for the convenience of an client, and 5. Performed in the least costly setting and manner appropriate to treat the client’s mental health, intellectual/developmental disability or substance abuse condition. Mediation: The process of bringing individuals or agencies in conflict together with a neutral third person who assists them in reaching a mutually agreeable solution. MIS: Management Information System. Natural Resource Linking: Processes that maximize the use of family and community support systems to optimize functioning. NC Innovations Plan: A 1915(c) Home and Community-Based Wavier for Intellectual/Developmental Disabilities. Innovations “waives” institutional care; funds that could be used to serve a person in an ICFMR facility are used to serve people in the community. NC MH/DD/SAS Health Plan: A 1915(b) Medicaid Managed Care Waiver for Mental Health and Substance Abuse allowing for a waiver of freedom of choice of providers so that the MCO can determine the size and scope of the provider network. This also allows for use of Medicaid funds for alternative services. Network Provider: A provider of behavioral health services that meets the CenterPoint criteria for application, credentialing, contracting and enrollment and holds a fully executed contract to deliver services. Revised 7/21/15 117 No Reject: Provider must have a “no reject” policy in regard to clients. Providers must agree to accept all referrals meeting criteria for service provided; provider capacity to meet individual referral needs will be negotiated between CenterPoint and the provider. Non-paneled staff: Staff who provide services that are not approved for billing by the client’s third party insurer or Medicare. Out-of-Area Provider: A contracted Hospital, Agency or Licensed Independent Practitioner who provides services to a client of the LME/MCO outside of the catchment area. Out-of-Plan Services: Health care services, which the Plan is not required to provide under the terms of this Contract. The services are Medicaid-covered services reimbursed on a fee-for service basis. Out-of-Network Provider: A provider (hospital, Agency or Licensed Independent Practitioner) who has been approved under CenterPoint procedures and holds a Client-specific Agreement or Contract to deliver services to a client whose Medicaid originates in one of the catchment area counties. Such providers are not listed on the website provider search and are not offered as a choice to other CenterPoint clients. Outlier: An event that falls outside a particular range (e.g., average length of stay is significantly greater than the norm). Care Coordination Department: A CenterPoint department that provides outreach, linkage and Treatment Planning Care Management functions for Special Needs Populations. Primary Diagnosis: The most important or significant condition of an individual at any time during the course of treatment in terms of its implications for the individual’s health, medical care and need for services. Priority Populations: People with the most severe type of mental illness, severe emotional disturbances, as well as, substance abuse disorders with complicating life circumstances conditions, and /or situations which impact the person’s capacity to function, often resulting in high risk behaviors. Protected Health Information (PHI): Individually Identifiable Health Information (IIHI) that is or has been electronically transmitted by a covered entity, as well as such information when it takes any other form. Provider Council: The CenterPoint Area Providers Council (CAPC) is an independently functioning group with its own bylaws and election processes. Membership, purpose and operations are defined by a set of by-laws established by the group. Provisional Status: Status of provider agency following the occurrence of a significant event which requires state level reporting and increased monitoring of the contract status of the provider by the LME/MCO. Revised 7/21/15 118 Penetration Rate: The degree to which a defined population cohort is served. Person-Centered Planning: A process for planning and supporting the individual receiving services that builds upon the individual's capacity to engage in activities that promote community life and that honor the individual's preferences, choices and abilities. The Person-Centered Planning process involves families, friends and professionals as the individual desires or requires. The resulting treatment document is the Person-Centered Plan. Pre-Authorization (also called Initial Authorization): Approved medically necessary services at a given level of care prior to service delivery. Primary Clinician: Professional assigned after the initial intake that is ultimately responsible for implementation/coordination of the Treatment Plan/ Person-Centered Plan. Prior Authorization: The act of authorizing specific services before they are rendered. Prompt payment guidelines: State-mandated timelines the LME/MCOs must follow when adjudicating and paying claims. Provider: Any person or entity providing services under a fully executed Agreement or Contract. Provider Network: The hospitals, agencies, professional groups, or professionals under contract with the LME/MCO that meet the LME/MCO’s standards and that provide authorized, covered services to eligible and enrolled persons. QHP: Qualified Health Plan. Re-qualification: Process to assess network providers for continued participation as a CenterPoint contracted provider; re-credentialing. Qualified Professional: Any individual with appropriate training or experience as specified by the North Carolina General Statues or by rule of the North Carolina Commission on Mental Health, Developmental Disabilities, and Substance Abuse Services in the fields of mental health or intellectual/developmental disabilities or substance abuse treatment