PNS Spinal Cord Inj
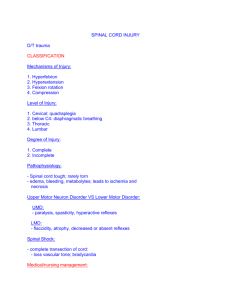
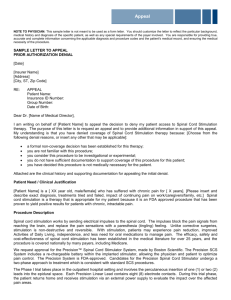
advertisement

PNS Disorders & Spinal Cord Injury Megan McClintock, MS, RN Fall 2011 – NRS 440 Trigeminal Neuralgia (tic douloureux) Dx/Treatment CT & MRI Tegretol (carbamazepine) or Trileptal (oxcarbazepine) Nerve blocks Biofeedback Glycerol rhizotomy Microvascular decompression Gamma knife Interventions Strong opiods are usually avoided Environmental management during attacks Soft-bristled, small toothbrush Foods high in protein/calories, easy to chew, lukewarm Bell’s Palsy Treatment Moist heat Gentle massage Electrical stimulation of the nerve Facial exercises Corticosteroids (prednisone) Mild analgesics Antivirals Interventions Prevention Hot, moist packs Protect the face from cold and drafts Good nutrition (chew on unaffected side) Meticulous oral hygiene Dark glasses Artificial tears Taping eyelid closed or protective shield Facial sling Gentle massage Facial exercises Guillian-Barré Syndrome Dx/Treatment • Diagnosis based on history, s/s • Supportive care • Ventilatory support in acute phase • Plasmapheresis • IV high-dose immunoglobulin (Sandoglobulin) • Nutritional support Interventions Careful assessment Prepare for intubation if vital capacity less than 800 mL Careful prevention of infection Establish a communication system early Catheterization ROM Meticulous eye care Nutrition (risk of aspiration) F&E balance Prevention of constipation Botulism Most serious type of food poisoning Thought that the neurotoxin prevents Ach from working Sx – n/v, diarrhea, abdominal cramping, afebrile, no mental deficits, decscending paralysis with cranial nerve deficits Death can occur from circulatory failure, resp paralysis, or resp complications Tx – IV botulinum antitoxin, purge of GI tract Prevention is key Nursing care is like for Guillian-Barre Tetanus (Lockjaw) Spinal Cord Injury Spinal Cord Injury Shock Spinal Shock 50% experience this Neurogenic Shock Decreased reflexes Occurs due to loss of vasomotor tone Loss of sensation Hypotension Flaccid paralysis Bradycardia All below the level of the injury Peripheral vasodilation Can last days to months Decreased cardiac output Still start active rehabilitation Usually associated with cervical or high thoracic injury Venous pooling Degree of Paralysis Degree of Paralysis Degree of Paralysis Syndromes of Spinal Cord Lesions Central Cord Syndrome Anterior Cord Syndrome Brown-Séquard Syndrome Posterior Cord Syndrome Signs/Symptoms Respiratory Above C4 have total loss of resp muscle function Below C4 can have problems with the phrenic nerve Cervical/thoracic injuries cause paralysis of abdominal/intercostal muscles Ma have a tracheostomy Neurogenic pulmonary edema Cardiovascular Above T6 decreases the activity of the SNS Bradycardia, hypotension Signs/Symptoms Urinary Urinary retention Spinal shock causes retention, atonic bladder Begin intermittent cath as soon as possible GI Above T5, problems are related to hypomobility Stress ulcers Intraabdominal bleeding (signs are masked) Below T12 and spinal shock - neurogenic bowel Signs/Symptoms Skin Potential for skin breakdown Thermoregulation Poikilothermism Decreased ability to sweat/shiver below level of injury Worse with high cervical injuries Metabolic needs Metabolic alkalosis, Na, K levels (from NG suctioning) Acidosis (from decreased tissue perfusion) High protein, high calorie diet Peripheral vascular Problems DVT & PE risk (harder to detect) Dx/Treatment CT Treat systemic and neurogenic shock If cervical injury, must maintain all body systems (pg 1552) Assess muscle groups, sensory status, brain injury, musculoskeletal injuries, internal injuries Logroll during transfers/repositioning Stabilization of injury – traction, realignment, surgery Drugs High dose methylprednisolone w/in 8 hours of injury Vasopressors (dopamine) All drugs may be metabolized differently with SCI Acute Interventions Immobilization Stabilize the neck to prevent lateral rotation Keep body correctly aligned Logroll when turning If traction is used, it must be maintained at all times Kinetic therapy bed Halo Fixation Pin Site care Skin care under vest Be able to insert 1 finger under vest Do not hold onto halo to move Weights must hang freely Don’t release traction Keep a set of wrenches close Keep sheepskin pad under vest, wash weekly Acute Interventions Respiratory Critical to assess during first 48 hrs Above C3 requires mechanical ventilation Assess carefully Chest PT Assisted coughing or incentive spirometry Acute Interventions Cardiovascular Limit vagal stimulation (turning, suctioning) Assess VS frequently Give anticholinergics (atropine) for bradycardia Give vasopressors (dopamne) for hypotension Sequential compression devices ROM and stretching exercises Prophylactic heparin (Lovenox) Watch closely for signs of hypovolemic shock Acute Interventions Fluid & Nutrition NG tube Gradually start food/fluids will bowel sounds are active or flatus is passed High protein, high calorie diet Evaluate swallowing