CPC_Trumbly - Healthcare Professionals
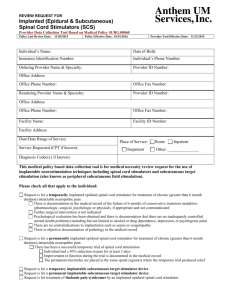
advertisement

CPC: A Paralysis Quandary for a Dime Alan Trumbly, DO Objectives Case Presentation Problem List Locate the Lesion Develop Differential Relate Differential to patient Cross fingers and choose… Patient CC: Progressive Upper Extremity Weakness. HPI: 70 y.o. Right handed, Hispanic Male. 2 weeks ago developed fever, chills, nausea, vomiting, abdominal cramping, diarrhea. Symptoms resolved in 24-36 hours. 2 Days PTA: Left upper extremity numbness, tingling, and weakness. 1Day PTA: Continued to progressively worsening, and by the PM both upper extremities involved. Transferred to S/W on day of admission for further neurological workup. Patient HPI: On day of admission Both arms quite weak. Dull aching neck pain, especially with rotation to the right. NO diploplia, ptosis, dysarthria, dysphasia, shortness of breath, lower extremity weakness, or bowel or bladder incontinence. NO pain in limbs or back. NO prior neurological history, except lumbar laminectomy for Left L4-L5 radiculopathy. Patient PMH: Hypertension Hyperlipidemia Diabetes: good blood sugar control, no neuropathy. Fam Hx: negative for neurological disease. Soc Hx: No tobacco or alcohol. Allergies: none Medications: none Patient Vitals: Afebrile PExam: Gen: pleasant, straightforward, Hispanic man, upset, but no distress, alert and oriented with no dysarthria. CN: visual fields full, pupils react 3 to 2 mm, no papilledema, ocular motility full, no nystagmus. Mild left facial weakness. Masseter and temporalis strength and bulk, as well as pterygoid strength all normal. Patient PExam: Palate elevated briskly midline. Right deviation of the tongue with protrusion. Left SCM and Trapezius were weak. Right SCM and Trapezius were normal. Motor: no fasciculations or atrophy Upper ext: Deltoids 2/5 bilaterally, Triceps 4-/5 right, and 3/5 on the left. Finger and wrist extensors 0/5 Reflexes: Absent in the upper extremities, , trace at the right knee, absent at the ankles. Plantar responses were neutral bilaterally. Patient Finger and wrist extentsors 0/5 bilaterally. Interosseous muscles 2/5 bilaterally. Hand Grips 3/5 bilaterally. ABSENT in upper extremities Triceps 4-/5 right, 3/5 left. Deltoids 2/5 bilaterally Quads 5/5 Right hip flexor 4+/5 and left 5/5 Trace at right knee Motor: Reflexes: ABSENT at ankles Foot Dorsiflexion: 4+/5 Right, and 4/5 left Patient PExam: All sensory modalities reported normal. Plantar responses neutral bilaterally. Gait: not testable. Cerebellar: not testable. Labs: 142 103 13 4.2 30 1.0 Tot Bili: 0.8 Alk Ph: 90 AST: 23 ALT: 32 Tot Prot: 7.0 Alb: 4.1 5.8 13.7 38.9 MCV: 84.4 208 Our Mission Additional studies were done upon arrival here and a diagnosis was made??? Problem List Subacute (days) Progressive Upper Extremity Weakness Absent Muscle Stretch Reflexes Rightward deviation of the tongue, and Left SCM and Trapezius were weak Recent Diarrhea Illness (2 weeks prior) Diabetes Hypertension Hx of Lumbar laminectomy FDR 32nd President Presidency spanned the Great Depression of 1930’s, and most of World War II. Only U.S. president to have served more than two terms. Location, Location, Location What are symptoms to look for? What are the locations possible? Signs that Distinguish Patterns of Weakness Sign UMN LMN Myopathic Atrophy None Severe Mild Fasciculations None Common None Tone Spastic Decreased Norm/Dec Distribution Pyramidal/regional Distal/segmental Proximal DTR Hyperactive Hypoactive/absent Normal/hypoactive Babinski Present Absent Absent Location, Location, Location Hemisphere Brainstem Cerebellum Cord AHC Root Plexus Nerve NMJ Muscle Location, Location, Location Hemisphere Brainstem Cerebellum Cord AHC Root Plexus Nerve NMJ Muscle Location, Location, Location Hemisphere Brainstem Cerebellum Cord AHC Root Plexus Nerve NMJ Muscle Location, Location, Location Hemisphere Brainstem Cerebellum Cord AHC Root Plexus Nerve NMJ Muscle FDR Founded the National Foundation for Infantile Paralysis in the US in 1938, which funded rehab programs for victims of paralytic polio and the development of the vaccine. Now known as the March of Dimes. