PPT
advertisement

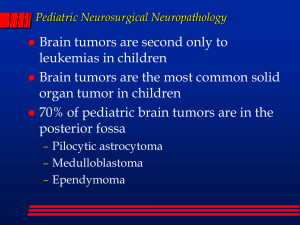
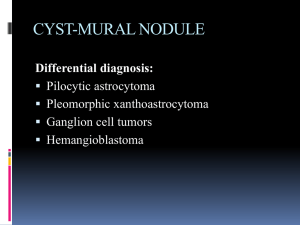
C.Hydrocephalus ex vacuo - Refers to dilation of the ventricular system with a compensatory increase in CSF volume secondary to a loss of brain parenchyma, as may occur after a. infarcts or b. with a degenerative disease. C. Herniation - Intracranial pressure may increase by focal expanding lesion or generalized edema.. - Because the cranial vault is subdivided by rigid dural folds (falx and tentorium), a focal expansion of the brain causes it to be displaced in relation to these partitions - If the expansion is sufficiently severe, herniation will occur - Herniations are named by . a. Either the part of the brain that is displaced or b. The structure across which it moves. - The usual consequence of such displacement is compromise of the blood supply to the "pushed" tissue, resulting in infarction. - This often leads to another round of swelling and further herniation. - Types of herniations: 1. Subfalcine (cingulate) herniation - Expansion of a mass in the frontal or parietal lobe will eventually result in herniation of ipsilateral cingulate gyrus under the free edge of the falx to produce selective displacement of the pericallosal arteries away from the lesion and from the midline - This may compromise circulation through the pericallosal arteries ( branches of anterior cerebral artery) and result in infarction of the parietal parasaggital cortex , manifesting clinically as a weakness or sensory loss in one or both legs 2. Tentorial (uncal) or uncinate gyrus herniationAny supratentorial expanding hemispheric mass may produce herniation of the ipsilateral uncus (tip and medial part of parahippocampal gyrus)and medial part of the parahippocampal gyrus medially and downwards through the tentorial incisura - This occurs most frequently when the mass is located in the temporal lobe - Consequences of temporal lobe displacement: Uncal herniation A. The ipsilateral oculomotor nerve compressed between the free edge of the tentorium and the posterior cerebral artery 1. At first the oculomotor nerve is flattened , and compressed 2. Later, there will be hemorrhage in the oculomotor nerve, and the resulting paralysis of the nerve produces ptosis and dilation of the pupil ipsilateral to the lesion - Dilation of the pupil is the earliest consistent sign of tentorial herniation and may occur before there is any loss of consciousness B. Compression of the cerebral peduncle (crus cerebri)on the side of the mass lesion by direct pressure from the herniating brain will result in contralateral limb weakness C. The posterior cerebral artery may also be compressed, resulting in ischemic injury to the territory supplied by that vessel, including the primary visual cortex. D. When the extent of herniation is large enough the contralateral cerebral peduncle may be compressed against the edge of the tentorium and this may lead to its nfarction in the this results in n hemiparesis ipsilateral to the side of the herniation NOTE: - Because hemispheric lesions typically cause contralateral weakness, this ipsilateral hemiparesis can be a false localizing sign that would suggest to the examiner that the patient has a lesion in the opposite, unaffected hemisphere E. Duret hemorrhages . - Progression of tentorial herniation is often accompanied by hemorrhagic lesions in the in the tegmentum of the midbrain and the tegmental parts of the pons but not in the medulla - Are linear or flame-shaped lesions - The most likely mechanism of hemorrhage is stretching and tearing of the central perforating branches of the basilar artery that supply the rostral brainstem leading to infarction or hemorrhage - The presence of Duret hemorrhages implies a grim prognosis Durett hemorrhage 3. Central transtentorial hernion - Occur in cases of : a. Expanding frontal and parietal lesions b. or bilateral chronic subdural hematoma c. or diffuse brain swelling • Both parahipocampal gyri will herniate . 4.Tonsillar herniation (foramen impaction, cerebellar cone) - Refers to displacement of the cerebellar tonsils through the foramen magnum. - It occurs as an early complication of expanding masses in the posterior cranial fossa but may also occur with supratentorial space-occupying lesion - The pathognomonic indication of this herniation is hemorrhagic necrosis at the tips of the cerebellar tonsils and a groove on the ventral surface of the medulla where it is compressed against the anterior border of foramen magnum - This pattern of herniation is life-threatening Tonsillar herniation III. CNS Tumors - About half to three-quarters are primary tumors, and the rest are metastatic. - Tumors of the CNS make up a larger proportion of cancers of childhood, accounting for as many of 20% of all tumors. - CNS tumors in childhood differ from those in adults both in histologic subtype and location. - In childhood, tumors are likely to arise in the posterior fossa, while in adults they are mostly supratentorial. - Tumors of the nervous system have