or habilitation, including physicians, psychologists, psychological associates, social workers, registered nurses and certified counselors (NC G.S. §122C-3). QIP: Quality Improvement Project. Recipient: An individual eligible for NC Medicaid; a “client”; may refer to an individual with Medicaid eligibility who is receiving behavioral health services. Reconsideration review: A review of a previous finding or decision by CenterPoint based on the provider’s Reconsideration Request and any additional materials presented by the provider; may be applicable for both providers and clients. Revised 7/21/15 119 Re-Credentialing: The review process to determine if a provider continues to meet the criteria for inclusion in the LME/MCO provider network. Routine Need - Mental Health: A condition in which the person describes signs and symptoms which are resulting in impairment and functioning of life tasks; impact the person’s ability to participate in daily living; and/or have markedly decreased the person’s quality of life. Routine Need – Substance Abuse: A condition in which the person describes signs and symptoms consequent to substance use resulting in a level of impairment which can likely be diagnosed as a substance use disorder according to the current version of the Diagnostic and Statistical Manual of Mental Disorders. SED (children with Severe Emotional Disturbances): The criteria for determining if a child has SED are: Age seventeen (17) or under Mental, behavioral, or emotional disturbance severe enough to substantially interfere with or limit the minor's role or function in family, school, or community activities Global Assessment Scale (GAS) score less than sixty (60) Service Location: Any location at which a client may obtain any covered service from a network provider. SMI (persons with Severe Mental Illness): The criteria for determining if a person has SMI are: Age eighteen (18) or older Substantial disorder of thought or mood that significantly impairs judgment, behavior, capacity to recognize reality or the ability to cope with the ordinary demands of life Global Assessment Scale (GAF) score less than or equal to fifty (50) OR One (1) or more psychiatric hospitalizations or crisis home admissions in the last year. Special Needs Population: Population cohorts defined by diagnostic, demographic and behavioral characteristics that are identified in a LME/MCO Waiver environment. The Managed Care Organization responsible for Waiver operations must identify and assure that these individuals receive appropriate assessment and services. Spend Down: Medicaid term used to indicate the dollar amount of charges a Medicaid client must incur before Medicaid coverage begins during a specified period of time. SPMI (persons with Severe and Persistent Mental Illness): The criteria for determining if a person has SPMI are: Age eighteen (18) or older Substantial disorder of thought or mood that significantly impairs judgment, behavior, capacity to recognize reality or the ability to cope with the ordinary demands of life Global Assessment Scale (GAF) score less than or equal to thirty (30), AND Revised 7/21/15 120 Three (3) or more psychiatric hospitalizations or crisis home admissions in the last year Includes all persons diagnosed with: o Bipolar Disorders 296.00-296.96 o Schizophrenia 295.20-295.90 o Major Depressive Disorders 296.20-296.36 Support Plan: A component of the Person-Centered Plan that identifies treatment needs, natural resources, and community resources that can help the client achieve personal goals and live in the least restrictive setting possible. Third-Party Billing: The process of billing an insurance company, Medicare or another “third party” agency for services rendered. Treatment Planning/Care Coordination: A managed care function aiming to assure that clients who meet Special Needs population criteria receive the necessary assessments and assistance in accessing services. CenterPoint Care Coordinators carry out this function. If the client is not already engaged with a provider, the Care Coordinator will assist in linking and engaging the client with providers that can provide the needed services and community resources that will support them. Urgent Need Mental Health: The person with this condition is not actively suicidal or homicidal; denies having a plan, the means or intent for suicide or homicide; but expresses feelings of hopelessness, helplessness or rage. Without immediate intervention, this individual’s condition could rapidly deteriorate and could potentially become actively suicidal or homicidal, or could progress to the point of needing emergent services and care. Urgent Need Substance Abuse: An individual with this condition is not imminently at risk of harming self or others or unable to adequately care for self. However, by virtue of their substance use, prompt assistance is needed to avoid further deterioration in the person’s condition, which could require emergency assistance. Utilization Review (UR): UR involves a formal review of the appropriateness and medical necessity of behavioral health services to determine if the service is appropriate and helps to achieve established goals. UR also aids in or if changes need to be made in the PCP, services and supports provided. Utilization Management (UM) Authorization – UM authorization is the process of evaluating the medical necessity, appropriateness and efficiency of behavioral healthcare services against established guidelines and criteria to assure that the client receives necessary, appropriate, high-quality care in a costeffective manner. Utilization Review (UR) Manager – A qualified professional working for the LME/MCO who reviews a client's clinical data to determine the clinical necessity of care and authorizes services associated with the plan of care. Revised 7/21/15 121