PediatricTumors
advertisement

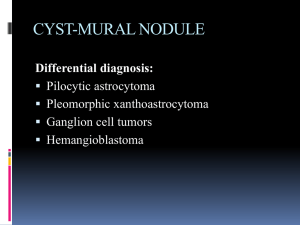
Pediatric Neurosurgical Neuropathology Brain tumors are second only to leukemias in children Brain tumors are the most common solid organ tumor in children 70% of pediatric brain tumors are in the posterior fossa – Pilocytic astrocytoma – Medulloblastoma – Ependymoma CNS tumors: pediatric vs. adult Adults: 70% of tumors are supratentorial – meningioma – pituitary adenoma – High grade astrocytoma » Anaplastic astrocytoma (grade III) » Glioblastoma multiforme (grade IV astrocytoma) Pediatric: 70% in posterior fossa – pilocytic astrocytoma (cerebellar astrocytoma) – medulloblastoma Brain tumors: intro Intracranial neoplasms – Primary – Secondary » Metastatic » Local invasion Tumors of the spinal cord Primary brain tumors: intro Primary brain tumors are rare – 2.5% of all cancer deaths – Second most common type of tumor in children – There are over 100 different brain tumors Most common types – Astrocytomas (adults and children) » Grades I-IV – Medulloblastomas (in children) » also known as: primitive neuroectodermal tumor-PNET – Meningiomas (adults) – Pituitary adenomas (adults) Clinical presentation Clinical symptoms depend upon: – Age, location, and type of tumor and grade Symptoms may include: – Increased intracranial pressure » secondary to obstruction of CSF at aqueduct » hydrocephalus (infants), headache, papilledema, vomiting – – – – seizures focal neurological deficits hormonal changes (pituitary adenoma) visual changes (diplopia, field defects) » Pituitary adenoma - pressure on optic chiasm CNS tumors: diagnosis Symptoms prompt neuroimaging CT and MRI – intra-axial vs. extra-axial – Location of tumor – contrast enhancement » typical of high grade » also in some low grade, i.e., pilocytic astrocytomas CNS tumors: location Extra-axial – meningiomas Cerebral hemispheres – grade II-III astrocytomas, GBM Crossing corpus callosum - GBM optic nerve - pilocytic astrocytoma – (in Neurofibromatosis Type 1) Sella - Pituitary adenoma Peri-III ventricle - Pilocytic astrocytoma, GBM CNS tumors: location posterior fossa (in children) – pilocytic astrocytoma – medulloblastoma brainstem (pons) – pontine glioma (astrocytoma) spinal cord – low-grade astrocytomas (grade I and II) Pilocytic astrocytomas – Most common in children – Grade I astrocytoma – Cerebellum (posterior fossa), optic nerve » Thalamic, spinal cord, cerebral – – – – Discrete, well circumscribed mass Often with associated cystic area Contrast enhancing Histologic appearance: » Biphasic: piloid cells and microcystic areas » Rosenthal fibers » no mitoses Pilocytic astrocytomas Rosenthal fibers biphasic Piloid cells cyst Tumor of cerebellum, often with cyst, biphasic, Rosenthal fibers, piloid cells (enlongated bipolar) Astrocytoma - high grade Astrocytoma grade II and III are very, very rare in the pediatric population Grade IV - glioblastoma multiforme – Most common astrocytoma in adults – Only about 10% of astrocytomas in children Diffusely infiltrating tumor of cerebral hemispheres Contrast enhancing tumor Histological appearance: – – – – Densely cellular, with marked nuclear pleomorphism Numerous mitoses Endothelial proliferation Necrosis with pseudopallisading Glioblastoma (grade IV) Less common in children than adults, typical pathology (necrosis with pseudopallisading) Pontine glioma Diffuse expansion of pons, usually high grade astrocytoma (III-IV) Medulloblastomas PNET of posterior fossa in children Histologic appearance: – – – – – – Densely cellular “small blue cell tumor” Numerous mitoses Apoptotic (karyorrhectic) cells Endothelial proliferation Necrosis neuronal or glial differentiation » Homer Wright rosettes » GFAP positive cells Medulloblastoma Mass arising in roof of fourth ventricle Homer Wright rosettes Ependymoma Mass arising in floor of fourth ventricle Perivascular pseudorosettes Meningiomas Discrete non-invasive tumor – Extra-axial, pushes into brain – Attached to dura – Hyperostosis or invasion of skull common Histologic appearance: – Fibroblastic or menigothelial cells – Meningothelial whorls – Psammoma bodies Rare in children, may be intraventricular (lateral ventricles) Meningiomas Extra-axial tumor, meningothelial cells, whorls and psammoma bodies Ganglioglioma Cerebrum, cervicomedullary, often with cystic component Increased numbers of neurons (some binucleate) and increased glial cells (usually astrocytic) Craniopharyngioma Heterogeneous, cystic mass in suprasellar region Basiloid layer, stellate reticulum, “wet” keratin, often calcified Choroid plexus papilloma Lateral ventricle in children (fourth ventricle in adults) Germ cell tumors Germinoma Teratoma Pineal - 99% males, most are germinomas Suprasellar - often mixed germ cell tumor, 50% female Teratomas are rare Metastatic tumors The most common “brain” tumor in adults is metastatic Metastatic tumors are rare in children The most common metastatic tumor in children is osteosarcoma Local extension of malignant tumors of vertebral bodies (Ewing’s sarcoma) or paravertebral soft tissues (neuroblastoma) are not uncommon Other tumors Subependymal giant cell astrocytoma (SEGA) – Intraventricular tumor in Tuberous sclerosis Desmoplastic infantile ganglioglioma (DIG) – Superficial cerebral tumor in infants Dysembryoplastic neuroepithelial tumor (DNET) – Hamartomatous lesion associated with seizures Atypical teratoid rhabdoid tumor (ATR, AT/RT) – Infants, posterior fossa, very malignant Eosinophilic granuloma – A type of Langerhans cell histiocytosis – Single discrete osteolytic lesion in skull Meningioangiomatosis – Hamartomatous superficial cerebral lesion associated with seizures Hereditary syndromes Neurofibromatosis type I – – – – – Café-au-lait spots Dermatofibromas, multiple optic nerve astrocytomas, bilateral plexiform neurofibroma Malignant peripheral nerve sheath tumor Neurofibromatosis type II – bilateral acoustic neuroma – multiple meningiomas – ependymomas