unique characteristics that set them apart from neoplastic processes elsewhere in the body. a.These tumors do not have detectable premalignant or in situ stages comparable to those of carcinomas b.Even low grade tumors may infiltrate large regions of the brain, thereby leading to serious clinical deficits and poor prognosis , non-resectability, and poor prognosis. c.The anatomic site of the neoplasm can influence outcome independent of histologic classification due to local effects a. A benign meningiomas may cause cardio respiratory arrest from compression of the medulla b. Brain glioma may be non- resectable - Even the most highly malignant gliomas rarely spread outside the CNS - Some tumors may infiltrate the subarachnoid space - Medulloblastoma may spread to distant sites I. Gliomas - Gliomas are tumors of the brain parenchyma that are classified the basis of their resemblance to different types of glial cells. - The major types of tumora in this category are: A. Astrocytomas, B. Oligodendrogliomas, C.Ependymomas A. Astrocytoma : - Several different categories of astrocytic tumors are recognized, the most common being:1.Diffuse ( infiltrative) 2.Pilocytic astrocytomas. 1. Diffuse Astrocytoma : - Account for about 80% of adult primary brain tumors. - Most frequent in the fourth through sixth decades. - Usually are found in the cerebral hemispheres - The most common presenting signs and symptoms are: a. Seizures, b. Headaches c. Focal neurologic deficits related to the anatomic site of involvement - They show a spectrum of histologic differentiation that correlates with clinical course and outcome - On the basis of histologic features, they are divided into three groups a.Well-differentiated astrocytomas(WHO grade II/IV: - Symptoms can be static or progress only slowly during a number of years but at some point progress - The mean survival is more than 5 years. - Eventually, patients suffer rapid clinical deterioration . - These tumors are poorly defined, infiltrative tumors that expand and distort invaded brain without forming a mass Microscopic appearance: a. A mild to moderate increase in the number of astrocytic nuclei with mild nuclear pleomorphism b. An intervening GFAP-positive astrocytic cell processes that give the background a fibrillary appearance c. The transition between neoplastic and normal tissue is indistinct, d. Tumor cells can be seen infiltrating normal tissue at some distance from the main lesion. b. 1. 2. 3. Anaplastic astrocytomas (WHO GRADE III)show: Regions that are more densely cellular The cells have greater nuclear pleomorphism Increased mitoses are often observed (The most important feature). AnaplasticAstrocytoma Astrocytoma(WHO grade III) Anaplastic (WHO grade III) c. Glioblastoma (WHO grade IV) - It has a histologic appearance similar to anaplastic astrocytoma with the additional features of: a. Pseudopalisading necrosis b. and /or b. Microvasular proliferation Note - Glioblastomas have abnormal vessels that are "leaky" and will show contrast enhancement with imaging studies • Glioblatomas are either: 1. Primary - The patients develop it from the start - Is the most common type of glioblastoma 2. Secondary - Progress from lower grades Note : Once the histologic features of glioblastoma appear, the prognosis is very poor; with treatment( resection , radiotherapy , and chemotherapy), the median survival is only 15 months Glioblastoma (WHO grade IV) Glioblastoma • Genetic Changes in astrocytomas 1. In low grade astrocytomas(grade II) - Mutations that alter the enzymatic activity of two isoforms of the metabolic enzyme isocitrate dehydrogenases(IDH1 and IDH2)and this genetic change differentiates this tumor from gliosis and pilocytic astrocytoma 2. In glioblastomas - Loss of function mutation in p53 and Rb tumor suppressor pathway 2. Pilocytic astrocytomas WHO grade I Are relatively benign tumors Typically occur in children and young adults Are usually located in the cerebellum Other locations: a. Floor and walls of the third ventricle, b. The optic pathways(called optic glioma) c. Spinal cord and occasionally the cerebral hemispheres. • Note: Infatile pilocytic astrocytoma is called pilomyxoid astrocytoma and it is grade II typically located in the hypothalamus Morphology of pilocytic astrocytoma Gross: - Well circumscribed - Is often cystic, with a mural nodule in the wall of the cyst Microscopically, the tumor is composed of a. Hypercellular areas composed of bipolar astrocytes with with long, thin "hairlike " processes that are GFAP positive b. Hypocellular areas formed of microcysts. c. Rosenthal fibers d. Eosinophilic granular bodies, e. Necrosis and mitoses are absent. • Genetically Pilocytic astrocytomas don’t show mutations in IDH1 and IDH2 Pilocytic astrocytoma Pilocytic astrocytoma - Tumors that appear on MRI as cyst containing a nodule are: a. Pilocytic astrocytoma b. Ganglioglioma c. Pleomorphic Xantho astrocytoma QUIZ 2 • What is the nucleus that is located beneath the anterior commissure in the basal forebrain and rich in acetylcholine