before starting oral feeding Enteral or parenteral nutrition may be needed Creative ways to encourage eating Dietary supplements as needed Acute Interventions Bladder & Bowel Indwelling catheter Lots of fluid intake Watch for UTIs Transition to intermittent catheterization as soon as possible every 3-4 hours Bowel program Rectal stimulant followed by gentle digital stimulation Temperature Control Maintain environmental temp Don’t overload with covers or expose too long (baths) Cooling blanket for fevers Acute Interventions Stress Ulcers Usually occur 6-14 days after injury Test stool/gastric contents for blood Give steroids with antacids or food Histamine receptor blockers (Zantac, Pepcid) or proton pump inhibitors (Protonix, Prilosec) Sensory Deprivation Stimulate patient above the level of injury Prism glasses, conversation, music, smells, flavors Reflexes Explain that this is not always a return to function Antispasmodic drugs (baclofen, Dantrium, Zanaflex) Autonomic Dysreflexia Life threatening emergency!!! Massive uncompensated cardiovascular reaction caused by the SNS Occurs in response to visceral stimulation Sx – HTN (up to 300), throbbing headache, sweating above the level of the lesion, bradycardia, piloerection, flushing of skin above the level of the lesion, blurred vision/spots, nasal congestion, anxiety, nausea Tx – elevate HOB to 45 degrees or sit upright, call dr, assess for cause, cath (lidocaine jelly), ensure cath is not kinked, digital rectal exam (anesthetic ointment), remove constrictive clothing, monitor BP closely, give Procardia, teach the patient Home Care Respiratory If ventilator-dependent can still be mobile Assisted coughing, incentive spirometry Neurogenic Bladder Types – reflexic, areflexic, sensory Identify appropriate drainage method Surgical options Anticholinergic drugs, adrenergic blockers, antispasmodic drugs Avoid long-term use of indwelling catheters if possible Home Care Neurogenic Bowel High fiber diet, adequate fluid intake Suppositories (dulcolax, glycerin) or small-volume enemas with digital stimulation 20-30 minutes later Stool softener (Colace) Valsalva and manual stimulation (for lower motor neuron lesions) Time BM for 30-60 minutes after breakfast Upright position with feet flat on floor or on stepstool if possible Exercise Home Care Neurogenic Skin Twice daily comprehensive visual and tactile exam Carefully watch ischia, trochanters, heels, sacrum Reposition every 2 hours Pressure relieving cushions, special mattresses Adequate intake of protein Protection from thermal injury Use pillows to protect bony prominences In a wheelchair, lift self up and shift weight every 15-30 min Home Care Sexuality See table 61-13 (pg 1562) If upper motor neuron lesion, can have reflex sexual function If lower motor neuron lesion, may be capable of psychogenic erection (ejaculation may retrograde into bladder) Tx – drugs, vacuum devices, surgical procedures Fertility a problem with men Women have problems with lubrication Open communication is important Sexual activity may be less spontaneous May have incontinence during sexual activity Home Care Grief and Depression Can feel an overwhelming sense of loss Believe they are useless and a burden to their family May have regression Expect a wide fluctuation of emotions Table 61-14 (pg 1563) Mourning Process Counseling for caregiver and family Sympathy is not helpful, insist that care be performed Spinal Cord Tumor Rare Can be primary or secondary Can be extradural, intradural extramedullary, or intradural intramedullary Most are slow-growing and don’t cause secondary injury May have sensory and motor problems Early sx – back pain with radicular pain causing intercostal pain, angina or herpes zoster; pain worsens with activity, coughing, straining, lying down Treatment Dx with spinal xray, MRI, CT Surgical Treatment: tumor removal Radiation Therapy (may also do chemo) Compression of the cord is an emergency!!!! Give high-dose corticosteroids 1. A patient is just admitted to the hospital following a spinal cord injury at the level of T4. A priority of nursing care for the patient is monitoring for 1. 2. 3. 4. return of reflexes. bradycardia with hypoxemia. effects of sensory deprivation. fluctuations in body temperature. 2. A young adult is hospitalized after an accident that resulted in a complete transection of the spinal cord at the level of C7. The nurse informs the patient that after rehabilitation, the level of function that is most likely to occur is the ability to 1. 2. 3. 4. breathe with respiratory support. drive a vehicle with hand controls. ambulate with long-leg braces and crutches. use a powered device to handle eating utensils. 3. During assessment of a patient with a spinal cord injury at the level of T2 at the rehabilitation center, which of the following findings would concern the nurse the most? 1. 2. 3. 4. A heart rate of 92 A reddened area over the patient’s coccyx Marked perspiration on the patient’s face and arms A light inspiratory wheeze on auscultation of the lungs