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Myesthenia Gravis Young women and older men Diplopia, Dysarthria, Dysphagia, Dyspnea Deficits are fatigable. Pure muscular weakness without the atrophy, and normal DTR, Sensation, Mentation, and Sphincter tone. Lambert-Eaton Syndrome: Paraneoplastic, DTR absent but improve with exercise, incontinence present, and antibody mediated. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Botulism Abdominal and GI symptoms preceding syndrome that resembles myasthenia gravis. Improperly canned foods contaminated with the exotoxin of Clostridium botulinum. Rapidly developing paralysis usually affects the ocular and cranial musculature first then generalized (Descending). Toxin-mediated inhibition of acetylcholine release from axon terminals at NMJ. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Organophosphate Poisoning Miosis, Excessive bodily secretions, and fasciculations. Decreased acetylcholinesterase activity that causes excessive acetylcholine at the NMJ. Symptoms vary 5 to 12 hours after exposure. Tx with atropine. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease FDR August, 10 1921, FDR was 39 y.o. fell into Bay of Fundy, near Campobello, New Brunswick. 1933, elected President of the US with symmetrical lower extremity weakness. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Spinal Cord Disease Signs and symptoms occur at affected area and below. Associated with UMN lesions. Caused by compressive or noncompressive lesion. Central Cord Syndrome: Most often caused by syringomyelia and intramedullary cord tumors. Pathological process starts centrally and proceeds centrifugally, producing motor and sensory signs. Suspended sensory loss: decussating spinothalamic tract fibers are affected, loss of pain and temperature is bilateral, “cape distribution”>>> “sacral sparring”. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Anterior Horn Cell Disease Cell bodies of peripheral motor nerves. Amyotrophic Lateral Sclerosis: Most common, affects AHC and corticospinal tracts. Distal bilateral weakness, with atrophy and fasciculation's (LMN signs), combined with bulbar signs, hyper-reflexia, upgoing toes (UMN signs). Asymmetric limb weakness. Post-Polio Syndrome Major cause of morbidity and death throughout the world during the first half of the 20th century. Young children characterized by a mild, brief febrile illness. Small group would develop fever, HA, meningeal irritation, soreness, and asymmetric paralysis. Introduction of the inactivated polio vaccine in 1954. West Nile Virus RNA flavivirus. Majority asymptomatic, 20% develop febrile disease, and only 1% will develop neuroinvasive disease (aseptic meningitis, encephalitis, or flaccid paralysis). Abrupt onset of fever, headache, myalgia, weakness, and often, abdominal pain, nausea, vomiting, or diarrhea. Flaccid paralysis caused by WNV infection is similar clinically and pathologically to poliomyelitis caused by poliovirus, with damage of anterior horn cells. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Transverse Myelitis Inflammatory diseases of the Spinal Cord: viral, bacterial, fungal, parasitic, noninfectious. Antecedent event that precede symptoms by days to 1-2 weeks. Demyelinating and inflammatory process leading to an incomplete cord lesion initially produce a flaccid areflexic paralysis known as spinal shock, and acute UMN paralysis. Marked disturbances in autonomic function can occur below the level of the lesion. All sensory modalities are lost below the level of the lesion. Radicular pain is common at the level of the lesion. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Tick Paralysis Rocky Mountain wood tick (Dermacentor andersoni) and the American dog tick (Dermacentor varaibilis). Symptoms within 2-7 days. Bilateral Lower Extremity weakness that progresses to paralysis, ascends upward to trunk, arms, and head within hours and may lead to respiratory failure and death. Minor sensory symptoms but constitutional signs are usually absent. DTR’s are usually hypoactive or absent and opthalmoplegia and bulbar palsy can occur. Human cases are rare and usually occur in children under the age of 10. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Arsenic Poisoning Symptoms: violent GI symptoms, sense of dryness and tightness in the throat, thirst, hoarseness, and difficulty of speech. Emerald Green. Arsenicosis - chronic arsenic poisoning from drinking water, New Hampshire. Check hair follicles. Tx: Chelating agents. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Acute Intermittent Porphyria Rare metabolic disorder in the production of heme. Deficiency of the enzyme porphobilinogen deamniase leads to the metabolite porphyrin accumulating in the cytoplasm. Symptoms of AIP may include abdominal pain, constipation, and muscle weakness. Look for trigger. Acute Weakness Spinal Cord Disease: Transverse Myelitis AHC Disease Epidural and Extradural Tumor or Spinal Cord tumor Epidural Hematoma Herniated intervertebral disk Peripheral Nerve Disease: Guillain-Barre’ Syndrome Acute intermittent porphyria Arsenic poisoning Tick paralysis NMJ disease: Myasthenia gravis Botulism Organophosphate poisoning Muscle disease: Polymyositis Rhabdomyolysis-myoglobinuria Acute alcoholic myopathy Electrolyte imbalances Endocrine disease Guillain-Barré Syndrome 1859, Landry’s ascending paralysis. 1916, Guillain and Barré described the CSF findings. Acquired demyelinating disorders of the peripheral nervous system with an acute onset. Heterogeneous syndrome with several variants: Acute inflammatory demyelinating polyradiculoneuropathy (AIDP) Miller-Fisher Syndrome Acute axon loss ("axonal") polyradiculopathy Acute motor axonal neuropathy Acute motor-sensory axonal neuropathy Other variants GBS: Pathogenesis Antecedent infection evokes an immune response, this in turn cross-reacts with peripheral nerve components. (Molecular Mimicry) Results in acute polyneuropathy as the response in directed toward myelin or the axon of PN. Rabbits sensitized with C. jejuni lipooligosaccharide or GM1, would develop anti-GM1 IgG antibodies and paralysis. GBS: Clinical Features Usually begins distal legs, but 10% in arms or face. 50% will develop facial weakness and/or oropharygeal weakness. 15% develop oculomotor weakness. 80% develop parasthesias, usually mild. Often severe low back pain. 30% develop severe respiratory muscle weakness requiring ventilatory support. Dysautonomia in 70%: HR, BP, urinary retention, ileus, loss of sweating, and occasionally Sudden Death. GBS: Antecedent Events 70% of cases or 2/3’s, 1-3 weeks prior. Campylobacter jejuni: Most common, worse prognosis HIV: any stage. Other infections: CMV, EBV, Hepatitis, Mycoplasma pneumoniae, Influenza, Herpes. Vaccination: Influenza, Meningococcal (MCV4; report to VAERS). Small percentage: Surgery, Trauma, BM Transplant, TNF-alpha antagonist, and systemic illnesses. AIDP Most Common in US and Europe. 85-90% of cases. Peripheral nerve myelin is the target of immune attack. Typical clinical features: progressive, fairly symmetric muscle weakness accompanied by absent or depressed DTR. Miller-Fisher syndrome 5% of cases in US and 25% in Japan. Ophthalmoplegia, ataxia, and areflexia. And ~1/3 will have some extremity weakness. Associated with antibodies to ganglioside GQ1b in 85-90%. AMAN/AMSAN First recognized in 1986. More frequent in China, Japan, and Mexico, but still 510% of GBS in US. More severe course than demyelinating GBS; antibodies to GM1 in some cases. 