Neurology
advertisement

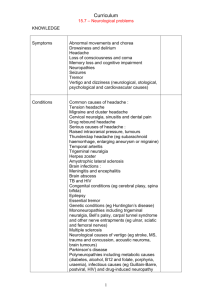
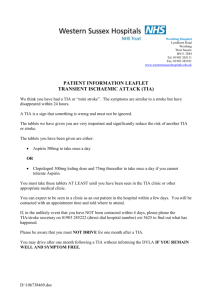
Neurology Aaqid Akram MBChB (2013) Clinical Education Fellow Objectives • Understand processes behind neurological diseases. • Understand aetiology • Progressive nature • Wider impact a neurological disease has on health Epilepsy • Seizure – Transient S/S – Abnormal electrical activity • Epilepsy – >1 unprovoked seizures (>24 hours apart) – 1 unprovoked + probability of further seizures – Epilepsy syndrome Epilepsy - Focal • Focal (Partial) – Limited to one hemisphere – Localised • Awareness = simple • Impaired awareness = focal dyscognitive – May progress to generalised (tonic-clonic) Epilepsy – Generalised • Generalised (throughout the brain) – Absence (Petit Mal) – Myoclonic – Clonic – Tonic – Tonic-clonic (Gran Mal) – Atonic Epilepsy - Causes • • • • • • • • • Vascular Idiopathic/iatrogenic Trauma Autoimmune Metabolic Infective Neoplastic Congenital Degenerative Epilepsy - Investigations • • • • • • Blood Tests – rule out other causes Imaging – CT/MRI (MRI>CT) EEG Video of seizures ECG Genetic testing Epilepsy - Management • Education + Self Management (ESN) • Provoked – After illness/surgery • Correction of electrolytes – Alcohol/substance misuse • Addiction services • Anti epileptic drug (AED) – – – – Carbamazepine Levetiracetam Lamotrigine Sodium Valproate Motor Neuron Lesions Motor Neurone Disease • Anterior horn cells of spinal cord / motor cranial nuclei • UMN/LMN signs (LMN>UMN) • ?abnormality of mitochondrial function • 2/100,000 • >50 years old • Male>female Motor Neurone Disease • Amyotrophic lateral sclerosis (ALS) – Focal onset • Limb onset: most common • Bulbar onset: appx 20% • Respiratory onset: least common – Cognitive dysfunction: 15% – Pure UMN: primary lateral sclerosis – Pure LMN : progressive muscular atrophy • Symptom treatment/NIV/Riluzole Dementia • • • • • • • Memory Loss Cognitive decline Difficulties with ADL Progressive decline No clouding of consciousness Appx 800,000 £23 billion a year Dementia • Alzeihmer’s (50%) – Cerebral degeneration, atrophy – Amyloid plaque formation – Reduced ACh production from affected neurons • Vascular (25%) – Cerebrovascular disease – Stepwise degeneration • With Lewy Body (DLB) (15%) – Abnormal protein deposition in neurons – Brain stem/neocortex • Fronto-temporal (<5%) – Protein tangles (Pick’s bodies) seen histologically • Parkinson’s Disease (PD) Cognitive Function • • • • • • • • Attention/concentration Orientation (Time/place/person) Memory (Short and long term) Praxis (getting dressed/lay a table) Language function Executive function (problem solving) Psychiatric features Cognitive impairment screen – MMSE/6CIT/GPCOG/7Minute Screen Dementia • Acetylcholinesterase Inhibitors (AChE) – Donepezil/galantamine/rivastigmine – Titrated slowly (cholinergic effects) – Alzeihmer’s / some evidence for PD • N-Methyl-D-Aspartate (NMDA) – Memantine – Moderate to severe Alzeihmer’s • Avoid antipsychotics – unless agitation/aggression – Lorazepam/haloperidol/olanzapine (PO>IM>IV) Parkinson’s Disease • Idiopathic syndrome of parkinsonism – Resting Tremor – Rigidity – Bradykinesia • Degeneration of dopaminergic pathways – Substantia nigra • Drug Induced – Block dopamine receptors/reduce storage – Tranquilisers/anti emetics (metoclopramide) Parkinson’s Disease • 50-59 years old: 17/100,000 • 70-79 years old: 93/100,000 • Exposure to: – – – – Pesticide manganese dust carbon disulphide severe CO poisoning • Born in spring • Males>females • Encephalitis Parkinson’s Disease • Tremor (4-6 Hz) – At rest + concentration – Absent during activity – Asymmetrical before generalisation • Rigidity – Increased resistance to passive movement • Bradykinesia – Slowness of voluntary movement – Reduced automatic movements – Reduced arm swing while walking • Festinated shuffling gait + unsteadiness on turning • Fixed facial expression + infrequent blinking Parkinson’s Disease • Levodopa – Honeymoon period up to 10 years – Side effects are rare • Dopamine agonists – Motor features/younger patients – More common side effects – Pramipexole / bromocriptine • Monoamine oxidase B inhibitors – Selegiline/rasagiline Parkinson’s Disease • • • • • • • COMT Inhibitors Amantadine Apomorphine (SC) Pallidotomy Thalamic Subthalamic Deep Brain Stimulation Parkinson’s Disease • Depression/anxiety – TCA/SSRI • Dementia – AChE Inhibitors • Compulsive behaviours – Dopamine agonists may cause development of • Pathological gambling • Compulsive eating/shopping • Hallucinations/Psychosis – Clozapine • Acute akinesia (Parkinson’s Crisis) – Infection/surgery/GI disease Parkinson’s Disease • Multiple System Atrophy – – – – Appears as parkinsonism initially Rapid progression Inability to look down voluntarily Autonomic dysfunction (urogenital, postural hypotension) • Progressive supranuclear palsy – Paresis of conjugate gaze – Problems looking up and down voluntarily – Dysphagia and dysphasia. Multiple Sclerosis • Cell mediated autoimmune – Repeated episodes of inflammation – Loss of insulating myelin sheath – Sclerosis in these areas – Slowing or blocking of signal transmission • Relapsing Remitting (RR)(80%) • Secondary progressive (50% from RR) • Primary progressive (15%) Multiple Sclerosis • • • • • • • Distance from equator Females>males 40-50 years old Genetic predisposition - +ve FHx Reduced relapses in pregnancy] Clinical diagnosis + supporting MRI Revised McDonald Criteria Multiple Sclerosis • Relapses – Methylprednisolone – Azathioprine may reduce relapses and progression • Disease modifying therapy – Interferon Beta/Glatiramer – Dimethyl fumarate/Teriflunomide/Alemtuzumab • Second line – Natalizumab/Fingolimod/Mitoxzantrone • Other – Cannabinoids – Percutaneous venoplasty • Symptom specific medication TIA/Stroke • Disruption of blood supply to brain • Rapidly developing disturbance of cerebral function • > 24 hours = stroke • <24 hours = TIA • Infarction(Ischaemic) (70%) • Haemorrhage (Intracranial) (15) • SAH (5%) Brain Anatomy TIA/Stroke • • • • • Hypertension Smoking DM Heart Disease Peripheral vascular disease • Previous TIA/stroke • Polycythaemia vera • Carotid artery occlusion • COCP • Hyperlipidaemia • Clotting disorders • Alcohol TIA/Stroke • FAST • Cerebral (50%) [TACS/PACS] – – – – Contralateral hemiplegia (flaccid spastic) Contralateral sensory loss Homonymous hemianopia Higher cerebral dysfunction (dysphasia/visiospatial disorder) • Cerebellar/Brainstem (25%) [POCS] – Quadraplegia/locked in syndrome/gaze disturbances • Lacunar (25%) [LACS] – Basal ganglia/internal capsule/thalamus/pons – Pure motor/pure sensory/mixed/ataxia TIA: Risk of Stroke • • • • • A = Age > 60years old B = Blood pressure > 140/90 C = clinical features (1) (1) – Unilateral weakness – Speech disturbance only (2) (1) D = duration – >60 minutes – 10-59 minutes (2) (1) D = Diabetes (1) >3 – Aspirin 300mg daily (likely reduced to 75mg after assessment) – Specialist assessment + investigation within 24 hours – Secondary prevention Stroke Rehabilitation • • • • • • • • Specialist Stroke Unit Vision Memory Emotion Swallowing Communication Motor Function Pain Management Long term effects • • • • • • ADL Progression + Fear of progression DVLA Mood – altered personality? Independence/Reliance Institutionalisation DVLA • Seizure – 1st episode • 6 months off driving • high risk = 12 months – Mulitple • Must be seizure free for 5 years +/- medication • Chronic Neurological Disorders – Unable to drive • Impairment of coordination • Impairment of muscle power – require medical assessment suggesting driving performance not impaired (1-3 year licence) DVLA • TIA – Single • Cannot drive for 1 month – Multiple over short period • Notify DVLA • 3 months free from further attacks • Stroke – Cannot drive for 1 month • If driving performance not impaired – If deficit >1 month • Notify DVLA • Cannot drive until driving performance not impaired Objectives Were: • Understand processes behind neurological diseases. • Understand aetiology • Progressive nature • Wider impact a neurological disease has on health