60-70% preceded by Campylobacter jejuni infection. Seasonal incidence, being more frequent in the summer. AMSAN: More severe form of AMAN, pathology is predominantly axonal lesions of both motor and sensory nerve fibers. GBS: Lab features Albuminocytologic Dissociation: normal WBC with an elevated CSF Protein level. 80-90% of patients with GBS at one week after sx onset. EMG and NCS: acute polyneuropathy with predominate demylinating features in AIDP, and axonal in AMAN and AMSAN. Glycoprotein Antibodies: Anti GQ1b in 8590% of MFS. GBS: Diagnostic Criteria Required features: Progressive weakness and Areflexia. Supportive features include: Progression of symptoms over days to four weeks Relative symmetry Mild sensory symptoms or signs Cranial nerve involvement, especially bilateral facial nerve weakness Recovery starting two to four weeks after progression halts Autonomic dysfunction No fever at the onset Elevated protein in CSF with a cell count <10 mm3 Electrodiagnostic abnormalities consistent with GBS GBS doubtful: Sensory level Marked, persistent asymmetry of weakness Severe and persistent bowel and bladder dysfunction More than 50 white cells in the CSF Criteria for diagnosis of Guillain-Barre syndrome. Ann Neurol 1978; 3:565. GBS: Treatment Supportive Care: Impending Respiratory Arrest: FVC <20 mL/kg, Maximum inspiratory pressure <30 cmH2O, Maximum expiratory pressure <40 cmH2O. Prospective study of 722 GBS patients, 313 req mechanical ventilation. Predictors of intubation: Time of onset to admission less than seven days Inability to cough Inability to stand Inability to lift the elbows Inability to lift the head Liver enzyme increases Sharshar T; et.al. Crit Care Med 2003 Jan;31(1):278-83. GBS: Treatment Autonomic dysfunction: monitor BP, fluid status, and cardiac rhythm. Monitor B/B function. Pain Control: 40-50% pts have neuropathic pain. Plasma Exchange: remove circulating antibodies, complement, and other agents. IVIG : unknown, possibly anti-idiotypic antibodies interfering with T and B cells. GBS: Treatment AAN Observations: Treatment with plasma exchange or IVIG hastens recovery from GBS. The beneficial effects of plasma exchange and IVIG are equivalent. Combining the two treatments is not beneficial. Steroid treatment alone is not beneficial. Neurology 2003 Sep 23;61(6):736-40. “What was the cause of FDR’s paralytic illness?” A.S. Goldman, et. al. Journal of Medical Biography 2003; 11:232-240. 1) Protracted symmetric ascending paralysis over 10-13 days 2) Facial paralysis 3) Bladder and bowel dysfunction 4) Numbness and Dysaesthesia 5) Absence of meningismus 6) Descending pattern of recovery 7) Fever 8) Permanent paralysis Disease incidence in age group x symptom probability. Six of eight favored GBS. J Med Biogr. 11: 232–240 (2003) FINAL ANSWER Perform LP, anti GQ1b, EMG and NCS. GBS, possibly AMAN variant. References www.uptodate.com Harrisons Goetz: Textbook of Clinical Neurology, 2nd ed. Copyright © 2003 Saunders, An Imprint of Elsevier. Criteria for diagnosis of Guillain-Barre syndrome. Ann Neurol 1978; 3:565. Early predictors of mechanical ventilation in Guillain-Barre syndrome. Sharshar T; Chevret S; Bourdain F; Raphael. Crit Care Med 2003 Jan;31(1):278-83. Practice parameter: immunotherapy for Guillain-Barre syndrome: report of the Quality Standards Subcommittee of the American Academy of Neurology. Hughes RA; Wijdicks EF; Barohn R; Benson E; Cornblath DR; Hahn AF; Meythaler JM; Miller RG; Sladky JT; Stevens JC. Neurology 2003 Sep 23;61(6):736-40. Goldman, AS et al, What was the cause of Franklin Delano Roosevelt's paralytic illness?. J Med Biogr. 11: 232–240 (2003)